
Diagnosing osteoporosis depends a lot on lab tests that check bone mineral density (BMD). The main tool used is the dual-energy X-ray absorptiometry (DXA) scan.Listing the key osteoporosis labs and diagnostic tests (including DEXA) used to confirm bone loss and rule out secondary causes.
DXA scans send a high- and low-energy X-ray beam through the body. They usually check the hip and spine. This test is non-invasive and helps find bone loss early. It lets doctors start treatment before serious fractures happen.
Liv Hospital focuses on patients with its new diagnostic methods. They make sure people get a full osteoporosis assessment with the latest technology.

Finding osteoporosis early is key to keeping bones strong and avoiding breaks. Osteoporosis often doesn’t show symptoms until a bone breaks. So, finding it early is very important for managing it well.
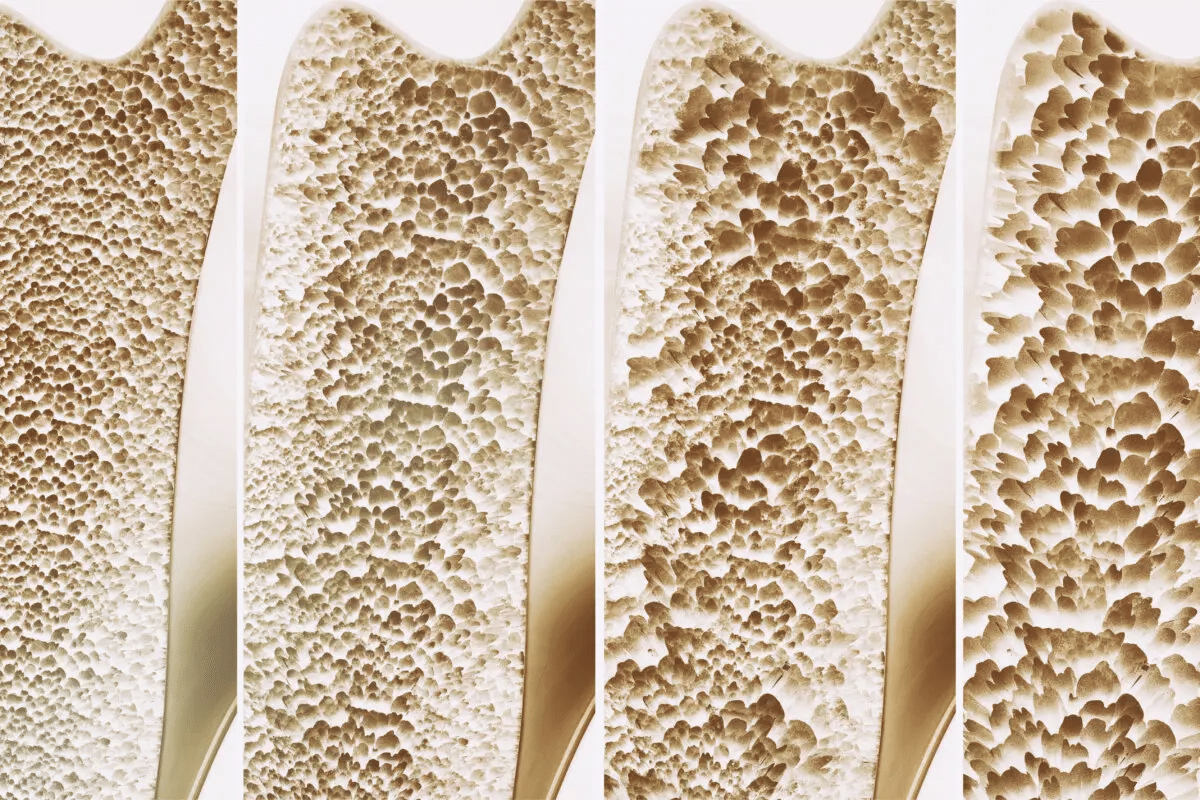
Osteoporosis causes bones to weaken and break more easily. Knowing why bones get weaker is key to acting fast.
Bones stay healthy when bone formation and resorption are in balance. But, as we get older, this balance changes, leading to bone loss. Hormonal changes, lifestyle, and some health issues can make this loss worse.
Progressive bone loss not only makes bones less dense but also changes their shape. This makes breaks more likely. Testing for osteoporosis lab tests early can spot those at risk.
Some factors make getting osteoporosis more likely, so it’s smart to test early. These include age, sex, family history, and certain health issues.
|
Risk Factor |
Description |
|---|---|
|
Age |
Risk goes up with age, more after 50 |
|
Sex |
Women are more at risk, after menopause |
|
Family History |
Having osteoporosis or breaks in close relatives |
|
Medical Conditions |
Conditions like rheumatoid arthritis, diabetes, and thyroid issues |
Knowing these risk factors helps decide who needs osteoporosis laboratory tests. Finding it early can stop breaks and make life better.
Bone mineral density testing is key in diagnosing and managing osteoporosis. It gives vital info on bone health. This helps doctors check fracture risks and see if treatments work.
BMD testing checks the minerals like calcium in bones. This shows how strong and healthy bones are. The results are in grams per square centimeter (g/cm²) and compared to a young adult’s average.
BMD testing is vital. It spots people with low bone mass or osteoporosis early. Doctors can then predict fracture risks and suggest prevention or treatment.
Doctors decide on BMD testing based on risk factors for osteoporosis and fractures. Key risk factors include age, gender, family history, and lifestyle or medical conditions.
Screening guidelines for BMD testing change with age, gender, and risk factors. For example, the USPSTF suggests BMD testing for women aged 65 and older. They also recommend it for postmenopausal women under 65 with risk factors.
Knowing these guidelines and BMD testing basics helps people protect their bone health. This reduces the risk of osteoporosis-related fractures.
DXA scans are key in diagnosing osteoporosis. They measure bone density precisely. This technology is non-invasive and quick, making it a game-changer in bone health.
DXA scans use low-level X-rays to see bone and soft tissue. They have two X-ray beams to measure bone mineral content and density. This is done in areas like the hip and spine.
The scan is painless and quick. Patients lie on a table while the DXA machine scans. The results show bone density, helping doctors understand bone health.
The hip and spine are key for DXA scans. They are common fracture areas. This helps doctors understand fracture risk and bone health.
Hip Assessment: The hip is important because hip fractures are serious. DXA looks at the femoral neck and total hip.
Spine Assessment: The lumbar spine is also critical. DXA can spot early bone loss and fractures here. This is important for quality of life.
DXA scans are very accurate in measuring bone density. But, there’s a concern about radiation. DXA uses a low dose, making it safe.
DXA machines use the least radiation needed for accurate results. They’re not used for repeated scans unless needed. This keeps radiation exposure low.
Understanding DXA results is key to spotting osteoporosis and starting treatment. DXA scans measure bone mineral density (BMD). This is then compared to a standard to see the risk of osteoporosis.
T-scores are vital in DXA results. They compare your BMD to a young adult’s, of the same sex. The T-score shows how many standard deviations you are from the average young adult BMD.
T-score Interpretation:
Z-scores compare your BMD to someone of the same age. This score is useful for younger people or when looking at secondary causes of osteoporosis.
A Z-score below -2.0 might mean your low BMD is not just age-related. It could point to other factors causing bone loss.
The T-score helps diagnose osteoporosis and assess fracture risk. The lower the T-score, the higher the fracture risk. This is important for doctors to decide on treatment and prevention.
|
T-score Range |
WHO Classification |
Fracture Risk |
|---|---|---|
|
Above -1 |
Normal |
Low |
|
-1 to -2.5 |
Osteopenia |
Moderate |
|
-2.5 or lower |
Osteoporosis |
High |
It’s important for doctors to understand DXA results well. By looking at T-scores and Z-scores, they can find at-risk patients. This helps them plan the best prevention and treatment.
Beyond just bone density tests, blood and urine tests are key for a full osteoporosis check-up. These tests give important info on why bones might be losing strength. They help doctors create the best treatment plans.
Basic blood tests are vital for understanding osteoporosis. They show how well the body is working and can spot issues that might harm bones. These tests check kidney and liver health and mineral levels, all important for bones.
Kidney function tests are important because kidney problems can lead to bone loss. They affect how the body handles calcium and phosphate. Liver enzymes are also checked to make sure liver issues aren’t causing osteoporosis.
Calcium and vitamin D are key for strong bones. Testing their levels is a big part of checking for osteoporosis. Calcium levels are checked to see if they’re normal. Vitamin D levels are also tested, as a lack of it can cause bone loss.
Vitamin D helps the body absorb calcium. Without enough, bones can’t get the calcium they need. Doctors check vitamin D levels to see if supplements are needed.
Hormonal imbalances can hurt bone health. Testing hormones is a big part of checking for osteoporosis. Doctors look at thyroid function, parathyroid hormone levels, and other hormones that affect bones.
Thyroid disorders can lead to osteoporosis if not treated. Hyperthyroidism can make bones lose strength faster. Parathyroid hormone imbalances can also affect calcium levels and bone health.
By looking at all these test results, doctors can understand what’s causing osteoporosis. They can then create a treatment plan that works best.
Measuring bone turnover markers is key to understanding bone health in osteoporosis. These markers show how bones are built and broken down. This helps doctors diagnose and treat osteoporosis better.
Bone formation markers like Procollagen Type 1 N-terminal Propeptide (P1NP) and osteocalcin are important. P1NP is a protein piece made when bones are built. Osteocalcin is made by bone-building cells and shows how much bone is being made.
P1NP and Osteocalcin: These markers are important because they show how active bone-building is. High levels can mean more bone turnover, which can happen in osteoporosis or when bones heal.
Bone resorption markers, such as C-terminal telopeptide (CTX) and N-terminal telopeptide (NTX), show bone breakdown. CTX and NTX are pieces of bone collagen broken down by bone-eating cells.
CTX and NTX: These markers are key for checking how fast bones are being broken down. High levels of CTX or NTX can mean more bone breakdown, often seen in osteoporosis or other bone diseases.
Bone turnover markers are very useful in checking how well osteoporosis treatment is working. By looking at changes in bone turnover, doctors can see if a treatment is effective and make changes if needed.
|
Marker |
Type |
Clinical Use |
|---|---|---|
|
P1NP |
Bone Formation |
Monitoring anabolic therapy response |
|
Osteocalcin |
Bone Formation |
Assessing bone turnover |
|
CTX |
Bone Resorption |
Monitoring antiresorptive therapy response |
|
NTX |
Bone Resorption |
Assessing risk of bone loss |
Bone turnover markers are a valuable tool in managing osteoporosis. They help doctors tailor treatments to each patient and track how well treatments are working over time.
DXA is the top choice for finding osteoporosis, but other methods are also good. These options are great when DXA is not available or for certain health needs.
Quantitative Computed Tomography (QCT) is a detailed scan for bone health. It looks at the spine and hip. Unlike DXA, it measures bone volume, not just area.
Peripheral DXA (pDXA) checks bone density at places like the heel or forearm. It’s used for quick screenings because it’s portable and cheaper.
Quantitative Ultrasound (QUS) is a safe way to check bone health. It uses sound waves at the heel to guess bone strength.
In summary, QCT, pDXA, and QUS are useful for bone health checks. Each has its own strengths and uses. They help doctors find and treat osteoporosis in different ways.
Understanding secondary causes of osteoporosis is key to a good treatment plan. Lab tests are vital in finding these causes that lead to bone loss and higher fracture risk.
Thyroid issues, like hyperthyroidism, can speed up bone loss, leading to osteoporosis. Thyroid function tests like TSH, free T3, and free T4 help spot thyroid-related bone loss. Parathyroid problems, like hyperparathyroidism, also cause osteoporosis by taking more calcium from bones. Parathyroid hormone (PTH) levels check parathyroid function.
Kidney and liver diseases can cause osteoporosis by messing with vitamin D and mineral balance. Liver function tests like ALT and AST, and kidney function tests like serum creatinine and eGFR are key. They help find liver or kidney problems that might be causing osteoporosis.
Celiac disease and other malabsorptive conditions can cause osteoporosis by not absorbing nutrients like calcium and vitamin D. Serologic tests for celiac disease, like tTGA and EMA, help diagnose it. Checking vitamin D levels and other nutrient deficiencies also helps spot malabsorption issues.
By finding and treating secondary causes of osteoporosis, doctors can create better treatment plans. This helps improve bone health and lower the risk of fractures.
Understanding the tiny details of osteoporotic bone is key for accurate diagnosis and treatment. Histological assessment looks closely at bone tissue. It shows the changes in structure and cells due to osteoporosis.
A bone biopsy takes a bone sample for examination. It’s useful when osteoporosis diagnosis is unsure or to rule out other bone issues. Bone biopsy is often suggested for patients with unusual fractures or unclear test results.
Several factors decide if a bone biopsy is needed:
Histomorphometry analysis looks at bone tissue structure in detail. It measures bone volume, trabecular thickness, and more. Histomorphometry helps understand bone loss and osteoporosis mechanisms.
The process includes:
Osteoporotic bone shows specific microscopic signs, like reduced density and changed trabecular structure. Microscopic examination shows thin trabeculae, increased spacing, and lost connectivity.
The microscopic signs of osteoporotic bone are vital for diagnosis and treatment. By studying these signs, doctors can better understand the disease’s progress. They can then plan targeted treatments.
New technologies are changing how we find and treat osteoporosis. They give doctors more accurate info on bone health. This helps patients get better care.
The Trabecular Bone Score is a new, non-invasive test. It looks at bone texture and structure. It’s different from old bone density tests because it checks the bone’s inner structure.
TBS Benefits:
HR-pQCT is a high-tech scan that shows bone details in 3D. It’s great for looking at both the outer and inner bone parts. This helps doctors understand bone strength and risk of breaking.
Key Features of HR-pQCT:
Artificial intelligence is being used more in osteoporosis. AI looks at lots of data to guess who might break bones. It uses clinical info and scan data to make predictions.
|
Technology |
Description |
Benefits |
|---|---|---|
|
TBS |
Assesses bone texture and microarchitecture |
Provides additional information beyond BMD, helps in assessing fracture risk |
|
HR-pQCT |
Offers detailed 3D images of bone microarchitecture |
Assesses cortical and trabecular bone compartments, provides information on bone strength |
|
AI |
Analyzes datasets to predict fracture risk |
Improves fracture risk prediction, identifies high-risk patients |
These new tools are making it easier to find and treat osteoporosis. They help doctors give better care and improve patient results.
Getting a correct diagnosis for osteoporosis is key. It’s important to use many tests to understand bone health well. This way, doctors can help patients better.
Tests like DXA scans, blood tests, and others are very helpful. They check bone density, how bones are changing, and the chance of breaking a bone. These tools help find who has osteoporosis and who might get it.
Doctors use a complete plan to diagnose osteoporosis. They look at the patient’s health, medical history, and test results. This approach helps create the right treatment plan. It makes patients’ outcomes better and lowers the chance of fractures.
Using different tests and technologies, doctors can give care that fits each patient. This helps manage osteoporosis better and keeps bones healthy.
To diagnose osteoporosis, doctors use a test called the Dual-Energy X-ray Absorptiometry (DXA) scan. This scan checks bone mineral density. Blood and urine tests also help by looking at calcium, vitamin D, and hormone levels.
Bone mineral density testing checks the bone’s mineral content. It’s usually done with DXA scans. It’s suggested for people over 65, those with a family history of osteoporosis, and those at risk due to low weight or previous fractures.
DXA scans use X-rays to measure bone density in the hip and spine. These areas are common for osteoporotic fractures. The results are compared to a young adult’s to find T-scores.
T-scores compare your bone density to a young adult’s. Z-scores compare it to someone of the same age. T-scores help diagnose osteoporosis and predict fracture risk. Z-scores help identify abnormal bone density for your age.
Bone turnover markers measure bone metabolism. They include P1NP, osteocalcin, CTX, and NTX. These markers help monitor treatment success and fracture risk.
Yes, there are alternatives like Quantitative Computed Tomography (QCT), Peripheral DXA (pDXA), and Quantitative Ultrasound (QUS). These are used for specific bone density assessments.
Tests for secondary causes include thyroid and parathyroid function tests. Kidney and liver function tests are also used. Screening for celiac disease and malabsorption is done too.
A bone biopsy is needed when there’s a suspicion of bone disease or when other tests are unclear. It helps analyze bone features under a microscope.
New technologies include Trabecular Bone Score (TBS), High-Resolution Peripheral Quantitative CT (HR-pQCT), and artificial intelligence in fracture risk prediction. They aim to improve osteoporosis diagnosis and fracture risk assessment.
Osteoporosis diagnosis involves clinical evaluation, medical history, and tests like DXA scans, blood and urine tests, and bone turnover markers. The diagnosis is confirmed by these test results and the presence of osteoporotic fractures.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC2600106/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!