Last Updated on November 25, 2025 by Ugurkan Demir

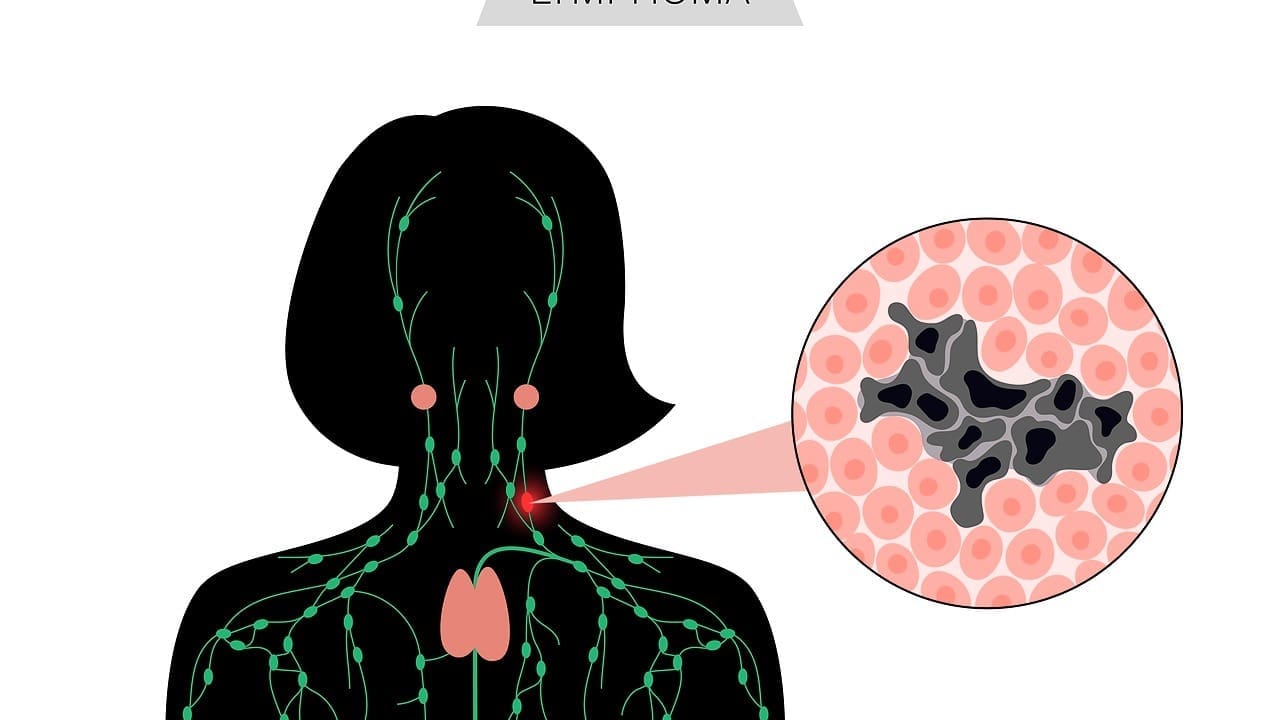
Life-threatening heart rhythm disorders can happen without warning. This makes it vital to spot them early and get help fast. At Liv Hospital, we know how critical quick medical action is for fatal arrhythmias that could cause sudden cardiac arrest.
Arrhythmias are problems with the heart’s electrical system. They affect how the heart pumps. We’ll look at the four lethal arrhythmias that are very dangerous, like ventricular fibrillation and pulseless ventricular tachycardia. Our goal is to provide top-notch healthcare. We support international patients with the latest treatments for heart rhythm issues.
Key Takeaways
- Understanding the four fatal arrhythmias is key for quick medical help.
- Liv Hospital is dedicated to giving world-class care to international patients.
- Our heart rhythm disorder treatments are current and complete.
- Ventricular fibrillation and pulseless ventricular tachycardia are very dangerous arrhythmias.
- Spotting these problems early and getting expert care is critical.
Understanding Heart Rhythms and Electrical Conduction
The heart’s electrical system is key to our heartbeat. It makes sure the heart beats in sync. This keeps our heart rhythm steady.
Normal Heart Electrical System
The heart’s electrical system is complex. It sends out electrical signals. These signals make the heart muscle contract and pump blood.
This system includes the SA node, AV node, bundle of His, and Purkinje fibers. They work together to keep the heart rhythm normal.
How Regular Heartbeats Work
Regular heartbeats come from a well-coordinated electrical system. The SA node starts it off, sending out signals at 60-100 beats per minute. These signals then go to the ventricles, making them contract and pump blood.
This process ensures our heartbeat stays regular.
| Component | Function |
| Sinoatrial (SA) Node | Acts as the heart’s natural pacemaker, generating electrical impulses. |
| Atrioventricular (AV) Node | Delays the electrical impulse, allowing the atria to fully contract. |
| Bundle of His | Transmits the electrical impulse to the ventricles. |
| Purkinje Fibers | Distributes the electrical impulse throughout the ventricles, causing contraction. |
What Is Heart Rhythm?
Heart rhythm is the pattern of electrical impulses that control our heartbeat. A normal rhythm is steady, usually between 60-100 beats per minute. Arrhythmias happen when this rhythm gets disrupted.
Heart disease, electrolyte imbalances, and genetics can cause these disruptions. The heart’s electrical system is vital. It ensures the heart’s chambers contract and relax in sync. Arrhythmias occur when this system fails.
What Are the 4 Fatal Arrhythmias?

The four fatal arrhythmias are serious heart rhythms that can cause sudden cardiac arrest. They make it hard for the heart to pump blood, leading to a quick drop in heart function.
Definition and Classification
The four fatal arrhythmias are ventricular fibrillation, pulseless ventricular tachycardia, asystole, and pulseless electrical activity. They are named based on their heart rhythm patterns and how they show up on an ECG.
Ventricular fibrillation has a chaotic heart rhythm. Pulseless ventricular tachycardia has a fast, regular rhythm but no pulse. Asystole shows a flatline ECG, meaning no heart activity. Pulseless electrical activity has a normal ECG but no effective heart contractions.
Why These Arrhythmias Are Life-Threatening
These arrhythmias are deadly because they make it hard for the heart to pump blood. This leads to poor blood flow to vital organs. Ventricular fibrillation and pulseless ventricular tachycardia can turn into asystole if not treated fast. Asystole and pulseless electrical activity mean the heart is not working right, leading to cardiac arrest.
Without a pulse and poor blood flow, a patient’s condition quickly gets worse. This can lead to death unless treated right away with CPR and defibrillation.
Epidemiology and Mortality Statistics
Ventricular fibrillation and pulseless ventricular tachycardia are big causes of sudden cardiac arrest. They are behind a lot of heart-related deaths. Research shows that survival rates for out-of-hospital cardiac arrests are low. This shows we need to act fast when these arrhythmias happen.
Every year, thousands of people die from these deadly arrhythmias. This shows how important it is to know about them, prevent them, and treat them well.
Ventricular Fibrillation: The Chaotic Killer
Ventricular fibrillation is a serious heart rhythm problem. It causes the heart to beat very fast and irregularly. This can lead to cardiac arrest, a life-threatening situation that needs quick medical help.
Mechanism and Characteristics
Ventricular fibrillation happens when the heart’s electrical system goes wrong. This makes the ventricles contract very fast and not in sync. This messes up the heart’s ability to pump blood, leading to cardiac arrest if not treated fast.
Key characteristics of ventricular fibrillation include:
- Rapid and erratic ventricular contractions
- Ineffective pumping of blood
- Immediate risk of cardiac arrest
- Need for urgent defibrillation
ECG Recognition and Patterns
An electrocardiogram (ECG) is used to diagnose ventricular fibrillation. It shows a unique pattern. On an ECG, ventricular fibrillation looks like a chaotic, irregular waveform without clear P waves or QRS complexes.
The ECG pattern of ventricular fibrillation can vary. Some cases have a coarse fibrillatory pattern, while others have a fine one. Spotting these patterns is key to diagnosing ventricular fibrillation and starting the right treatment.
| ECG Pattern | Description |
| Coarse Fibrillatory Pattern | High-amplitude, chaotic waveform |
| Fine Fibrillatory Pattern | Low-amplitude, chaotic waveform |
Survival Rates and Statistics
The chance of surviving ventricular fibrillation depends on how fast and effective the treatment is. Quick defibrillation can greatly improve survival rates. Studies show that survival rates can be between 5% and 20% if treated quickly. But, these rates drop a lot if treatment is delayed.
Survival statistics for ventricular fibrillation:
| Time to Defibrillation | Survival Rate |
| Within 3-5 minutes | 15%-20% |
| After 5 minutes | 5%-10% |
Knowing about ventricular fibrillation, its signs, and the need for quick treatment can really help patients. We stress the importance of awareness and readiness in dealing with this serious condition.
Pulseless Ventricular Tachycardia: Racing to Cardiac Arrest
Pulseless ventricular tachycardia is a serious heart rhythm problem that needs quick medical help to avoid cardiac arrest. It’s a fast heart rate in the ventricles that stops blood from flowing. This can be deadly if not treated fast.
Distinguishing Features
The main sign of pulseless ventricular tachycardia is a very fast heart rate over 100 beats per minute. It also means there’s no pulse. This is life-threatening because it can turn into ventricular fibrillation or cause cardiac arrest.
An ECG shows a wide QRS complex tachycardia without a P wave, meaning it starts in the ventricles. The lack of a pulse during this arrhythmia is a sign of a serious condition that needs quick action.
Relationship to Ventricular Fibrillation
Pulseless ventricular tachycardia and ventricular fibrillation are closely linked. They are both serious heart rhythm problems. Pulseless ventricular tachycardia can quickly turn into ventricular fibrillation, where the heart’s electrical activity becomes chaotic and stops effective blood flow.
Managing both conditions involves immediate defibrillation and CPR. These are key parts of advanced cardiac life support (ACLS) protocols.
Causes of Pulseless VT
Pulseless ventricular tachycardia often comes from heart disease like coronary artery disease, cardiomyopathy, and structural heart problems. It can also be caused by electrolyte imbalances, like potassium and magnesium issues, and some medications that lengthen the QT interval.
- Coronary artery disease
- Cardiomyopathy
- Electrolyte imbalances
- Prolonged QT interval due to medications
Knowing these causes is key to preventing and managing pulseless ventricular tachycardia well.
Asystole: When the Heart Stops Completely
Asystole is a serious heart condition where the heart stops working. It shows up as a flatline on an electrocardiogram (ECG). This means the heart has stopped beating.
Recognition and ECG Findings
Doctors diagnose asystole by looking at an ECG. If it shows a flat line, it means there’s no heart activity. This is different from other heart problems where the heart beats too fast or chaotically.
ECG Characteristics: A flat line or near-flat line on the ECG monitor, indicating the absence of electrical activity.
Verification: It’s important to check for no pulse and make sure ECG leads are correctly attached to confirm asystole.
Common Causes of Asystole
Asystole can happen due to serious heart or other health issues. Some reasons include:
- Severe heart disease
- Electrolyte imbalances
- Drug overdose or toxicity
- Hypoxia or severe respiratory failure
A medical expert notes, “Asystole is often a terminal rhythm. Its presence means a very bad outlook unless immediate, reversible causes are found and treated.”
“The presence of asystole should prompt an immediate search for reversible causes and initiation of CPR.”
— ACLS Guidelines
Prognosis and Challenges
The outlook for asystole patients is usually very poor. Survival rates are much lower than other heart arrest types. The main challenge is finding and treating causes quickly.
Quick action, like CPR and treating the cause, is key in managing asystole. Even with big challenges, knowing and spotting asystole is essential for doctors to give the right care.
Pulseless Electrical Activity (PEA): The Deceptive Rhythm
Pulseless electrical activity is a serious heart condition. It shows electrical activity but no pulse. This means the heart’s electrical system is working, but it’s not pumping blood.
Understanding the Paradox
PEA is a paradox because the heart’s electrical system is active but not pumping. Normally, electrical activity leads to heartbeats. But in PEA, this doesn’t happen. It’s caused by severe problems, not a primary heart rhythm issue.
Key factors contributing to PEA include:
- Severe metabolic disturbances
- Electrolyte imbalances
- Hypovolemia
- Cardiac tamponade
- Toxic exposures
Common Underlying Causes
PEA often comes from serious heart problems. Some common causes are:
| Cause | Description |
| Hypovolemia | Low blood volume leading to inadequate cardiac output |
| Cardiac Tamponade | Fluid accumulation in the pericardial sac compressing the heart |
| Electrolyte Imbalance | Disturbances in critical electrolytes like potassium and calcium |
A medical expert says, “The key to managing PEA is identifying and treating the underlying cause promptly.”
“Pulseless electrical activity is a true medical emergency requiring swift and decisive action.”
Differential Diagnosis
To diagnose PEA, doctors rule out other conditions like ventricular fibrillation or asystole. An ECG is key, showing a rhythm that should have a pulse but doesn’t.
It’s critical to differentiate PEA from other arrhythmias to provide appropriate care. Treatment for PEA includes fixing the underlying cause, CPR, and other support.
Heart Misfiring: Electrical Disorders of the Heart
When the heart’s electrical system goes wrong, it can cause arrhythmias. These irregular heartbeats need medical help. We’ll look at the heart’s electrical problems and what they mean.
Understanding Electrical Dysfunction
Electrical issues in the heart mean the heartbeat’s control is off. This can cause arrhythmias. These irregular heartbeats can be too fast, too slow, or not regular.
Common Causes of Electrical Dysfunction:
- Heart disease
- Electrolyte imbalances
- Genetic conditions
- Medications and toxins
A top cardiologist says, “Electrical heart disorders are a big problem worldwide.”
“The heart’s electrical system is a complex network that needs to work right to keep a normal rhythm.”
Conduction System Abnormalities
The heart’s conduction system sends out electrical signals for the heartbeat. Problems here can cause arrhythmias and other heart issues.
| Conduction System Abnormality | Description | Potential Consequences |
| AV Block | Delay or blockage of electrical impulses between atria and ventricles | Slow heart rate, potentially leading to fainting or heart failure |
| Bundle Branch Block | Delay or blockage of electrical impulses in the ventricles | Abnormal heart rhythms, potentially leading to arrhythmias |
Knowing about these conduction system problems is key for diagnosing and treating heart rhythm disorders. We’ll keep exploring the heart’s electrical issues and their impact on patient care.
What Causes Abnormal Heart Rhythm?
Arrhythmias can come from many sources. These include heart conditions, outside factors, and genes. Knowing these causes helps us find better ways to prevent and treat them.
Cardiac Disease Factors
Heart conditions are a big reason for abnormal heart rhythms. Diseases like coronary artery disease, heart failure, and cardiomyopathy mess with the heart’s electrical system. This can cause arrhythmias.
Common cardiac disease factors include:
- Coronary artery disease
- Heart failure
- Cardiomyopathy
- Valvular heart disease
Electrolyte Imbalances
Electrolytes like potassium, sodium, and calcium are key for the heart’s electrical activity. If these electrolytes are out of balance, it can mess with the heart’s rhythm. This often leads to arrhythmias.
| Electrolyte | Role in Heart Function | Effect of Imbalance |
| Potassium | Regulates heart rhythm | Hypokalemia can cause arrhythmias |
| Calcium | Influences heart contraction | Hypercalcemia can lead to arrhythmias |
Medication Effects and Toxicity
Some medicines can mess with the heart’s electrical system, causing arrhythmias. This includes drugs for other health issues and substances like caffeine and alcohol.
Examples of medications that can cause arrhythmias include:
- Antiarrhythmic medications (in some cases)
- Certain antibiotics
- Thyroid medications
Lifestyle and Environmental Triggers
Lifestyle choices and environmental factors can also lead to abnormal heart rhythms. Stress, too much alcohol, and toxins can all be culprits.
Lifestyle changes can help lower arrhythmia risk:
- Maintaining a healthy weight
- Exercising regularly
- Managing stress
Recognizing Life-Threatening Cardiac Rhythms
Knowing the signs of life-threatening heart rhythms can save lives. It’s important to spot these rhythms early to get help fast.
Warning Signs and Symptoms
Life-threatening heart rhythms show clear signs. Look out for palpitations, chest pain, shortness of breath, and fainting. Some people might not feel anything until it’s too late.
Here are symptoms that mean you should get help right away:
- Severe chest pain or discomfort
- Shortness of breath or trouble breathing
- Fainting or feeling like you’re going to faint
- Rapid or irregular heartbeat
- Dizziness or feeling lightheaded
Differentiating from Non-Fatal Arrhythmias
Not all heart rhythm problems are serious. We must tell the safe ones from the dangerous ones. Life-threatening arrhythmias often have a very fast or slow heart rate, or a very irregular rhythm.
To tell them apart, we look at:
- Underlying heart disease
- Symptom severity
- How well they respond to treatment
When to Seek Emergency Care
If you or someone else has symptoms of a life-threatening heart rhythm, get to the emergency room fast. Waiting too long can be deadly.
Go to the emergency room if you have:
- Chest pain or discomfort that lasts more than a few minutes
- Severe shortness of breath
- Fainting or loss of consciousness
- Severe dizziness or lightheadedness
Quick action can save lives. We must be ready to act fast when we see these signs.
Emergency Response and Treatment Protocols
Cardiac arrest from fatal arrhythmias needs quick and right care. The right treatment can greatly help survival rates and outcomes.
CPR and Early Defibrillation
CPR and early defibrillation are key in emergency care for cardiac arrest. CPR keeps blood flowing and oxygen to organs until the heart beats normally again.
Early defibrillation is key for arrhythmias like ventricular fibrillation (VF). It uses an electric shock to get a normal heartbeat back.
Advanced Cardiac Life Support (ACLS)
ACLS gives a clear plan for managing cardiac arrest. It includes giving medicines, managing airways, and using defibrillators. ACLS guides healthcare workers in quick decisions during emergencies.
Medication Interventions
Medicines are very important in treating cardiac arrest. Drugs like epinephrine and amiodarone help fix the heart rhythm or support it during resuscitation.
| Medication | Use in Cardiac Arrest | Dosage |
| Epinephrine | To support cardiac function | 1 mg IV/IO every 3-5 minutes |
| Amiodarone | To treat ventricular fibrillation or tachycardia | 300 mg IV/IO, followed by 150 mg |
Post-Resuscitation Care
After bringing a patient back, post-resuscitation care is key. It includes watching for problems, managing temperature, and giving support to avoid more heart issues.
Good emergency care and treatment plans are essential. They help save lives and reduce harm in cardiac arrest cases.
Modern Approaches to Fatal Arrhythmia Prevention
Preventing fatal arrhythmias requires a mix of strategies. We know more about these dangerous heart rhythms now. New methods help stop them before they start.
Risk Stratification Methods
Finding who’s at risk is key. Several methods help us do this, like:
- Electrocardiogram (ECG) analysis
- Heart rate variability assessment
- Left ventricular ejection fraction (LVEF) measurement
- Genetic testing for inherited conditions
Knowing who’s at risk lets us take steps to prevent these dangerous heart rhythms.
Implantable Cardioverter-Defibrillators
Implantable cardioverter-defibrillators (ICDs) are life-saving devices. They’re for people who’ve had a heart attack or are at high risk. They detect and fix dangerous heart rhythms.
ICDs send an electric shock to fix the heartbeat when needed. Studies have shown they cut down on deaths in high-risk groups.
Ablation Therapies
Ablation therapies destroy the bad electrical pathways in the heart. They treat arrhythmias like atrial fibrillation and ventricular tachycardia. Techniques like catheter ablation are used.
It’s a good option for those who don’t get better with medicine or have arrhythmias that keep coming back.
Genetic Testing and Counseling
Genetic testing is key for finding inherited conditions like long QT syndrome and Brugada syndrome. Early identification means we can take steps to prevent them.
Genetic counseling helps families with these conditions. It gives them the info and support they need to manage their risk.
By using these modern methods together, we can lower the number of fatal arrhythmias. This improves outcomes for those at risk.
Conclusion: Advances in Managing Fatal Arrhythmias
Managing fatal arrhythmias has seen big improvements, helping patients at risk of sudden cardiac death. At Liv Hospital, we aim to give top-notch healthcare to international patients. Our team uses the latest in cardiac care to help those with heart rhythm issues.
Dealing with fatal arrhythmias has gotten much better, thanks to new medical tech and treatment plans. We understand the heart’s rhythm problems well and use effective treatments. This helps lower the risk of fatal arrhythmias and improves patient results.
Our focus on advanced cardiac care shows in our modern facilities and skilled team. We keep up with the latest in cardiac care to ensure our patients get the best treatment. This is for heart rhythm disorders and fatal arrhythmias.
FAQ
What are the 4 fatal arrhythmias that can lead to sudden cardiac arrest?
The 4 fatal arrhythmias are ventricular fibrillation, pulseless ventricular tachycardia, asystole, and pulseless electrical activity. These life-threatening heart rhythms need immediate medical help to prevent cardiac arrest.
What is ventricular fibrillation and how is it recognized on an electrocardiogram (ECG)?
Ventricular fibrillation is a chaotic and dangerous arrhythmia. It shows a disorganized heart rhythm. On an ECG, it looks like a chaotic, irregular pattern with no P waves or QRS complexes.
What causes abnormal heart rhythms?
Abnormal heart rhythms can come from cardiac disease, electrolyte imbalances, medication effects, and lifestyle triggers. Knowing these causes helps in prevention and management.
What is the difference between pulseless ventricular tachycardia and ventricular fibrillation?
Pulseless ventricular tachycardia is a dangerous arrhythmia that can quickly lead to cardiac arrest. It has a fast heart rate with no pulse. Ventricular fibrillation is more disorganized, with no coordinated electrical activity.
How is asystole recognized on an ECG and what are its common causes?
Asystole is seen on an ECG as a flat line, showing no heart electrical activity. Common causes include cardiac disease, electrolyte imbalances, and medication toxicity.
What is pulseless electrical activity (PEA) and how is it managed?
Pulseless electrical activity is a complex arrhythmia with electrical activity on an ECG but no pulse. Managing it involves finding and treating the underlying cause, like cardiac tamponade or hypovolemia.
What are the warning signs and symptoms of life-threatening cardiac rhythms?
Warning signs and symptoms include chest pain, shortness of breath, dizziness, and palpitations. Recognizing these symptoms is key for quick medical action.
What is the importance of CPR and early defibrillation in managing cardiac arrest?
CPR and early defibrillation are vital in managing cardiac arrest from fatal arrhythmias. Quick treatment can greatly improve survival chances.
How can fatal arrhythmias be prevented?
Preventing fatal arrhythmias requires a multi-faceted approach. This includes risk stratification, implantable cardioverter-defibrillators, ablation therapies, and genetic testing and counseling.
What is the role of implantable cardioverter-defibrillators in preventing sudden cardiac death?
Implantable cardioverter-defibrillators (ICDs) can detect and correct life-threatening arrhythmias. They prevent sudden cardiac death in high-risk patients.
Are electrical problems with the heart serious?
Yes, electrical problems with the heart, like arrhythmias, can be serious and potentially life-threatening. Quick medical attention is essential for diagnosis and treatment.
What are the types of heart rhythm disorders?
Heart rhythm disorders include various arrhythmias, such as atrial fibrillation, ventricular tachycardia, and ventricular fibrillation, among others.
What is heart rhythm and how is it regulated?
Heart rhythm refers to the electrical activity that controls the heartbeat. It is regulated by the heart’s electrical system, involving complex interactions between cardiac cells and tissues.
References
- O’Rourke, M. F. (2018). Structure and function of systemic arteries: reflections on the vascular wall and blood flow. Vascular Medicine, 23(4), 316-323. https://pubmed.ncbi.nlm.nih.gov/30016416/