Vision loss from autoimmune disorders affects millions worldwide, often without warning. When the body’s immune system mistakenly targets its own healthy cells, it can lead to a wide range of health issues. This includes problems with vision. Wondering what autoimmune disease attacks the eyes? Get the facts on conditions that cause vision loss and learn the critical warning signs.
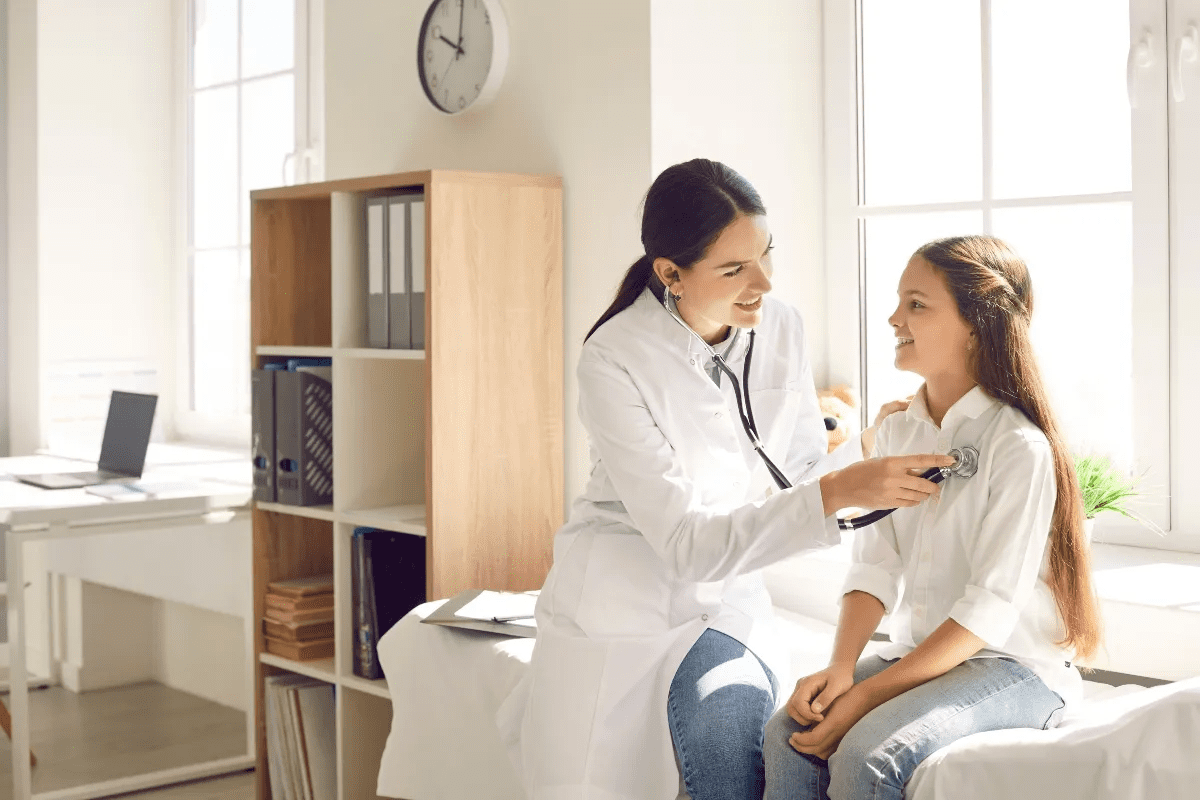
At Liv Hospital, we know that eye care needs specialized expertise and care focused on the patient. Many autoimmune diseases can harm the eyes and cause vision loss. It’s important to understand how these conditions affect eye health for early detection and treatment.
Key Takeaways
- Autoimmune diseases can cause significant vision problems.
- The immune system mistakenly attacks healthy cells, including those in the eyes.
- Early detection is key for effective treatment.
- Liv Hospital offers detailed eye care with specialized knowledge.
- Knowing how autoimmune diseases affect eye health is essential.
Understanding Autoimmune Diseases and Their Impact on Vision
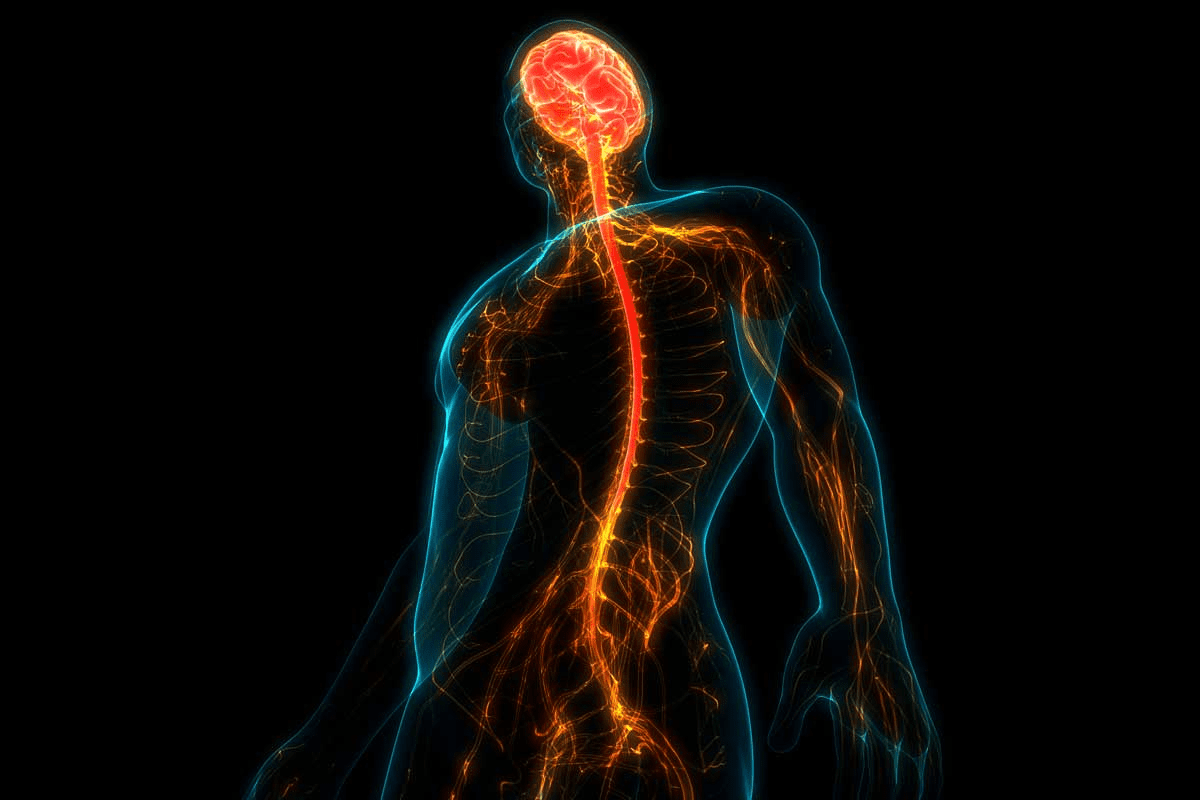
Autoimmune diseases can severely affect our vision, leading to serious issues if not treated. These diseases happen when our immune system attacks healthy body tissues, including the eyes. The eyes, being delicate and full of blood vessels, are often targeted by autoimmune attacks. If not treated, this can cause permanent damage.
How the Immune System Normally Protects the Eyes
The immune system is key in keeping our eyes safe from harm. It uses antibodies and immune cells to fight off infections. It’s designed to only attack harmful invaders, not our own tissues. The eyes, being very sensitive, have special protection to keep them working well.
When the Immune System Attacks Eye Tissues
In autoimmune diseases, the immune system mistakenly sees the eyes as threats. It then attacks the eye tissues, causing inflammation and damage. This can lead to vision problems. Uveitis is a major cause of preventable blindness, showing how critical it is to manage eye-related autoimmune diseases.
The effects of autoimmune diseases on the eyes vary. They can cause inflammation, tissue damage, and vision loss. Knowing these effects helps in finding effective treatments and preventing long-term damage.
Autoimmune Disease | Effect on the Eyes | Potential Vision Impact |
Uveitis | Inflammation of the uvea | Vision loss, blindness |
Neuromyelitis Optica | Damage to the optic nerves | Severe vision loss |
Sjögren’s Syndrome | Dry eyes, potentially leading to further complications | Discomfort, possible vision problems |
Uveitis: A Leading Cause of Preventable Blindness
Uveitis is an inflammatory condition that can cause blindness. It affects the uveal components of the eye. This inflammation in the middle layer of the eye can lead to serious vision problems.
Types of Uveitis and Their Effects on Vision
Uveitis is divided into types based on the affected area. Anterior uveitis affects the front part and is linked to diseases like ankylosing spondylitis. Intermediate uveitis impacts the middle, and posterior uveitis affects the back, leading to more severe vision issues.
Each type can cause different symptoms, from mild to severe vision loss. It can also be linked to other autoimmune diseases, making diagnosis and treatment harder.
Symptoms and Progression of Uveitis
Symptoms of uveitis vary among patients. Common signs include eye pain, redness, sensitivity to light, and blurred vision. Some may see floaters or have decreased vision.
If not treated, uveitis can cause cataracts, glaucoma, and retinal detachment. These complications can worsen vision problems.
Knowing the symptoms and how uveitis progresses is key for early treatment. Quick medical care can prevent long-term vision damage and improve outcomes.
Neuromyelitis Optica: When the Immune System Targets Optic Nerves
Neuromyelitis optica, also known as Devic’s disease, is an autoimmune disorder that mainly affects the eyes. It happens when the immune system mistakenly attacks the optic nerves. This leads to inflammation and damage.
We will look at how neuromyelitis optica is different from other eye diseases. We will also explore the specific vision loss patterns it causes.
Distinguishing Neuromyelitis Optica from Multiple Sclerosis
Neuromyelitis optica is often confused with multiple sclerosis (MS) because both can cause optic neuritis. But, there are key differences. Neuromyelitis optica has severe and selective attacks on the optic nerves and spinal cord. MS affects a wider range of central nervous system tissues.
One major difference is the presence of specific antibodies in neuromyelitis optica patients. These antibodies target a protein called aquaporin-4. The presence of these antibodies is a strong indicator of neuromyelitis optica, not MS.
Characteristics | Neuromyelitis Optica | Multiple Sclerosis |
Primary Areas Affected | Optic nerves and spinal cord | Broad range of CNS tissues |
Presence of Aquaporin-4 Antibodies | Common | Rare |
Severity of Optic Neuritis | Often severe | Variable |
Vision Loss Patterns in Neuromyelitis Optica
The vision loss in neuromyelitis optica can be severe and affect both eyes. It often presents with episodes of optic neuritis. This can cause rapid vision loss and eye pain.
The severity and permanence of vision loss vary. Timely treatment is key to prevent long-term damage.
In some cases, patients may have a single episode of optic neuritis. Others may have recurrent attacks. The frequency and severity of these episodes can significantly impact vision.
Understanding the patterns of vision loss in neuromyelitis optica is essential. It helps in managing the condition effectively. Early intervention is key to preserving vision and improving patient outcomes.
Sjögren’s Syndrome: Beyond Dry Eyes to Vision Complications
Sjögren’s Syndrome is a serious autoimmune disease that affects the eyes. It mainly causes dry eye due to the immune system attacking the lacrimal glands.
This condition not only causes discomfort but can also lead to serious vision complications if not properly managed. We will explore how Sjögren’s Syndrome affects the eyes and the long-term risks it poses.
Attack on Lacrimal Glands
Sjögren’s Syndrome attacks the lacrimal glands and mucous membranes. These glands are key for tear production. When they are damaged, tear production drops, causing dry, irritated eyes.
- Dry eye symptoms include a gritty sensation, blurred vision, and increased sensitivity to light.
- If left untreated, dry eye can lead to more severe complications, including damage to the cornea.
Long-term Vision Risks
Untreated dry eye from Sjögren’s Syndrome can lead to several long-term vision risks. These include:
- Corneal Damage: The cornea can become ulcerated or scarred, potentially leading to vision loss.
- Chronic Discomfort: Persistent dry eye can cause ongoing discomfort and affect quality of life.
- Increased Risk of Infections: Dry eyes are more susceptible to infections due to the lack of protective tear film.
Understanding the risks of Sjögren’s Syndrome and its impact on the eyes is key to managing the condition. Recognizing symptoms early and getting proper treatment can help avoid long-term vision problems.
Multiple Sclerosis and Optic Neuritis
Multiple sclerosis is a chronic autoimmune disease. It often shows symptoms early, including vision problems. Eye doctors play a key role in spotting these cases.
Recognizing MS-Related Vision Changes
Optic neuritis is a big vision problem in MS. It’s an inflammation of the optic nerve that can cause vision loss. Spotting the signs early is key for treatment.
Symptoms include:
- Blurred vision
- Loss of vision in one eye
- Pain on eye movement
- Impaired color vision
These vision changes can signal MS. Knowing the connection between autoimmune disease eyes and optic neuritis is important.
Recovery Patterns and Permanent Vision Damage
Recovery from optic neuritis varies. Some see their vision return fully, while others face lasting vision issues. The severity of the inflammation and treatment success play big roles.
Some people may not get their vision back. Others might face recurring problems. Managing MS is key to protecting your vision.
In summary, the link between MS and vision issues, like optic neuritis, stresses the need for eye care. It’s vital for preventing long-term vision loss.
Thyroid Eye Disease: When Graves’ Disease Affects Vision
When the immune system attacks the eye’s tissues, it can cause Thyroid Eye Disease. This is often linked to Graves’ disease. It leads to swelling and inflammation around the eye, causing bulging eyes and vision issues.
Mechanisms of Eye Bulging and Pressure
The immune system’s attack on the orbital tissues causes swelling. This swelling makes the eyes bulge out. The bulging happens because the inflamed tissues and fat behind the eye expand, pushing the eyeball forward.
The swelling and increased pressure can cause double vision and, in severe cases, vision loss. It’s important to understand these symptoms to manage them effectively.
Symptom | Cause | Potential Complication |
Bulging Eyes (Proptosis) | Inflammation and swelling of orbital tissues | Exposure Keratopathy, leading to corneal damage |
Double Vision (Diplopia) | Swelling and inflammation of extraocular muscles | Permanent vision impairment if not treated |
Vision Loss | Optic nerve compression due to increased orbital pressure | Permanent blindness if not promptly addressed |
Managing Vision Threats in Thyroid Eye Disease
Managing Thyroid Eye Disease needs a multi-faceted approach. This includes controlling Graves’ disease, reducing inflammation, and treating eye symptoms directly.
Treatments may include medications like corticosteroids to reduce inflammation. Sometimes, surgery is needed to relieve pressure on the optic nerve or correct eyelid retraction.
Early diagnosis and treatment are key to preventing vision damage. Patients with Graves’ disease should be closely monitored for signs of Thyroid Eye Disease.
What Autoimmune Disease Attacks the Eyes Through Joint Conditions
Autoimmune diseases can harm the eyes when they attack the joints. Conditions like rheumatoid arthritis and systemic lupus erythematosus can lead to eye problems. We will look at how these diseases affect the eyes and the vision issues they can cause.
Rheumatoid Arthritis and Scleritis
Rheumatoid arthritis (RA) mainly affects the joints but can also harm the eyes. It can cause scleritis, a severe inflammation of the eye’s white outer layer. Scleritis can cause intense pain, redness, and can damage vision permanently if not treated.
Scleritis Symptoms:
- Severe eye pain
- Redness and swelling
- Sensitivity to light
- Vision disturbances
It’s important to catch and treat scleritis early to avoid lasting damage. Doctors may use anti-inflammatory or immunosuppressive drugs to treat it.
Systemic Lupus Erythematosus and Ocular Manifestations
Systemic lupus erythematosus (SLE) is an autoimmune disease that can affect many parts of the body, including the eyes. SLE can cause eye problems ranging from mild dry eye to severe inflammation of the retina.
Ocular Manifestation | Description |
Dry Eye | Reduced tear production leading to eye discomfort |
Retinal Vasculitis | Inflammation of the blood vessels in the retina, potentially causing vision loss |
Scleritis | Inflammation of the sclera, similar to that seen in RA |
Regular eye exams are key for SLE patients to catch and treat eye problems early.
It’s important to understand how autoimmune joint diseases can affect the eyes. By recognizing these risks, doctors can take steps to protect vision and improve patients’ lives.
Rare Autoimmune Eye Conditions
Rare autoimmune eye conditions can severely harm vision if not treated. They often pose unique challenges in diagnosis and treatment.
Autoimmune Retinopathy
Autoimmune retinopathy is a rare condition where the immune system attacks the retina. This can lead to severe vision loss. It may occur alone or with other autoimmune diseases.
Symptoms and Diagnosis: Patients often report sudden vision loss, which can affect both eyes. Tests like electroretinography and imaging studies help diagnose retinal damage.
Treatment Approaches: Treatment usually involves immunosuppressive therapy to stop the disease from getting worse. Early treatment is key to saving vision.
Mooren’s Ulcer and Other Uncommon Conditions
Mooren’s ulcer is a rare, painful condition that affects the cornea. It is thought to be caused by an autoimmune response.
Condition | Primary Symptoms | Treatment Options |
Autoimmune Retinopathy | Sudden vision loss, often bilateral | Immunosuppressive therapy |
Mooren’s Ulcer | Painful corneal ulceration | Topical corticosteroids, immunosuppression |
Other rare autoimmune eye conditions include sympathetic ophthalmia and autoimmune corneal diseases. Each condition presents unique challenges in diagnosis and treatment.
We understand the complexity and severity of these rare autoimmune eye conditions. Accurate diagnosis and timely treatment are essential for managing these conditions effectively.
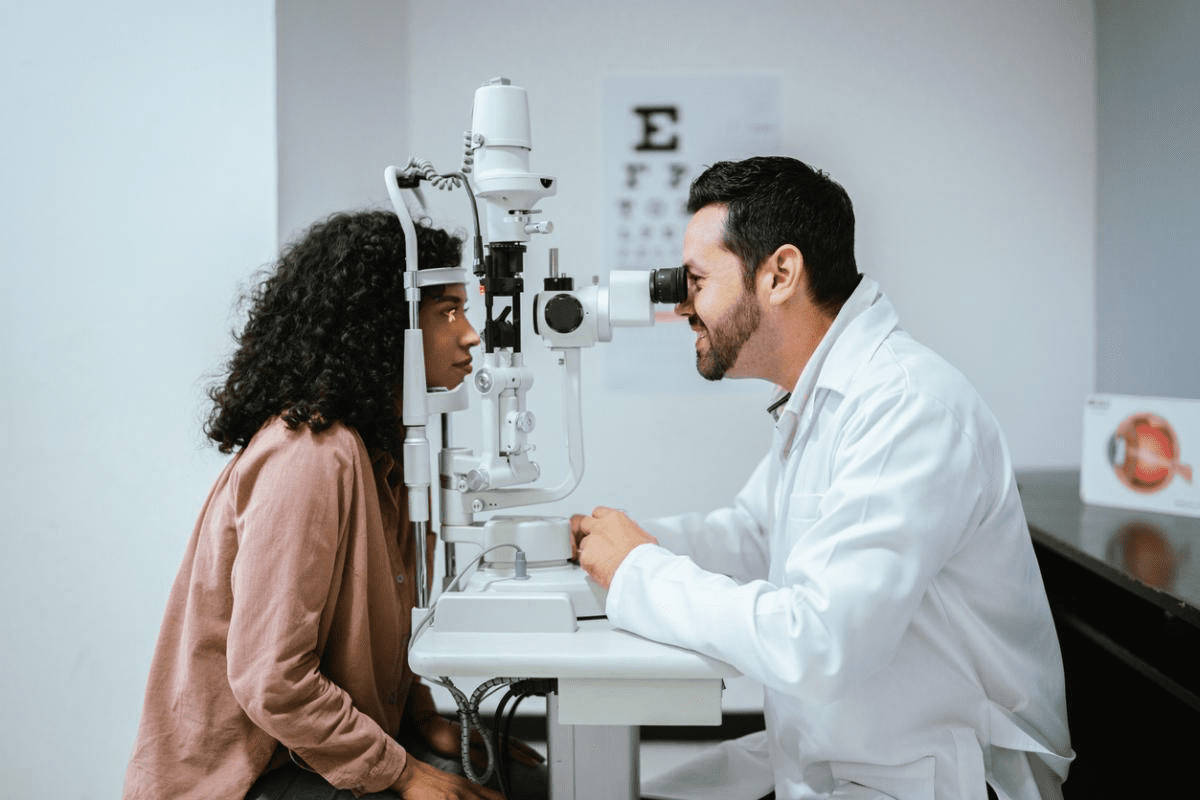
Diagnosis of Autoimmune Eye Diseases
Diagnosing autoimmune eye diseases is complex. It requires a detailed approach. Conditions like uveitis and neuromyelitis optica can cause severe vision loss if not treated quickly and correctly.
We use many tools to find these diseases. The process includes a detailed medical history, eye exams, lab tests, and imaging studies.
Specialized Eye Examinations
Eye exams are key in diagnosing these diseases. They include:
- Visual acuity tests to check vision sharpness
- Slit-lamp exams to look at the eye’s front part
- Ophthalmoscopy to check the retina and optic nerve
- Optical coherence tomography (OCT) to see the retina’s layers
These exams help spot inflammation and damage in the eyes. They also find other signs of autoimmune diseases.
Laboratory Tests and Imaging
Lab tests and imaging are vital for confirming a diagnosis. They help us understand how far the disease has spread. Common tests include:
Test | Purpose |
Blood tests | To find inflammatory markers and autoimmune antibodies |
Fluorescein angiography | To see blood flow and find vascular issues |
MRI scans | To check the optic nerve and other eye structures |
Experts say, “Early diagnosis and treatment of autoimmune eye diseases are critical to preventing irreversible vision loss.”
This shows why a detailed diagnostic approach is so important.
By combining eye exams, lab tests, and imaging, we can accurately diagnose autoimmune eye diseases. This helps us create an effective treatment plan.
Treatment Approaches for Autoimmune Eye Diseases
Autoimmune eye diseases need a mix of treatments to fight inflammation and save vision. Each treatment plan is made for the specific disease affecting the eyes.
Conventional Treatments and Medications
Medications that reduce inflammation and calm the immune system are key. Corticosteroids are often the first choice because they work well against inflammation. But, they can have side effects, so doctors look for other options too.
A leading expert says, “The goal is not just to treat symptoms but to find the root cause of the autoimmune response.”
“Understanding the pathophysiology of autoimmune eye diseases is key to finding new treatments.”
Biologic Therapies and Emerging Treatments
Biologic therapies are a big step forward in treating autoimmune eye diseases. They target specific parts of the immune system, giving a more focused treatment than usual drugs. Biologic agents have shown to reduce inflammation and slow disease progress in conditions like uveitis and scleritis.
New treatments like gene therapy and new biologic agents are coming. They offer hope for better managing autoimmune eye diseases in the future.
Managing Vision Loss and Rehabilitation
Even with new treatments, some people with autoimmune eye diseases may lose vision. It’s important to manage this to keep their quality of life good. Rehabilitation services, like low vision aids and occupational therapy, help patients adjust to vision loss.
We stress the need for a team approach to care. This includes ophthalmologists, rheumatologists, and rehabilitation specialists to meet the complex needs of patients with autoimmune eye diseases.
Conclusion: Living with Autoimmune Eye Conditions
Managing autoimmune eye conditions needs a full plan to keep your vision safe. Diseases like uveitis, neuromyelitis optica, and thyroid eye disease can cause serious vision loss. It’s vital to treat them right away.
We’ve talked about different eye autoimmune diseases and how they affect your sight. Early diagnosis and treatment are key. It takes teamwork between patients, eye doctors, and other health experts for the best results.
Knowing how autoimmune eye disease works and taking care of yourself can reduce risks. Keeping an eye on your condition, following treatment plans, and making healthy lifestyle choices are important. These steps help protect your eye health.
We aim to offer top-notch healthcare and support for those with autoimmune eye conditions. Together, we can make life better for those facing these tough challenges.
FAQ
What is an autoimmune disease and how does it affect the eyes?
An autoimmune disease happens when the body’s immune system attacks its own cells. This can lead to inflammation and damage in the eyes. It can cause vision problems.
What is uveitis and how does it affect vision?
Uveitis is inflammation in the middle layer of the eye. It’s a big cause of blindness worldwide. If not treated, it can lead to vision loss.
What is neuromyelitis optica and how does it differ from multiple sclerosis?
Neuromyelitis optica is a rare disease that mainly affects the optic nerves. It causes severe vision loss. It’s different from multiple sclerosis because it targets the optic nerves more.
How does Sjögren’s syndrome affect the eyes?
Sjögren’s syndrome mainly affects the glands that make tears. This leads to dry eyes. If not managed, it can cause vision problems.
Can multiple sclerosis cause vision problems?
Yes, multiple sclerosis can affect the optic nerves. This leads to optic neuritis. It can cause vision changes, with some chance of recovery or permanent damage.
What is thyroid eye disease and how does it affect vision?
Thyroid eye disease is when the immune system attacks the eye tissues. It causes bulging eyes and vision problems. Proper management is needed to protect vision.
How do autoimmune joint conditions like rheumatoid arthritis affect the eyes?
Autoimmune joint conditions, like rheumatoid arthritis, can harm the eyes. They can cause inflammation and vision problems.
What are some rare autoimmune eye conditions?
Rare autoimmune eye conditions include autoimmune retinopathy and Mooren’s ulcer. They can affect vision and need special treatment.
How are autoimmune eye diseases diagnosed?
Diagnosing autoimmune eye diseases needs a detailed approach. It involves eye exams, lab tests, and imaging to find these conditions.
What are the treatment options for autoimmune eye diseases?
Treatments for autoimmune eye diseases vary. They include medicines, biologic therapies, and new treatments. The goal is to manage vision loss and help with recovery.
Can autoimmune eye diseases be managed effectively?
Yes, with the right care, people can manage their autoimmune eye conditions. It’s important to have a complete care plan for eye health.
What is the importance of managing vision loss in autoimmune eye diseases?
Managing vision loss is key in autoimmune eye diseases. It greatly affects a person’s life. Rehabilitation efforts can help lessen the impact of vision loss.