Last Updated on December 3, 2025 by Bilal Hasdemir
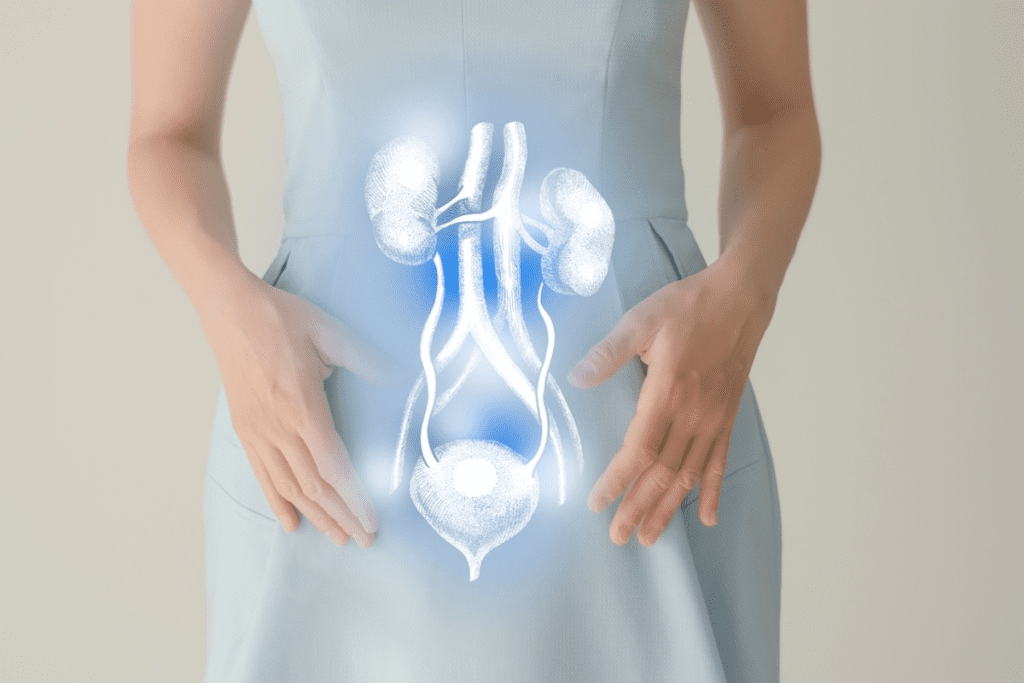
Urethral stricture is a condition where the urethra gets narrower due to scar tissue. This can cause problems with urination, making life harder for those affected.
Finding the right treatment depends on many things. These include how long and where the stricture is, how complex it is, and the patient’s overall health. Knowing what causes and symptoms of urethral stricture are important for choosing the best treatment.
There are a few ways to treat urethral stricture. These include urethroplasty, urethral dilation, and urethrotomy. Each method has its own benefits and is right for different patients.
Key Takeaways
- The best treatment for urethral stricture depends on the stricture’s characteristics and patient factors.
- Urethral stricture is a narrowing of the urethra caused by scar tissue.
- Treatment options include urethroplasty, urethral dilation, and urethrotomy.
- Understanding the stricture’s length, location, and complexity is key for the best treatment.
- Patient-specific factors are important in choosing the most effective treatment.
Understanding Urethral Strictures and Their Impact
A urethral stricture is when the urethra gets narrower. This can cause big problems with urinating. It happens when scar tissue or inflammation blocks the normal flow of urine.
Definition and Causes of Urethral Strictures
Urethral stricture disease means the urethra gets narrower. There are different reasons for this:
- Idiopathic: Unknown causes, which are rare.
- Iatrogenic: Caused by medical procedures, like catheterization or surgery.
- Inflammatory: Caused by infections or inflammation.
- Traumatic: Due to injuries to the urethra.
Knowing the cause helps doctors choose the right treatment.
Symptoms and Diagnosis
The symptoms of urethral stricture vary but often include:
- Weak urinary stream
- Straining to void
- Incomplete emptying of the bladder
- Urinary tract infections (UTIs)
To diagnose urethral stricture, doctors use:
- Clinical evaluation, including medical history and physical examination.
- Uroflowmetry to check urine flow rate.
- Imaging studies, like retrograde urethrography or ultrasound, to see the urethra and measure the stricture.

Understanding urethral strictures helps doctors give better care. This improves patients’ lives and outcomes.
Key Factors That Determine the Optimal Urethral Stricture Treatment
Choosing the right treatment for urethral stricture depends on several key factors. We look at many things to decide the best course of action. This helps ensure the treatment works well.
Stricture Length and Location Considerations
The length and where the stricture is located are very important. Stricture length matters a lot because longer ones need more complex treatments. Shorter ones might just need urethral dilation or urethrotomy.
The location of the stricture also affects treatment. Strictures in the bulbar urethra are easier to treat than those in the penile urethra. Knowing exactly where it is helps us choose the right treatment.
Complexity and Previous Treatments
The complexity of the stricture and whether it’s come back before affects treatment. We check if it’s primary or recurrent and any previous treatments. If it’s come back or failed before, we might need to try something different.
- What treatments have been tried before can guide our next steps.
- Complications like spongiofibrosis can also shape our treatment plan.
- For complex cases, we might need to use a mix of treatments or do things in stages.
Patient-Specific Factors
Each patient’s health, age, and what they prefer also matter a lot. We look at the patient’s medical history and any concurrent health conditions. These can affect what treatment is best.
- Age and health can make some treatments better than others.
- What the patient prefers and their lifestyle also play a part in choosing treatment.
- Other urological issues can also influence the treatment plan.
By carefully looking at these factors, we can create a treatment plan that meets each patient’s needs. This helps improve their quality of life and treatment outcomes.
Minimally Invasive Procedures for Urethral Strictures
Minimally invasive treatments have changed how we treat urethral strictures. They offer effective solutions with fewer side effects. These methods help restore urine flow, easing symptoms and improving life quality.

Balloon Dilation Technique and Outcomes
Balloon dilation is a common treatment for urethral strictures. It uses a balloon catheter to widen the narrowed urethra. The procedure is guided by fluoroscopy for precise placement. Urethral dilation can greatly relieve symptoms, but its effectiveness varies by stricture type.
The results of balloon dilation are often good, mainly for shorter strictures. But, success rates drop for longer or more complex strictures. We often start with balloon dilation because it’s less invasive and has a quick recovery.
Direct Vision Internal Urethrotomy (DVIU)
Direct Vision Internal Urethrotomy (DVIU) is another key procedure for urethral strictures. It uses an endoscope and a cold knife or laser to widen the urethra. This method is done under direct vision for precise control.
DVIU is best for short, bulbar urethral strictures. It has high success rates for the right patients, but there’s a risk of recurrence. The choice between DVIU and other treatments depends on several factors, including stricture length and patient health.
Comparative Success Rates for Different Stricture Types
Success rates for urethral stricture treatments vary by stricture type. Shorter strictures do better with balloon dilation and DVIU than longer ones.
When comparing treatments, we look at stricture length, location, and complicating factors like spongiofibrosis. Choosing the right treatment for each patient is key to success. This approach improves quality of life and reduces the need for more invasive treatments.
Advanced Drug-Coated Balloon Technologies
Advanced drug-coated balloon technologies are changing how we treat urethral strictures. These new methods are leading to better treatment results.
Drug-coated balloons, like those with paclitaxel, are showing great promise. They have success rates over 90% in some studies. This is a big leap forward from older treatments.
Paclitaxel-Coated Balloons for Anterior Strictures
Paclitaxel-coated balloons are a top choice for treating anterior urethral strictures. Paclitaxel stops cells from growing back, which helps prevent strictures from coming back.
The advantages of paclitaxel-coated balloons include:
- High success rates in treating anterior urethral strictures
- Minimally invasive procedure, reducing recovery time
- Effective in reducing stricture recurrence
Recent studies show a big drop in stricture recurrence with paclitaxel-coated balloons. For example, a study on PMC shows their effectiveness in treating urethral strictures.
As we keep improving drug-coated balloon technology, we’ll see even better results for urethral stricture patients. Using these technologies in clinics is a big step towards better, less invasive treatments.
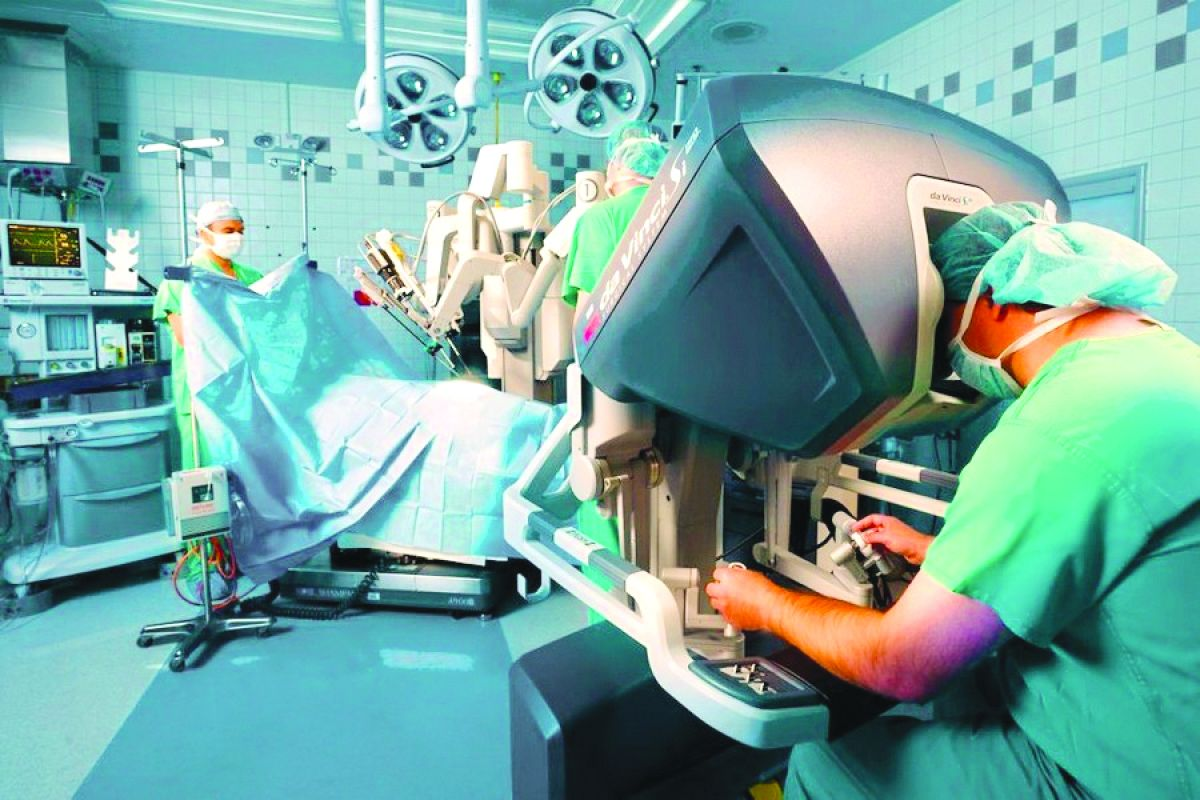
Urethroplasty Options for Complex and Recurrent Strictures
For those with complex and recurrent urethral strictures, urethroplasty is a top choice. This surgery rebuilds the urethra to better urine flow and ease symptoms.
Oral Mucosa Graft Urethroplasty (OMGU) is a leading technique. It uses a graft from the mouth to fix the stricture. This method is popular for its success and lasting results.
Oral Mucosa Graft Urethroplasty (OMGU)
OMGU shines for complex and recurring strictures. It starts with taking a graft from the mouth. This graft then widens the narrowed urethra, improving flow.
The oral mucosa’s rich blood supply aids in healing and lowers complication risks. Plus, it’s taken from a hidden area, reducing scarring.
Recovery Process and Long-Term Success Rates
Recovery after OMGU includes catheter use to heal the graft. Close monitoring during this time is key. Long-term, many see big improvements in symptoms and life quality.
Research backs urethroplasty, like OMGU, for lasting results on complex and recurring strictures. The success comes from careful surgery and the use of oral mucosa grafts.
In summary, urethroplasty, mainly OMGU, is a top treatment for complex and recurring urethral strictures. Knowing about the procedure, recovery, and outcomes helps patients choose wisely.
Conclusion: Making an Informed Decision About Stricture Treatment
Understanding urethral stricture is key to effective treatment. It affects quality of life, causing weak urine flow and pain. These are common symptoms of urethral stricture disease.
Choosing the right treatment depends on several factors. These include the stricture’s length, location, and the patient’s health. We’ve looked at various treatments, from simple procedures to complex surgeries.
Patients can make better choices by knowing about urethral stricture icd10. New treatments like drug-coated balloons and oral mucosa graft urethroplasty offer hope for complex cases.
Getting a treatment plan that fits you is essential. We suggest talking to healthcare experts. They can help find the best treatment for your needs.
FAQ
What is a urethral stricture?
A urethral stricture occurs when the urethra gets narrower. This can make it hard to urinate. It can happen for many reasons, like accidents during medical procedures, infections, or injuries.
What are the symptoms of a urethral stricture?
Symptoms can differ from person to person. But common signs include a weak urine flow, feeling like you have to strain to pee, and taking a long time to pee. Doctors use tests to figure out if you have this problem.
How is a urethral stricture diagnosed?
Doctors use a few ways to find out if you have a urethral stricture. They might do tests like uroflowmetry and imaging studies. These help them see how bad the stricture is and where it is.
What are the treatment options for urethral stricture?
There are a few ways to treat urethral stricture. Doctors might use procedures like balloon dilation or Direct Vision Internal Urethrotomy (DVIU). Sometimes, surgery like urethroplasty is needed.
What is urethroplasty, and when is it recommended?
Urethroplasty is a surgery to fix the urethra. It uses a graft or flap to rebuild it. It’s usually recommended for serious or recurring cases. It has a good success rate.
What is the success rate of paclitaxel-coated balloons in treating urethral stricture?
Paclitaxel-coated balloons work well for treating some types of urethral stricture. They are a good option for many patients.
How do I determine the best treatment for my urethral stricture?
Finding the right treatment depends on several things. These include how long and where the stricture is, how complex it is, and your personal health. Talking to a doctor is the best way to figure this out.
What is the recovery process like after urethroplasty?
After urethroplasty, you’ll likely need a catheter for a while. Then, you can slowly start doing normal things again. How well you do after surgery can vary, but it’s usually good.
Can urethral stricture be treated with minimally invasive procedures?
Yes, you can treat urethral stricture with less invasive methods. These include balloon dilation and DVIU. The choice depends on the stricture’s details and your health.
References
- American Urological Association. (2016). Urethral Stricture: AUA Guideline. Retrieved from https://www.auanet.org/guidelines-and-quality/guidelines/urethral-stricture-guideline