Last Updated on November 27, 2025 by Bilal Hasdemir
Coronary artery disease (CAD) is a big problem worldwide. Knowing the different types of CAD is key to treating it well. At Liv Hospital, we focus on giving top-notch care to patients from around the globe.
Coronary artery disease affects the heart’s blood supply. This article will cover the three main types of CAD. We’ll also share real-life examples to show how CAD can affect health over time.
Teaching patients about their health is very important. By learning about CAD and its types, patients can make better choices for their care.
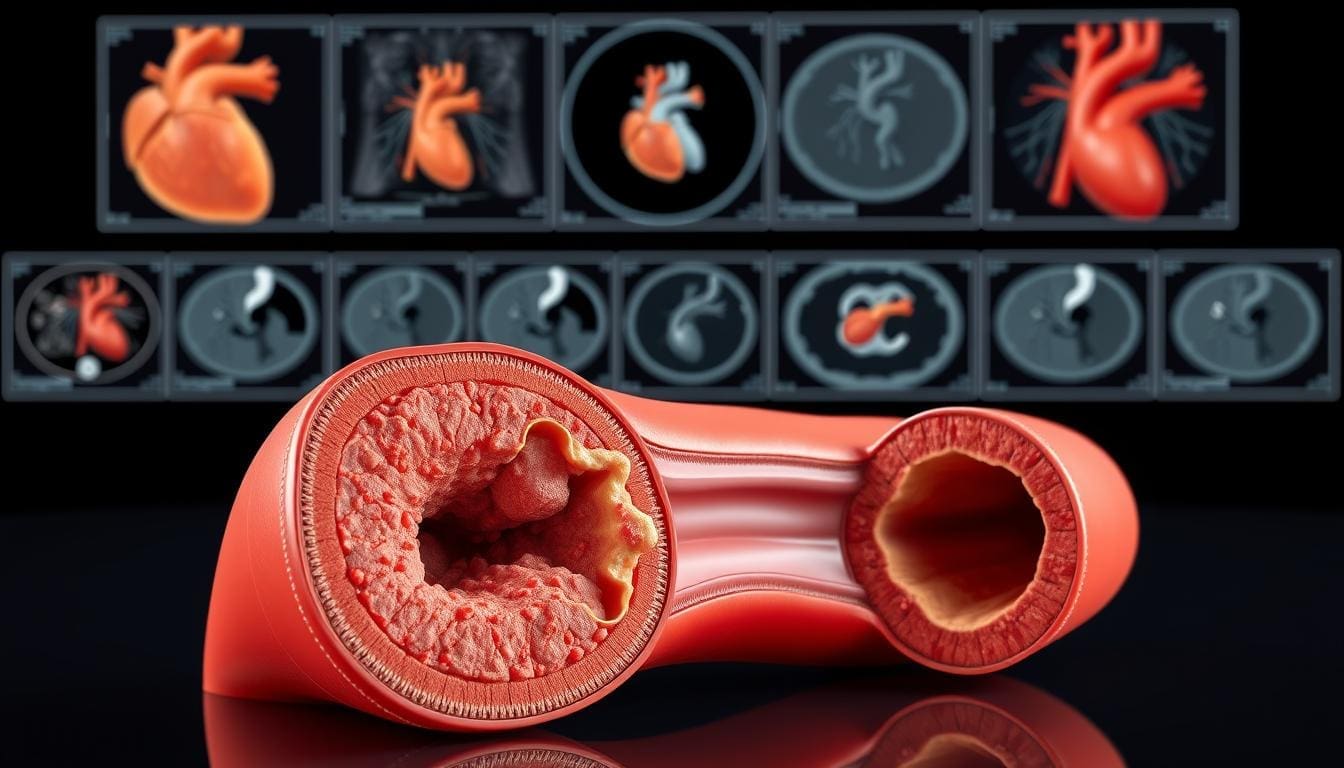
Coronary Artery Disease (CAD) is when the coronary arteries get worse because of atherosclerosis. This can cause serious health problems. CAD is when the coronary arteries get narrowed or blocked, which stops blood from reaching the heart.
CAD happens when plaque builds up in the coronary arteries. This makes them narrow or block completely. It’s a type of heart disease that can really affect someone’s life and how long they live.
As plaque grows, it cuts down blood flow to the heart. This can cause chest pain, known as angina. Or, it can lead to a heart attack if the blood flow stops completely.
“Coronary Artery Disease is when the coronary arteries get narrowed or blocked because of atherosclerosis,” says doctors. This shows why keeping the coronary arteries healthy is so important to avoid heart problems.
CAD is a big reason for deaths worldwide. The World Health Organization (WHO) says heart diseases, including CAD, are the top cause of death globally. CAD affects millions of people every year.
CAD is a big health problem worldwide. Knowing what CAD is and how it affects the heart can help people take steps to avoid it. This means eating right, exercising, and managing stress to lower CAD risk.
Seeing CAD as a serious heart disease helps us understand why we need to act fast. We should get medical help and make lifestyle changes. This includes eating well, staying active, and handling stress to avoid CAD.
The atherosclerotic process starts with plaque building up in the coronary arteries. This can lead to heart problems. Atherosclerosis is when plaque buildup makes the arterial walls hard and narrow.
Damage to the inner layer of the coronary artery often causes this. High blood pressure, smoking, or high cholesterol are common culprits. As the artery wall heals, it gets inflamed, and plaque starts to form.
Over time, this plaque grows. It can narrow the artery and limit blood flow to the heart.
Plaque forms from cholesterol, fat, and calcium on the inner walls of coronary arteries. A bad diet, not exercising, and genetics can make it worse.
As plaque builds up, it narrows the artery. This is called stenosis. It reduces blood flow to the heart muscle, causing chest pain or angina.
More plaque buildup can cause significant arterial narrowing or even blockage. A blocked artery can damage the heart muscle below it. This can lead to a myocardial infarction or heart attack.
The shift from narrowing to blockage can happen suddenly or slowly. Sometimes, a piece of plaque can rupture. This causes a blood clot to form, suddenly blocking the artery. Knowing how atherosclerosis works is key to preventing and managing coronary artery disease.
Coronary artery disease is not just one thing. It’s a range of conditions, including obstructive, nonobstructive, and SCAD. Knowing these types helps us understand how CAD affects people differently.
The main types of coronary artery disease are based on how they affect the heart. Obstructive coronary artery disease has big blockages in the arteries, usually from atherosclerosis. Nonobstructive coronary artery disease has issues that don’t block the arteries much. Spontaneous coronary artery dissection (SCAD) is when the artery wall tears on its own.
Each type of CAD has its own signs and symptoms. Obstructive CAD often shows up with heart pain or a heart attack. Nonobstructive CAD might cause similar symptoms but without big blockages. SCAD is rare and usually affects younger women without usual risk factors, leading to sudden heart problems.
Doctors need to know these differences to treat each type of CAD better. This helps improve how well patients do.
We look into obstructive coronary artery disease, a serious issue where plaque blocks the coronary arteries. It’s a top cause of heart problems and deaths around the world. Often, it leads to heart attacks and other serious heart issues.
Obstructive coronary artery disease narrows the coronary arteries due to plaque buildup. This makes it hard for blood to reach the heart muscle. It can cause symptoms like angina.
The disease’s cause involves a mix of lipid metabolism, inflammation, and cell growth in the artery walls. Over time, this buildup can severely reduce blood flow through the artery.
Several factors lead to the narrowing of arteries in obstructive CAD. These include:
Knowing these factors is key to finding effective treatments for obstructive CAD.
The main symptom of obstructive CAD is angina pectoris. It’s chest pain or discomfort from temporary heart muscle ischemia. People often describe it as a squeezing or pressure feeling in the chest.
“Angina is a warning sign that the heart is not getting enough oxygen-rich blood. It’s a signal that you should seek medical attention.”
— American Heart Association
Other signs include shortness of breath, feeling tired, and irregular heartbeats. Spotting these symptoms early is vital for quick action.
| Symptom | Description |
|---|---|
| Angina Pectoris | Chest pain or discomfort due to myocardial ischemia |
| Shortness of Breath | Difficulty breathing, potentially indicating heart failure |
| Fatigue | Unusual tiredness or lack of energy |
Obstructive CAD can show up in many ways, from stable angina to serious heart attacks. It’s key for doctors to know these types to treat them right.
Stable angina is a common sign of obstructive CAD. It’s chest pain or discomfort that happens when you’re active or stressed. The pain usually goes away with rest or medicine.
A 55-year-old man with high blood pressure and high cholesterol feels tightness in his chest when he walks uphill. It goes away after a few minutes of rest.
The American Heart Association says, “Stable angina means the heart muscle doesn’t get enough blood and oxygen because of blocked arteries.”
“This condition is often predictable and can be managed with lifestyle changes and medication.”
Unstable angina is a more serious and unpredictable form of obstructive CAD. It’s chest pain or discomfort that happens at rest, is new, or gets worse. It’s a medical emergency because it can lead to a heart attack.
Myocardial infarction, or heart attack, happens when the heart doesn’t get enough blood. Symptoms include severe chest pain, shortness of breath, and feeling lightheaded. Quick medical help is vital to reduce damage.
A 65-year-old diabetic man went to the emergency room with sudden chest pain that spread to his left arm. He also felt nauseous and sweaty. His ECG showed ST-segment elevation, and his troponin levels were high, proving he had a heart attack.
Nonobstructive coronary artery disease (CAD) is a condition where the coronary arteries don’t have big blockages. Yet, people with it feel symptoms like those with big blockages. We’ll dive into this condition, covering its definition, how it works, and the differences between functional and structural issues.
Nonobstructive CAD has functional or structural problems in the coronary arteries without big blockages. This can cause less blood to reach the heart muscle, leading to symptoms like chest pain.
The reasons behind nonobstructive CAD include:
These factors make diagnosing nonobstructive CAD tricky. They don’t always show up on standard tests.
In nonobstructive CAD, both functional and structural problems are key. Functional issues are about how the arteries work, like during spasms. Structural issues are about changes in the artery walls.
| Abnormality Type | Description | Clinical Impact |
|---|---|---|
| Functional | Issues with coronary artery function, e.g., vasospasm | Can cause transient ischemia and chest pain |
| Structural | Changes in arterial wall composition or architecture | May lead to long-term reduction in blood flow |
The symptoms of nonobstructive CAD can look a lot like those of obstructive CAD. This makes it hard to tell them apart. People might feel angina, shortness of breath, or other symptoms usually linked to big blockages.
“The clinical presentation of nonobstructive CAD can be just as debilitating as obstructive CAD, requiring a thorough diagnostic approach to manage effectively.”
Expert Opinion
It’s important for doctors to understand nonobstructive CAD well. They need to look at both functional and structural problems when diagnosing and treating it.
Nonobstructive coronary artery disease (CAD) is a complex challenge. It shows up in different ways that need careful understanding. We will look at examples that show how nonobstructive CAD can appear, like coronary vasospasm, microvascular dysfunction, and vessel wall problems.
Coronary vasospasm is when the coronary arteries suddenly narrow. This can cause heart muscle to not get enough blood. Clinical signs include chest pain when you’re not active, and sometimes a change in the ECG. A study in Nature shows how important it is to spot coronary vasospasm as a cause of heart attacks.
“Coronary vasospasm is a serious issue that can look like blockages in the arteries,” say heart doctors. They stress the need to be very careful when diagnosing it.
Microvascular dysfunction is when the small arteries in the heart don’t work right. This can cause chest pain and other symptoms like blockages. People with this often have chest pain when they’re active, even if their arteries look fine on tests. Doctors use special tests to find out if this is what’s happening.
A review says, “Microvascular dysfunction is a big reason for ongoing chest pain in people with nonobstructive CAD. It needs a detailed diagnosis.”
Vessel wall problems in nonobstructive CAD include things like widened arteries or inflammation around the arteries. These can be seen with advanced imaging like CCTA. These issues can cause symptoms like chest pain. A study found, “Spotting vessel wall problems is key to understanding nonobstructive CAD and figuring out how to treat it.”
Understanding SCAD is key to diagnosing and treating patients with sudden heart attacks. SCAD is when the coronary artery wall tears, leading to heart attacks.
SCAD’s unique pathology is a tear in the coronary artery’s inner layer. This allows blood to enter the artery wall, creating a false lumen. It can block the artery, reducing blood flow.
The exact cause of SCAD is not known. But it’s thought to be due to hormones, genetics, and vascular issues.
SCAD mainly affects younger women without typical heart disease risk factors. Research shows SCAD patients are mostly female, aged mid-40s to early 50s.
Factors increasing SCAD risk include hormones, pregnancy, and certain tissue disorders.
SCAD can cause acute coronary events like unstable angina, heart attacks, and sudden death. Its symptoms can be similar to those of blocked arteries, making diagnosis hard.
“SCAD is an important cause of myocardial infarction in young women, and its recognition is critical for proper management.” –
A recent study on SCAD
Quickly recognizing and treating SCAD is vital to avoid lasting heart damage.
Diagnosing coronary disease involves both non-invasive and invasive methods. We use various techniques to find out the type and how severe coronary artery disease (CAD) is.
Non-invasive tests are often the first step in checking for coronary disease. These include:
These tests are key for the first check-up. They help decide if more detailed tests are needed.
For those with suspected or confirmed CAD, coronary angiography is used. It gives a detailed look at the coronary arteries. This procedure involves:
Coronary angiography lets us see exactly where and how bad the coronary disease is. It helps decide on treatments like angioplasty or CABG.
By using both non-invasive and invasive tests, we can accurately diagnose and treat coronary disease. This improves patient care.
We treat CAD differently based on its type. This includes obstructive, nonobstructive, and SCAD. Each type has its own treatment because CAD can vary a lot.
For obstructive CAD, we use lifestyle changes, medicines, and sometimes surgery. Lifestyle changes include eating better, exercising more, and quitting smoking. We also use medicines like beta-blockers and statins to help symptoms and slow the disease.
When lifestyle changes and medicines don’t work, we might need surgery. Invasive procedures like angioplasty or CABG are used. Angioplasty and stenting help open blocked arteries, while CABG bypasses them.
Nonobstructive CAD needs a special treatment plan. We focus on managing symptoms and finding the cause. Medicines like nitrates and calcium channel blockers help with angina. We also recommend lifestyle changes.
We also treat related conditions like high blood pressure and diabetes. Sometimes, coronary vasospasm is a problem. Calcium channel blockers can help with this.
SCAD treatment is very personal. Conservative management is often the first step. This includes watching closely and using medicine to manage symptoms.
In severe cases, we might need surgery like PCI or CABG. But we’re careful because SCAD patients can face more risks.
In summary, treating CAD, whether it’s obstructive, nonobstructive, or SCAD, needs a plan that fits each patient’s needs.
Stopping Coronary Artery Disease (CAD) from getting worse is key to better health and fewer heart problems. We can do this by making lifestyle changes and using medical treatments. This helps those with CAD live better lives.
Making lifestyle changes is important to stop CAD from getting worse. Eating right is a big part of it. We should eat more fruits, veggies, whole grains, and lean meats.
Also, exercising regularly is a must. Try to do at least 150 minutes of moderate exercise or 75 minutes of hard exercise each week.
Quitting smoking is also very important for CAD patients. Smoking makes the disease worse. Stress management, like meditation or yoga, can also help keep your heart healthy.
Medical care is just as important in stopping CAD from getting worse. Doctors use medicines like statins, beta-blockers, and antiplatelet agents. These help control high cholesterol, high blood pressure, and blood clots.
It’s also important to keep an eye on CAD risk factors. This lets doctors make changes to treatment plans as needed. Sometimes, doctors may need to do procedures to get blood flowing to the heart again.
By using both lifestyle changes and medical care, we can stop CAD from getting worse. This approach needs effort from both doctors and patients. It’s a team effort for better health.
Understanding coronary artery disease (CAD) is key to managing and preventing it. We’ve looked at the different types of CAD, like obstructive, nonobstructive, and spontaneous coronary artery dissection (SCAD). Each type has its own signs, diagnosis, and treatment.
Obstructive CAD causes big blockages in arteries, leading to symptoms like angina. Nonobstructive CAD might cause similar symptoms but without big blockages. SCAD is a rare but serious condition where the artery wall tears.
Managing CAD well needs a full plan. This includes changing lifestyle, using medicine, and sometimes surgery. Knowing the CAD type helps doctors create the best treatment for each patient.
Preventing CAD is also very important. Healthy habits and managing risks can greatly reduce the chance of getting CAD.
As cardiology advances, it’s vital for patients and doctors to keep up with new CAD management and prevention info. Together, we can improve life for those with CAD.
Coronary artery disease (CAD) is when the coronary arteries narrow or block. This happens because of plaque buildup. It affects blood flow to the heart.
The main types of coronary artery disease are obstructive CAD, nonobstructive CAD, and spontaneous coronary artery dissection (SCAD).
Obstructive CAD means the coronary arteries are narrowed or blocked. This is usually because of plaque buildup. It can reduce blood flow to the heart.
Nonobstructive CAD is when the coronary arteries are not narrowed much. But they might have problems that affect heart health.
SCAD is when there’s a tear in the inner layer of the coronary artery. This causes blood to build up between the layers. It can lead to sudden heart problems.
Doctors use many ways to diagnose CAD. They include stress tests, echocardiograms, and coronary angiography.
Treatment for obstructive CAD includes lifestyle changes and medicines. Procedures like angioplasty or coronary artery bypass grafting might also be needed.
Managing nonobstructive CAD focuses on treating underlying issues. This includes using medicines and making lifestyle changes.
SCAD treatment often involves careful monitoring and medicines. In some cases, more invasive treatments might be needed.
To prevent CAD from getting worse, adopt healthy habits. This includes eating well, exercising, not smoking, and managing health conditions. Medical care is also important.
To manage CAD, make healthy lifestyle choices. This includes eating right, staying active, managing stress, and avoiding tobacco.
Yes, there are medical strategies for CAD. These include medicines to control symptoms and manage risk factors. Regular check-ups are also key.
“Syndrome of Non-Obstructive Coronary Artery Diseases” — PMC article, describes INOCA/ANOCA etc.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8754003/ (PubMed Central)
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!