Last Updated on November 25, 2025 by Ugurkan Demir

Urinary incontinence is a big health issue affecting millions globally. It’s more common than many think, hitting over 60 percent of adult women in the U.S. This problem can make you lose confidence and affect your life quality. But, there are effective treatment options available. Beyond urine pills, explore 5 effective solutions for treating urinary incontinence, including medications and behavioral changes.
At Liv Hospital, we know how important it is to tackle urinary incontinence with full care. Our team combines the latest medical knowledge with support focused on you. We help you take back control and confidence with personalized incontinence solutions.
We will look at five effective ways to treat urinary incontinence. This will give you the info you need to choose the best care for yourself.
Key Takeaways
- Urinary incontinence is a treatable condition, not an inevitable part of aging.
- Effective treatment options are available to improve quality of life.
- Liv Hospital offers full care tailored to your needs.
- Five effective solutions will be discussed to address urinary incontinence.
- Seeking medical attention is the first step towards regaining confidence and control.
Understanding Urinary Incontinence: A Common but Treatable Condition

Learning about urinary incontinence is the first step to better bladder health. This condition means urine leaks out without control. It happens to people of all ages, but more often as they get older.
What Causes Urinary Incontinence?
Many things can cause urinary incontinence. Short-term causes include infections, pregnancy, and some medicines. Long-term causes include overactive bladder, diabetes, and multiple sclerosis.
Other factors like weak pelvic muscles, neurological disorders, and lifestyle choices also play a role. Knowing the causes helps find the right treatment.
Who is at Risk?
Some people are more likely to have urinary incontinence. Pregnant women, older adults, and those with certain health issues are at higher risk. This includes people with neurological disorders or chronic diseases.
| Risk Factor | Description |
| Pregnancy | Weakened pelvic muscles during pregnancy can lead to incontinence. |
| Age | Incontinence prevalence increases with age due to weakened muscles and other age-related changes. |
| Neurological Disorders | Conditions like multiple sclerosis and Parkinson’s disease can affect bladder control. |
By knowing the causes and risks of urinary incontinence, people can find the right medical help and make lifestyle changes. This helps manage their condition well.
Types of Urinary Incontinence You Should Know

It’s important to know about the different types of urinary incontinence. This condition is not just one thing. It includes several types, each with its own causes and symptoms.
Stress Incontinence
Stress incontinence happens when moving or pressure on the bladder makes you leak urine. It often happens when you cough, sneeze, laugh, or exercise. It’s usually because the muscles in your pelvic area are weak or the urethral sphincter is not working right.
A medical expert says, “Stress incontinence is common, affecting many, mostly women after childbirth or during menopause.”
“The key to managing stress incontinence lies in strengthening the pelvic floor muscles through exercises like Kegels.”
Urge Incontinence
Urge incontinence, also known as overactive bladder, is when you suddenly feel a strong need to pee and then can’t hold it. Your bladder muscles are too active or go off at the wrong times.
This condition can really disrupt your life. “Urge incontinence can significantly impact daily life, making it essential to seek medical advice for proper management.”
Mixed Incontinence
Mixed incontinence is when you have symptoms of both stress and urge incontinence. This makes it harder to diagnose and treat.
Managing mixed incontinence needs a detailed plan. “A tailored treatment plan is essential, combining lifestyle changes, exercises, and possibly medication.”
Overflow Incontinence
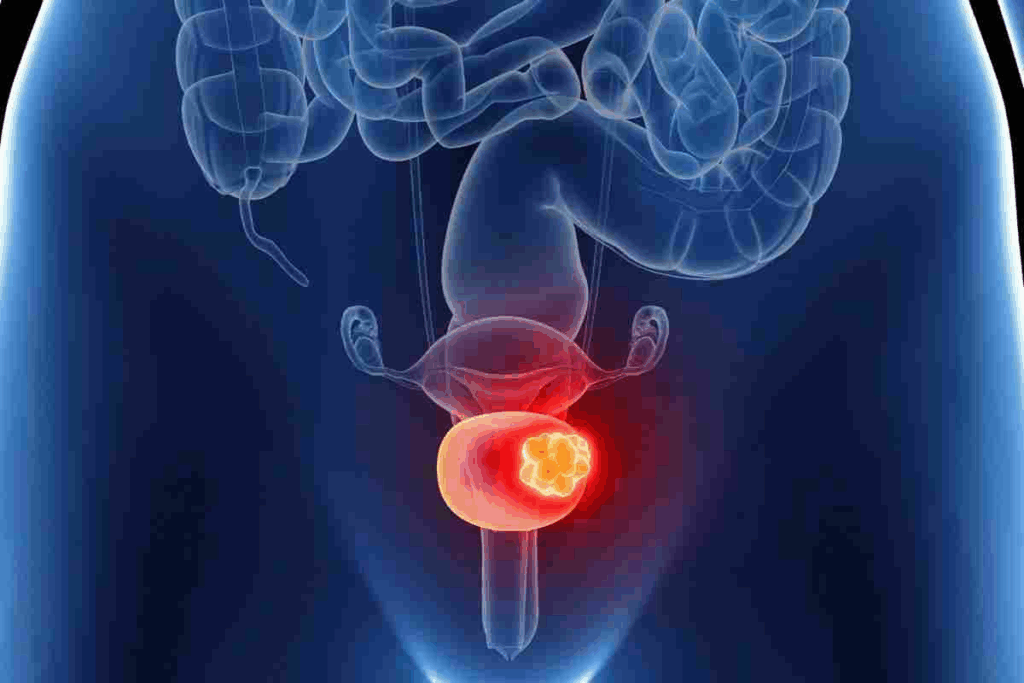
Overflow incontinence is when your bladder doesn’t empty fully, causing constant or frequent dribbling. It’s often due to bladder blockage, weak bladder muscles, or nerve damage.
A specialist notes, “Overflow incontinence can stem from many issues, like prostate enlargement in men or nerve damage from diabetes.”
Knowing the different types of urinary incontinence is key to finding the right treatment. Each type needs a specific approach. Identifying the correct type is vital for effective management.
Solution 1: Lifestyle Modifications for Better Bladder Control
Lifestyle changes are key in managing urinary incontinence. They offer a first step in fighting this common issue. By changing our daily habits, we can greatly improve bladder control and lessen incontinence symptoms.
Dietary Changes That Reduce Incontinence
Some foods can help with urinary incontinence. Staying away from caffeine, alcohol, and spicy foods can lessen bladder irritation. Eating foods high in fiber helps prevent constipation, which can make incontinence worse.
Keeping a food diary can help find out which foods trigger incontinence. By making smart food choices, we can manage our condition better.
Weight Management and Exercise Benefits
Keeping a healthy weight is vital for bladder control. Extra weight can put more pressure on the bladder and pelvic muscles, making symptoms worse. Regular exercise helps manage weight and strengthens bladder-supporting muscles.
Exercises like Kegels target the muscles that control the bladder. They improve muscle strength and coordination. Combining weight control with these exercises can reduce incontinence and boost bladder health.
Solution 2: Pelvic Floor Exercises – The Natural Approach
Pelvic floor exercises are a key part in fighting urinary incontinence. They are a natural and effective way to help. Kegel exercises focus on the muscles that hold the bladder and urethra in place. This helps control the bladder and cuts down on leaks.
How to Perform Kegel Exercises Correctly
To do Kegel exercises right, first find the pelvic floor muscles. You can do this by stopping your urine flow midstream. This shows you’re using the right muscles.
Then, squeeze these muscles for a few seconds and then relax them.
Step-by-Step Guide:
- Contract the pelvic floor muscles for 5 seconds.
- Release the muscles for 5 seconds.
- Repeat this cycle 10-15 times per session.
- Aim for at least three sessions a day.
Creating an Effective Pelvic Floor Training Routine
Being consistent with pelvic floor exercises is important. Having a routine and sticking to it makes a big difference. Adding Kegel exercises to other pelvic floor training, like biofeedback, can help even more.
Tips for an Effective Routine:
- Start with manageable sessions and gradually increase duration and frequency.
- Combine Kegel exercises with other pelvic floor strengthening activities.
- Monitor progress and adjust the routine as necessary.
Adding pelvic floor exercises to your daily routine can help manage urinary incontinence naturally and effectively.
Solution 3: Bladder Training Techniques
Bladder training is a key method for treating urinary incontinence. It involves slowly increasing the time between trips to the bathroom. This helps people control their bladder better, making incontinence less frequent and severe.
Scheduled Voiding: How It Works
Scheduled voiding means going to the bathroom at set times, even if you don’t feel like it. It helps create a routine and can greatly improve bladder control. Start with going every two hours and increase the time as you get better.
Benefits of Scheduled Voiding:
- Improves bladder capacity
- Reduces frequency of incontinence episodes
- Enhances overall bladder control
Urge Suppression Strategies
Urge suppression helps manage sudden urges to urinate. When you feel the urge, use strategies like deep breathing or distraction to delay going. This way, you can make it to the bathroom without an accident.
“The key to successful bladder training is consistency and patience.”
“Bladder training is a behavioral therapy that can significantly improve urinary incontinence symptoms by gradually increasing the bladder’s capacity and improving the patient’s ability to suppress urgency.”
Let’s look at how bladder training works:
| Technique | Description | Benefits |
| Scheduled Voiding | Urinating at fixed intervals | Improves bladder capacity, reduces incontinence episodes |
| Urge Suppression | Managing sudden urges to urinate | Enhances bladder control, reduces frequency of accidents |
Adding bladder training to your daily routine can greatly improve urinary incontinence symptoms. It’s important to be consistent and patient. The benefits of bladder training take time to show.
Solution 4: Urine Pills and Medications for Incontinence Management
Several medications are available to treat urinary incontinence. These can help manage symptoms. They work best when used with lifestyle changes and pelvic floor exercises.
Antimuscarinic Medications for Overactive Bladder
Antimuscarinic medications are often used for overactive bladder. They relax the bladder muscle. This increases bladder capacity and reduces incontinence episodes.
Examples include oxybutynin and tolterodine. But, they can cause dry mouth and constipation.
Beta-3 Adrenergic Agonists
Beta-3 adrenergic agonists, like mirabegron, treat overactive bladder. They increase bladder capacity. This allows it to hold more urine.
They have fewer side effects than antimuscarinics. But, they can cause high blood pressure.
Alpha-Blockers for Men with Prostate Issues
Alpha-blockers help men with urinary incontinence due to prostate issues. They relax prostate and bladder neck muscles. This makes urination easier.
They can improve urinary flow and reduce overflow incontinence.
Topical Estrogen for Women
Topical estrogen is recommended for women with urinary incontinence. It’s often used when incontinence is linked to vaginal dryness. Estrogen creams or pessaries can improve bladder control.
It’s important to talk to a healthcare provider about medication and treatment. Each person’s needs are different. Professional advice is key to finding the right medication.
Solution 5: Advanced Medical Interventions
When simple treatments for urinary incontinence don’t work, advanced medical options can help. These are for people who haven’t seen improvement with lifestyle changes, exercises, or medicines.
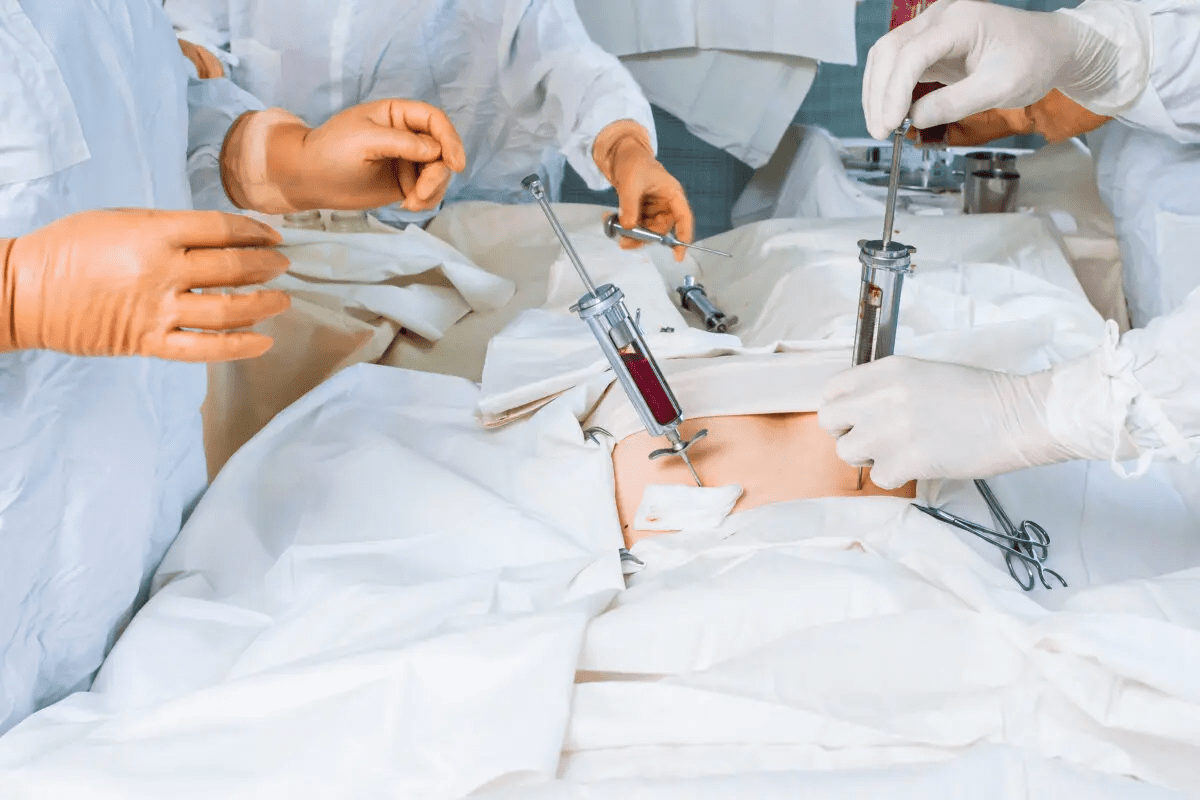
Minimally Invasive Procedures
Minimally invasive treatments have changed how we treat urinary incontinence. They aim to be less invasive, cutting down on recovery time and risks. Botox injections are used to relax the bladder muscle, helping those with an overactive bladder.
Bulking agents are also used. They are injected around the urethra to help it close better and stop leaks. These treatments are often done as an outpatient and show great promise in managing incontinence.
Surgical Options When Other Treatments Fail
For some, surgery is needed when other treatments don’t work. Sling surgery is a common choice. It involves placing a supportive sling under the urethra to improve its stability and prevent leaks. This surgery works well for stress urinary incontinence.
Other surgeries include colposuspension and artificial urinary sphincter implantation. Colposuspension lifts the bladder neck to improve continence. The artificial urinary sphincter provides a mechanical way to control urine flow. These surgeries are considered when incontinence greatly affects a person’s quality of life.
It’s important to talk to a healthcare provider to find the best advanced medical treatment. This will depend on your specific needs and medical history.
Alternative Medicine for Urinary Incontinence
Many people are looking at alternative medicine to help with urinary incontinence. This includes practices not part of regular medical care but can work alongside it.
We’ll look at some alternative methods that might help with urinary incontinence. These include herbal remedies, acupuncture, traditional Chinese medicine, and biofeedback therapy.
Herbal Remedies and Supplements
Some herbal remedies and supplements might help with urinary incontinence. For example, cranberry supplements are sometimes suggested. But, it’s important to talk to a doctor before trying them, as they can affect other medicines.
- Cranberry supplements: May help reduce urinary tract infections, which can contribute to incontinence.
- Saw palmetto: Some studies suggest it may help with urinary symptoms, though more research is needed.
- Ginkgo biloba: May improve bladder control, but evidence is limited.
Acupuncture and Traditional Chinese Medicine
Acupuncture is a part of traditional Chinese medicine. It involves putting thin needles into certain body points. It’s thought to help balance the body and improve functions like bladder control. Some studies show it can help with urinary incontinence, best when used with other treatments.
Traditional Chinese medicine also uses herbal formulas made just for you. These can be complex and need a licensed practitioner to use.
Biofeedback Therapy
Biofeedback therapy helps you learn about your body’s functions, like bladder muscle tension. By knowing these, you can control them better. This might help reduce urinary incontinence symptoms.
Biofeedback uses special equipment to show you how your bladder works. With a therapist’s help, you can learn exercises to improve bladder control.
In summary, alternative medicine offers many ways to manage urinary incontinence. While they can be helpful, always talk to a doctor before starting any new treatments. This ensures they’re right for you.
Managing Nocturia: Treatments for Nighttime Urination
Managing nocturia well needs lifestyle changes and sometimes medical help. Nocturia, or needing to pee a lot at night, can mess up sleep and health.
Lifestyle Adjustments for Reducing Nighttime Bathroom Trips
Changing your lifestyle can cut down on nighttime bathroom visits. Fluid management is key; drinking less before bed helps a lot. Also, avoid caffeine and alcohol in the evening to reduce trips to the bathroom.
Another good change is elevating the legs during the day. This helps prevent fluid buildup that can lead to needing to pee at night. These simple steps can really help manage the condition.
Medical Approaches to Nocturia
If lifestyle changes don’t work, medical help might be needed. Medications like desmopressin can reduce urine at night. Treatments for underlying issues like overactive bladder or sleep problems are also available.
In some cases, treating underlying health issues like diabetes or heart failure can help too. It’s important to work with a healthcare provider to find the best treatment.
By mixing lifestyle changes with medical treatments, people can manage nocturia better. This improves their overall quality of life.
Practical Daily Management: Products and Strategies
Managing urinary incontinence means picking the right products and planning daily activities with confidence. We’ll look at how to pick the best products and stay active despite incontinence challenges.
Choosing the Right Absorbent Products
Absorbent products are key for managing urinary incontinence. The market has many options, like adult diapers, pads, and protective underwear. These are designed for comfort, protection, and to keep things discreet.
When picking absorbent products, consider a few things:
- Absorbency Level: Pick products that fit your incontinence level. More absorbent ones are for more severe cases.
- Comfort: Look for breathable materials and a comfy fit to avoid skin irritation.
- Discretion: Choose products that look like regular underwear to feel more confident.
- Odor Control: Products with odor control can make you feel more comfortable and confident.
| Product Type | Absorbency Level | Comfort Features |
| Adult Diapers | High | Breathable materials, adjustable tabs |
| Protective Underwear | Medium to High | Stretchy waistband, moisture-wicking fabric |
| Pads | Low to Medium | Adhesive strips, ultra-thin design |
A healthcare professional notes, “The right absorbent product can greatly improve life for those with urinary incontinence. It provides protection and confidence.”
“The key to managing urinary incontinence is finding the right balance between protection, comfort, and lifestyle.”
Medical Expert, Urologist
Maintaining Social Activities and Travel
Urinary incontinence shouldn’t stop you from enjoying social activities or traveling. With some planning, you can keep doing what you love and explore new places.
To keep up with social activities and travel, try these strategies:
- Plan Ahead: Look up restrooms and facilities at your destination. Knowing where to find them can help reduce anxiety.
- Pack Essentials: Carry a kit with absorbent products, wipes, and a spare set of clothes.
- Stay Confident: Wear clothes that make you feel confident and comfortable.
By choosing the right absorbent products and using practical strategies, people with urinary incontinence can live active and fulfilling lives.
When to Seek Professional Help for Urinary Incontinence
It’s important to know when you need professional help for urinary incontinence. This condition can really affect your life. While some cases can be managed by changing your lifestyle, others might need medical help.
Warning Signs That Require Medical Attention
Some symptoms and changes mean you should see a doctor. These include:
- Sudden onset of symptoms: If your urinary habits or leakage change suddenly, see a healthcare professional.
- Severe leakage: If you leak a lot of urine or it happens often, it might be a sign of a bigger issue.
- Pain or discomfort: Feeling pain or discomfort while urinating or in your pelvic area means you should get medical help.
- Blood in urine: Seeing blood in your urine is a sign that needs immediate medical attention.
- Failed conservative management: If changing your lifestyle and doing pelvic floor exercises don’t help, it’s time to see a doctor.
What to Expect During a Medical Evaluation
When you visit a healthcare professional, they will do a thorough check-up. This includes:
- Medical history: They will look at your medical history to find any underlying conditions that might be causing your incontinence.
- Physical examination: A physical exam, possibly including a pelvic exam, will be done to check your overall health and find any physical causes.
- Diagnostic tests: You might have tests like urinalysis, ultrasound, or urodynamic tests to find out what’s causing your incontinence.
- Treatment options discussion: Based on what they find, your healthcare provider will talk about different treatment options with you. These can range from medications and lifestyle changes to surgery.
Getting professional help is a big step towards managing urinary incontinence well. Knowing the warning signs and what to expect at a medical evaluation helps you take charge of your bladder health. This can greatly improve your quality of life.
Conclusion: Taking Control of Your Bladder Health
Understanding urinary incontinence and its treatments can help you manage your bladder health. We’ve looked at many ways to deal with it, like changing your lifestyle and doing pelvic floor exercises. We’ve also talked about medications and more serious treatments.
Good treatment for a weak bladder means tackling the root cause. Making diet changes, losing weight, and doing pelvic floor exercises can really help. These steps can make a big difference in your bladder health.
It’s important to take charge of your bladder health. If you’re having trouble with incontinence, don’t hesitate to get help. With the right care, you can feel more confident and live a fuller life.
FAQ
What are the most effective treatments for urinary incontinence?
To treat urinary incontinence, try lifestyle changes and pelvic floor exercises. Bladder training and medications can also help. For severe cases, there are minimally invasive procedures and surgery.
What causes urinary incontinence?
Incontinence can come from pregnancy, childbirth, or menopause. It can also be caused by prostate issues, neurological disorders, or certain medicines. Lifestyle choices like obesity and smoking can play a role too.
Are there any alternative medicine options for urinary incontinence?
Yes, herbal remedies, acupuncture, and biofeedback therapy might help. But, always talk to a doctor before trying these treatments.
How can I manage nocturia?
To fight nocturia, cut down on fluids before bed and avoid caffeine and alcohol. Relaxation techniques can also help. Medications and bladder training can reduce nighttime trips to the bathroom.
What are the benefits of pelvic floor exercises for urinary incontinence?
Pelvic floor exercises, like Kegels, strengthen the bladder muscles. This improves bladder control and reduces symptoms. Regular exercise also boosts pelvic health.
Are there any medications available for urinary incontinence?
Yes, there are medicines like antimuscarinic drugs and beta-3 adrenergic agonists. Alpha-blockers and topical estrogen are also options. These help relax the bladder muscle and improve bladder capacity.
How can I choose the right absorbent products for urinary incontinence?
Look for absorbency, comfort, and discretion when picking products. Choose breathable materials and secure fastening. Odor control is also important for confidence and comfort.
When should I seek professional help for urinary incontinence?
If incontinence is persistent or severe, or if you have painful urination or blood in your urine, see a doctor. They can help find the cause and suggest treatments.
What can I expect during a medical evaluation for urinary incontinence?
Your doctor will review your history and perform a physical exam. They might do tests like urinalysis or urodynamic testing. Then, they’ll create a treatment plan for you.
Are there any solutions for incontinence that can improve my quality of life?
Yes, by making lifestyle changes, trying behavioral therapies, and using medical treatments, you can manage incontinence. Work with a healthcare professional to find the best plan for you.
References
National Center for Biotechnology Information. (2025). How to Treat Urinary Incontinence 5 Effective Solutions. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10284157/)