A hysterectomy is a big surgery that removes the uterus. It leaves many wondering about changes in their body. Nearly 600,000 hysterectomies are performed annually in the United States. This makes it a common surgery that needs clear understanding of its effects. Vaginal closure replaces the cervix after hysterectomy. Learn how the vaginal cuff is created and heals during recovery.
After a hysterectomy, the vaginal cuff formation is key. It’s how the vagina closes after the cervix is removed. Knowing about this is important for managing recovery and health.
The vaginal closure process and the new anatomy after a hysterectomy can be complex. But, knowing about these changes can greatly help a patient’s recovery and well-being.
Key Takeaways
- Understanding the changes in anatomy after a hysterectomy is key for recovery.
- Vaginal cuff formation is a vital part of post-hysterectomy anatomy.
- Knowing about post-hysterectomy anatomy can improve long-term health.
- Nearly 600,000 hysterectomies are done each year in the United States.
- Understanding vaginal closure helps manage recovery and expectations.
Understanding Hysterectomy: Types and Procedures

Choosing to have a hysterectomy means knowing about the different procedures and how they affect the body. A hysterectomy removes the uterus. It’s done for reasons like uterine cancer, fibroids, and heavy bleeding.
Different Types of Hysterectomy
There are many types of hysterectomy surgeries. Each one is used for different reasons and has its own effects. A total hysterectomy removes the uterus and cervix. A subtotal hysterectomy takes out the uterus but keeps the cervix.
The choice between these depends on the health issue and the patient’s overall health.
Common Reasons for Cervix Removal
The cervix is removed in some hysterectomies for cancer or abnormal cell changes. Sometimes, it’s removed to prevent future health problems. The decision to remove the cervix depends on the patient’s condition and the surgeon’s advice.
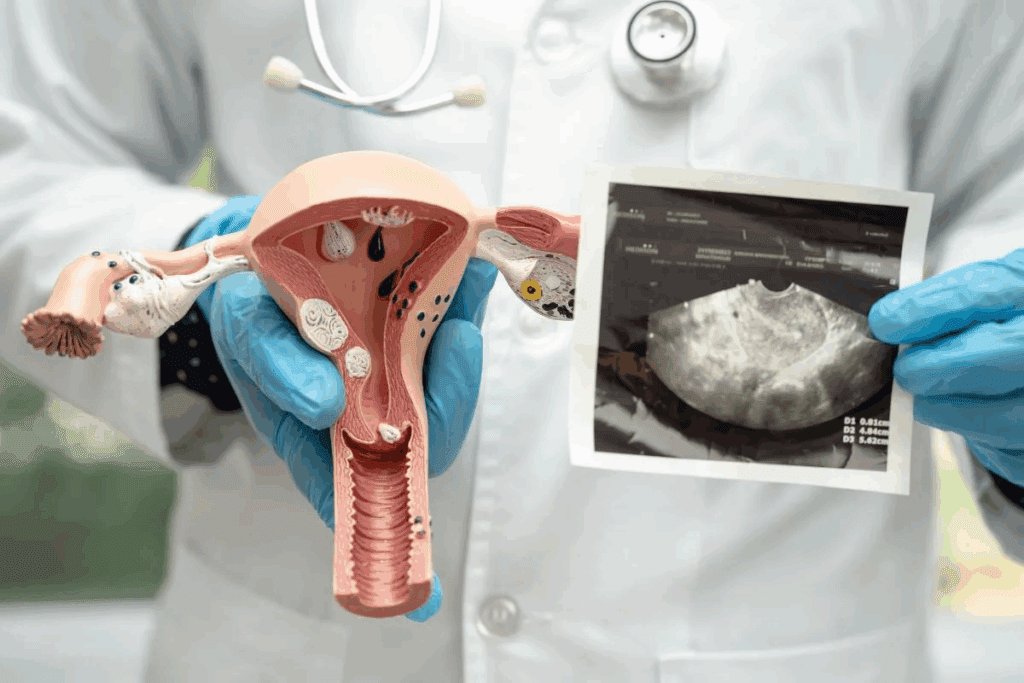
Anatomical Changes After Surgery
After a hysterectomy, the body changes a lot. Removing the uterus and cervix affects the vagina and pelvic floor. It’s important to understand these changes for proper care after surgery.
These changes can affect a patient’s life quality. A detailed follow-up care plan is needed. This includes watching for complications and addressing any changes in pelvic support or vaginal function.
The Role of the Cervix in Female Anatomy

The cervix is key to female reproductive health. It connects the uterus to the vagina, playing a vital role in fertility and well-being. It helps with various physiological processes.
Functions of the Cervix
The cervix has several important functions. It makes mucus that changes throughout the menstrual cycle. This helps or hinders sperm passage, depending on the cycle time.
The mucus plug also acts as a barrier against infection. It allows menstrual blood to flow out of the uterus during a woman’s period.
Cervical mucus is vital for fertility. During ovulation, it becomes more alkaline and less viscous, aiding sperm. At other times, it’s more acidic and thicker, blocking sperm. This is key for natural conception and fertility awareness methods.
What Happens When It’s Removed
Removing the cervix during a hysterectomy changes things. The vaginal cuff closes the top of the vagina, taking over some cervix functions. But, it can also change vaginal depth and elasticity.
Removing the cervix also affects the pelvic anatomy. The ligaments and tissues that supported it may change or be reattached. This can impact pelvic stability.
Impact on Surrounding Organs
Removing the cervix can affect nearby organs. The pelvic floor muscles and ligaments may change, impacting bladder and bowel function. This can lead to issues like urinary incontinence or pelvic organ prolapse.
| Organ/System | Potential Impact | Possible Complications |
| Bladder | Changes in support structures | Urinary incontinence |
| Bowel | Altered pelvic floor dynamics | Constipation or fecal incontinence |
| Vagina | Changes in depth and elasticity | Dyspareunia (painful intercourse) |
Knowing these impacts is key for managing expectations and addressing any complications after a hysterectomy.
The Vaginal Cuff: The New Anatomical Structure
The vaginal cuff is a key part of a woman’s body after a hysterectomy. It forms when the cervix is removed. This new part is important for women who have had this surgery.
Definition and Formation
The vaginal cuff is made during a hysterectomy. The surgeon closes the vagina after removing the cervix and uterus. The edges of the vaginal wall are sewn together to make a tight seal.
This step is vital to avoid problems like bleeding or prolapse. The way the cuff is made can change based on the surgery and the surgeon.
How It Differs from the Cervix
The vaginal cuff is not like the cervix. The cervix has its own role in childbirth and menstrual cycles. The main difference is how it’s made and its purpose. The vaginal cuff seals the vaginal canal after the reproductive organs are removed.
- The vaginal cuff doesn’t have the same functions as the cervix.
- It’s not a natural part of the body but is made during surgery.
- Its main job is to support and close the vaginal vault.
Anatomical Position and Connections
The vaginal cuff sits at the top of the vaginal canal, where the cervix used to be. It’s linked to the pelvic area through ligaments and tissues, which help keep it in place and support it.
The position of the vaginal cuff is key for keeping the pelvic organs stable and avoiding problems like prolapse. The connections between the cuff and the surrounding tissues are important for the pelvic floor’s stability.
- The vaginal cuff is at the top of the vagina.
- It’s supported by pelvic ligaments and tissues.
- It’s important for the pelvic floor to heal well after surgery.
The vaginal cuff, created during surgery, alters the support dynamics of the pelvic area.
Vaginal closure during hysterectomy is a precise process. It ensures a secure vaginal cuff is created.
Surgical Techniques
The surgical techniques used are key for a successful hysterectomy. Research in Cureus shows surgeons use various methods. These include continuous or interrupted sutures for closing the vagina.
The choice of technique depends on several factors. These include the patient’s anatomy, the surgeon’s preference, and the type of hysterectomy.
Key Considerations for Surgical Techniques:
- Patient’s overall health and anatomy
- Type of hysterectomy (abdominal, vaginal, or laparoscopic)
- Surgeon’s experience and preference
Types of Sutures Used
The types of sutures used for vaginal closure vary. Absorbable sutures like Vicryl or Monocryl are often preferred. They are absorbed by the body over time.
| Suture Type | Characteristics | Common Uses |
| Vicryl | Absorbable, braided | Vaginal cuff closure |
| Monocryl | Absorbable, monofilament | Skin closure, vaginal cuff |
| PDS | Absorbable, monofilament | Vaginal cuff, deeper tissue closure |
“The choice of suture material can significantly impact the healing process and the risk of complications.” –
A study on surgical outcomes in gynecology
The vaginal cuff, created during surgery, alters the support dynamics of the pelvic area.
Creating the vaginal cuff is a critical step. It involves closing the vaginal vault to prevent complications. This requires careful attention to detail for a secure closure.
The vaginal cuff is made by suturing the edges of the vaginal vault together. This supports the surrounding pelvic structures.
Steps in Creating the Vaginal Cuff:
- Assessing the vaginal vault for any bleeding or oozing
- Suturing the edges of the vaginal vault together
- Ensuring the closure is secure and supports pelvic structures
Surgical Approaches to Vaginal Cuff Creation
There are several ways to create the vaginal cuff during surgery. Each method has its own benefits. The choice of approach can greatly affect how well a patient recovers.
Abdominal Approach
The abdominal approach makes the vaginal cuff through an abdominal incision. This method lets the surgeon see the area clearly. It’s often chosen when there are complications or for certain medical reasons.
Vaginal Approach
The vaginal approach makes the cuff through the vagina, without an abdominal cut. This can lead to less pain and quicker healing. It’s seen as less invasive than the abdominal method.
Laparoscopic Methods
Laparoscopic methods use small cuts and a camera to create the cuff. This method can cause less scarring and faster healing. Laparoscopic surgery is known for its precision and lower risk of problems.
How Surgical Approach Affects Outcomes
The surgical method chosen can greatly impact patient results. This includes how fast they recover, the risk of complications, and their overall satisfaction. Knowing the differences between these methods is key to making the right choice.
Each surgical method has its own use, benefits, and possible downsides. The choice depends on the patient’s health, the reason for the hysterectomy, and the surgeon’s expertise.
Pelvic Support After Cervix Removal
After a hysterectomy, the body changes in ways that affect pelvic support. The cervix’s removal means other parts must work harder to keep things stable. This is to avoid issues like pelvic organ prolapse.
How Pelvic Stability Is Maintained
Pelvic stability comes from muscles, ligaments, and fascia. The pelvic floor muscles are key. They work with other tissues to hold the pelvic organs in place.
“The integrity of the pelvic floor is critical for continence and supporting the pelvic organs.”
Ligaments and fascia around the pelvic organs also help a lot. They offer a framework that supports the organs and spreads out forces on the pelvic floor.
Role of Surrounding Tissues
The vaginal cuff, created during surgery, alters the support dynamics of the pelvic area.
- The vaginal cuff acts as a new endpoint for the vagina.
- Ligaments and fascia help keep the vaginal cuff in place.
- Pelvic floor muscles support the vaginal cuff and keep the organs in position.
Preventing Pelvic Organ Prolapse
To stop pelvic organ prolapse after cervix removal, we need to take several steps. This includes keeping pelvic floor muscles strong, avoiding heavy lifting, and managing pressure in the abdomen.
| Prevention Strategies | Description |
| Pelvic Floor Exercises | Regular exercises to strengthen the muscles supporting the pelvic organs. |
| Avoiding Heavy Lifting | Reducing strain on the pelvic floor by avoiding heavy lifting and bending. |
| Managing Abdominal Pressure | Controlling conditions like chronic coughing or constipation to reduce pressure on the pelvic floor. |
It is essential for women to discuss potential changes with their healthcare provider.
Immediate Post-Surgical Anatomy
After a hysterectomy, the body changes a lot. The cervix is removed, and a new vaginal cuff is made. These changes are key to healing.
What to Expect Right After Surgery
Right after surgery, you might feel some pain and swelling in your vagina. The vaginal cuff might be sore and swollen. It’s important to follow your doctor’s care plan to avoid problems.
Key aspects to consider immediately after surgery include:
- Managing pain effectively
- Monitoring for signs of infection
- Adhering to a prescribed post-operative care plan.
Initial Healing Process
The healing starts a few days after surgery. The body begins to fix the tissues around the vaginal cuff. Avoid heavy lifting and bending to protect the surgery site.
The healing process can be influenced by various factors, including overall health, age, and adherence to post-operative instructions.
| Healing Stage | Timeline | Key Characteristics |
| Initial Healing | 0-3 days | Swelling, discomfort, tissue repair initiation |
| Early Recovery | 3-14 days | Gradual reduction in swelling, continued tissue repair |
| Advanced Healing | 2-6 weeks | Significant reduction in discomfort, continued strengthening of vaginal cuff |
Normal Post-Operative Symptoms
After a hysterectomy, you might feel some pain, vaginal discharge, and slight bleeding. These symptoms can be managed with medication and rest.
It’s important to know about possible complications. If you have severe symptoms, seek medical help. Knowing what to expect during recovery can help you get through it better.
The Healing Timeline of the Vaginal Cuff
The vaginal cuff, created during surgery, alters the support dynamics of the pelvic area.
First Few Weeks
In the first weeks after surgery, the body starts to heal. You might feel some pain, have vaginal discharge, or spot. These symptoms can be managed with rest, keeping the area clean, and sometimes medicine from your doctor.
The vaginal cuff starts healing right after surgery. But, the most healing happens in the first few weeks. Doctors usually tell patients to avoid heavy lifting, bending, or hard activities to avoid problems like vaginal cuff dehiscence.
Complete Healing Period
The vaginal cuff fully heals in several months. Usually, it’s healed in 6 to 8 weeks, but it can vary. Things like your health, age, and any complications can affect how fast it heals.
It’s important to have follow-up appointments with your doctor during this time. These visits help check if everything is healing right. They also catch any problems early.
Factors Affecting Healing Time
Many things can change how fast the vaginal cuff heals. These include your health, the surgery method, any infections, and if you’ve had other pelvic surgeries.
- Surgical Technique: The way the hysterectomy is done (abdominal, vaginal, or laparoscopic) can affect healing.
- Patient’s Health: Conditions like diabetes or being overweight can slow healing.
- Post-operative Care: Following your doctor’s instructions after surgery can greatly impact recovery.
Understanding these factors assists both patients and healthcare professionals in planning more effectively. It ensures the vaginal cuff heals as well as possible.
Potential Complications with Vaginal Closure
It is essential for women to discuss potential changes with their healthcare provider.
Vaginal Cuff Dehiscence
Vaginal cuff dehiscence is a serious issue. It happens when the top of the vagina, called the vaginal cuff, opens. This can cause infections and might need more surgery.
Infection Risks
Any surgery, like vaginal closure, can lead to infections. Symptoms can be mild or severe, like fever, pain, and bad smells. It’s key to get medical help quickly if you notice these signs.
Bleeding Concerns
It is essential for women to discuss potential changes with their healthcare provider.
Granulation Tissue Formation
Granulation tissue can grow at the vaginal cuff site. It can cause pain or bleeding. Doctors might use cauterization or other treatments to manage it.
| Complication | Symptoms | Treatment |
| Vaginal Cuff Dehiscence | Severe pain, bleeding, infection signs | Surgical repair, antibiotics |
| Infection | Fever, pain, foul-smelling discharge | Antibiotics, supportive care |
| Bleeding | Excessive bleeding, spotting | Monitoring, possible surgical intervention |
| Granulation Tissue | Discomfort, irregular bleeding | Cauterization, medical management |
Understanding these factors assists both patients and healthcare professionals in planning more effectively.
Physical Changes Women May Experience
Women who have a hysterectomy may notice many physical changes. These changes can affect how their body works and feels. Each woman’s experience is different.
Sensation Differences
One big change is how things feel. Women might notice altered sensations because of the surgery. For example, one woman said, “After my surgery, I felt a big change in my body, it was like a new normal.” This adjustment period can vary in length.
Structural Changes
The surgery removes the cervix and uterus, causing structural changes in the pelvic area. The vaginal cuff, created during surgery, alters the support dynamics of the pelvic area.
Impact on Urinary Function
Women might see changes in urinary function after the surgery. This could mean problems like incontinence or needing to pee more often. Health experts say, “The close location of the urinary tract to the surgery site can sometimes cause temporary or, in some cases, permanent changes in how you pee.”
Changes in Vaginal Depth and Elasticity
The surgery can also change vaginal depth and elasticity. The vaginal cuff makes the vaginal canal shorter, and some women might find it less elastic. A medical journal notes, “The vaginal cuff’s formation is key for supporting the vaginal vault, but it can change how deep and elastic the vagina is.”
It is essential for women to discuss potential changes with their healthcare provider. This way, they can understand what to expect and how to handle any issues that come up.
Sexual Function After Vaginal Cuff Formation
The vaginal cuff, created during surgery, alters the support dynamics of the pelvic area.
When It’s Safe to Resume Sexual Activity
Many women wonder when they can start having sex again after a hysterectomy. Doctors usually say wait 6 to 8 weeks. This gives the vaginal cuff time to heal.
What to Expect During Intercourse
When the vaginal cuff heals, sex might feel different. You might notice:
- Changes in Sensation: Some women feel less sensitive or different sensations.
- Vaginal Dryness: Hormonal changes can cause dryness, making sex less comfortable.
- Depth and Elasticity: The vaginal cuff might change how deep or elastic your vagina is.
Addressing Common Concerns
Women often worry about the safety and comfort of sex after a hysterectomy. They might worry about:
- Fear of Complications: Knowing the risks and being careful can help ease these fears.
- Pain During Intercourse: Talking to a doctor about any pain can find ways to make sex more comfortable.
Communicating with Partners
Talking openly with your partner is key during this time. Sharing any changes, worries, or discomfort can keep your sex life healthy and enjoyable.
Understanding the changes from vaginal cuff formation and talking openly with doctors and partners can help women feel confident about their sex lives.
Long-term Anatomical Considerations
It’s important to know about the long-term changes after a hysterectomy. This helps manage what to expect and how to recover. The removal of the cervix and the creation of the vaginal cuff cause permanent changes in the female body.
Permanent Changes to Expect
The vaginal cuff, created during surgery, alters the support dynamics of the pelvic area.
- The vaginal cuff becomes a new anatomical landmark.
- There may be changes in vaginal depth and elasticity.
- Pelvic organ support is maintained through the surrounding tissues and muscles.
How the Body Adapts Over Time
Over time, the body adjusts to the changes from the hysterectomy. The vaginal cuff heals and becomes part of the normal pelvic anatomy. The tissues and muscles around it continue to support the pelvic organs.
Adaptation Process: Healing times vary, but usually, the body adapts within a few months to a year after surgery. Health, age, and any complications can affect how quickly the body adapts.
Long-term Pelvic Support
Keeping the pelvic area supported long-term is key after a hysterectomy. The pelvic floor muscles are vital in supporting the pelvic organs. Doing pelvic floor exercises can strengthen these muscles and prevent issues like pelvic organ prolapse.
- Pelvic floor exercises can help maintain pelvic support.
- Regular check-ups with healthcare providers are essential for monitoring pelvic health.
- A healthy lifestyle, including a balanced diet and regular exercise, contributes to overall pelvic well-being.
Pelvic Floor Exercises and Rehabilitation
Keeping the pelvic floor muscles strong is key after a hysterectomy. These muscles support the pelvic organs. Their strength greatly affects recovery.
Importance of Pelvic Floor Strength
Pelvic floor strength is vital for continence and pelvic stability. Weak muscles can cause incontinence and prolapse. Pelvic floor exercises can strengthen these muscles, lowering the risk of these problems.
Recommended Exercises
Several exercises can strengthen the pelvic floor muscles. These include:
- Kegel exercises: These involve contracting and releasing the pelvic floor muscles to strengthen them.
- Pelvic tilts: This exercise helps in engaging the core and pelvic floor muscles.
- Bridge pose: Strengthens the glutes and pelvic floor muscles.
It’s important to start these exercises with a healthcare professional’s guidance. This ensures they are done correctly.
Working with Physical Therapists
Physical therapists specializing in pelvic health can create personalized exercise plans. They teach proper technique and how to progress. This is very helpful for women after a hysterectomy, as they can address specific challenges and improve pelvic floor function.
Timeline for Starting Exercises
The time to start pelvic floor exercises after a hysterectomy varies. It depends on health and surgery specifics. Gentle exercises can start a few weeks post-surgery, with more intense ones later. Always follow a healthcare provider’s advice on when and how to progress with exercises.
Medical Follow-up and Monitoring the Vaginal Cuff
After a hysterectomy, Monitoring the vaginal cuff’s health is crucial. Regular check-ups are key to spotting and fixing any problems early.
Regular Check-ups
Seeing your healthcare provider regularly is vital. They will check how well the vaginal cuff is healing. They might do a pelvic exam to see if everything is okay.
How Often? How often you need to see your doctor depends on your health and the surgery. You’ll usually have a first visit a few weeks after surgery. Then, you might need more visits based on your recovery.
Signs That Require Medical Attention
Knowing the signs of trouble with the vaginal cuff is important. Look out for:
- Unusual vaginal discharge or odor
- Severe pelvic pain
- Vaginal bleeding that is heavy or persistent
- Fever
- Signs of infection or abscess
If you notice any of these, get help right away.
Long-term Monitoring Recommendations
Monitoring the vaginal cuff’s health is crucial.
| Monitoring Aspect | Recommendation | Frequency |
| Pelvic Examination | Assess vaginal cuff integrity | At least annually |
| Symptom Review | Discuss any unusual symptoms | At each visit |
| Diagnostic Tests | Ultrasound or other tests as needed | As recommended by healthcare provider |
By sticking to these guidelines and talking openly with your doctor, you can have the best recovery after a hysterectomy.
Conclusion
It is essential for women to discuss potential changes with their healthcare provider. cervix leads to the vaginal cuff. This new structure helps keep the pelvic area stable.
The vaginal closure and the vaginal cuff’s creation are key parts of the surgery. Knowing about post-hysterectomy anatomy helps women recover better. It also helps them make smart health choices.
Healing, possible complications, and long-term anatomy are key to consider. Being informed helps women recover smoothly. It ensures they maintain good pelvic health after a hysterectomy. This leads to a better life with vaginal closure.
FAQ
What is the vaginal cuff, and how is it formed?
The vaginal cuff is made after a hysterectomy. It replaces the cervix. It’s created by stitching the top of the vagina shut with internal sutures.
What are the different types of hysterectomy procedures, and how do they affect vaginal closure?
There are several hysterectomy methods, like abdominal, vaginal, and laparoscopic. The type chosen can change how the vagina is closed and the vaginal cuff is made.
How is pelvic support maintained after the removal of the cervix?
Pelvic support comes from muscles and ligaments around the pelvic floor. Exercises and rehabilitation can also help keep the pelvic floor stable.
What can I expect immediately after a hysterectomy, and how long does the initial healing process take?
Right after surgery, you might feel pain, bleed, and swell. Healing takes weeks. You’ll likely feel tired, have pain, and notice changes in vaginal discharge.
How long does it take for the vaginal cuff to heal completely?
Healing the vaginal cuff fully can take 3 to 6 months. Your health, age, and any complications can influence how fast you heal.
What are the possible complications with vaginal closure, and how can they be prevented?
Complications like vaginal cuff dehiscence and infections can happen. To avoid them, follow your doctor’s advice, go to follow-up visits, and tell your doctor about any unusual symptoms.
How does the removal of the cervix affect sexual function, and when is it safe to resume sexual activity?
Removing the cervix might change how you feel during sex. But many women can start again after a few months. Wait 6-8 weeks before trying sex again and talk to your partner about any issues.
What are the long-term anatomical changes to expect after a hysterectomy, and how can pelvic support be maintained?
You might notice changes in vaginal depth and elasticity over time. To keep your pelvic floor strong, do exercises, go to check-ups, and follow your doctor’s advice.
Why are pelvic floor exercises and rehabilitation important after a hysterectomy?
These exercises are key to keeping your pelvic floor strong. They help prevent prolapse and improve your overall health after a hysterectomy.
How often should I have medical follow-up appointments after a hysterectomy, and what signs require medical attention?
It’s important to see your doctor regularly after a hysterectomy. If you notice heavy bleeding, pain, or fever, tell your doctor right away.
What is the role of absorbable sutures in vaginal closure, and how do they affect the healing process?
Absorbable sutures close the vaginal cuff and dissolve over time. They help the healing process by providing a secure closure that promotes tissue healing.
How does the surgical reconstruction of the vaginal cuff impact post-hysterectomy anatomy?
Rebuilding the vaginal cuff is vital for pelvic support and overall health after a hysterectomy. It creates a stable end to the vaginal canal.
References:
- Aydogmus, H. (2017). Cuff Closure by Vaginal Route in Total Laparoscopic Hysterectomy: Case Series and Review. Journal of Minimally Invasive Gynecology, 24(4), 584-590. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5427386/
- Planella, L. V. et al. (2025). Optimizing Vaginal Cuff Closure: A Systematic Review and Meta-analysis. Journal of Minimally Invasive Gynecology. https://pubmed.ncbi.nlm.nih.gov/40639552/

































