Discover what causes atherosclerosis, including major risk factors like cholesterol and blood pressure.
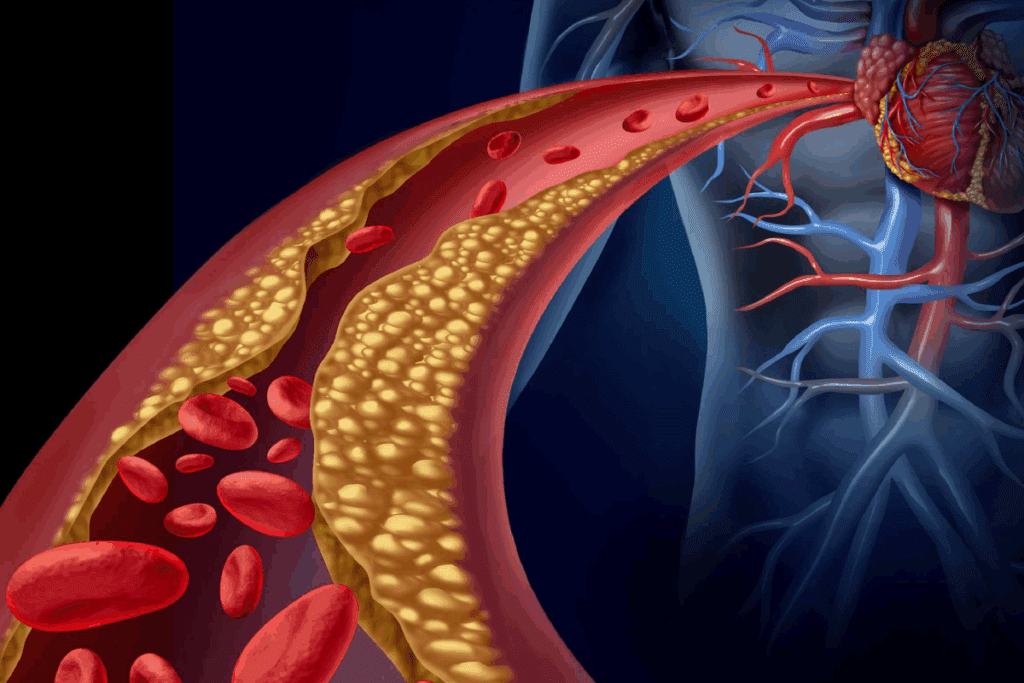
Atherosclerosis is a condition where plaque builds up inside the walls of arteries. This buildup narrows and hardens the arteries. It can restrict blood flow to vital organs, leading to serious cardiovascular diseases.
Understanding the risks and recognizing the signs early on can be lifesaving. Trusted medical institutions like LivHospital stress the importance of early detection and prevention. They say it’s key to managing this condition effectively.
Exploring the causes and risk factors of atherosclerosis shows it develops silently over years. Often, there are no symptoms until it’s too late.
Key Takeaways
- Atherosclerosis is a silent condition that can lead to serious cardiovascular diseases.
- Plaque buildup in arterial walls narrows and hardens arteries.
- Early detection and prevention are key in managing atherosclerosis.
- Recognizing risk factors early can save lives.
- Trusted medical institutions emphasize the importance of preventive care.
Understanding Atherosclerosis: The Silent Arterial Threat
As we get older, atherosclerosis can quietly grow, often without symptoms until later. This condition is marked by plaque buildup in the arteries, causing heart problems. Knowing about atherosclerosis is key to preventing and managing it.
The Progressive Nature of Plaque Buildup
Atherosclerosis is a disease that gets worse over time. It starts with plaque building up in the arteries. This plaque is made of fat, cholesterol, calcium, and more.
As plaque grows, it can harden or burst, causing serious health problems.
The disease begins with endothelial dysfunction. This is when the blood vessel’s inner lining gets damaged. This damage lets lipids get into the artery wall and build up.
As plaque grows, it narrows the artery. This can block blood flow to important organs.
How Atherosclerosis Develops Over Decades
Atherosclerosis often starts in childhood or teens and grows over decades. It’s influenced by genetics, lifestyle, and environment. Early action is vital to stop it from getting worse.
Factors like high cholesterol, high blood pressure, smoking, and diabetes speed up the disease. Knowing these risk factors helps us find ways to slow it down.
The Prevalence and Impact on Western Societies
In Western societies, atherosclerosis is a big health problem. It leads to many heart issues and deaths. By 65, most people have some artery changes.
This illustrates the importance of public health efforts in combating it. These efforts aim to lower risk factors.
Atherosclerosis also affects healthcare systems and economies. Preventive steps like changing lifestyle and managing risk factors are essential. They help lessen the disease’s impact.
Atherosclerosis vs. Arteriosclerosis: Key Differences Explained

Atherosclerosis and arteriosclerosis are often confused, but they mean different things. Atherosclerosis is a specific form of arteriosclerosis. Knowing the difference helps patients understand their heart health better.
Defining Both Conditions
Arteriosclerosis is when the arteries get hard and stiff. This can happen because of aging, high blood pressure, or other diseases. Atherosclerosis, on the other hand, is when plaque builds up inside the arteries, making them narrow and hard. So, all atherosclerosis is arteriosclerosis, but not all arteriosclerosis is atherosclerosis.
Why All Atherosclerosis is Arteriosclerosis, But Not Vice Versa
The main difference is in how the arteries change. Atherosclerosis is when lipids, inflammatory cells, and other substances build up on the artery walls, forming plaques. Arteriosclerosis, on the other hand, can be caused by different things, like medial calcification. Knowing this helps doctors understand the problem and choose the right treatment.
Diagnostic Distinctions for Patients
To diagnose atherosclerosis, doctors use tests like ultrasound, CT scans, or angiography to see the plaque. For arteriosclerosis, they might check how stiff the arteries are or look for calcification. Understanding these differences helps patients see why they’re getting a certain treatment.
How Atherosclerosis Affects Different Body Systems
Atherosclerosis is a widespread condition that can harm many arteries. It causes different symptoms based on where and how severe it is. This means it can lead to a variety of health issues, depending on the affected arteries.
Coronary Artery Disease: When Atherosclerosis Attacks the Heart
When atherosclerosis hits the coronary arteries, it causes coronary artery disease (CAD). This disease reduces blood flow to the heart. It can lead to angina pectoris, chest pain, or even a myocardial infarction (heart attack) if blood flow stops completely.
CAD often starts silently and shows symptoms only when it’s advanced. It’s important to know the risk factors and manage them to prevent CAD.
Cerebrovascular Impact: Strokes and TIAs
Atherosclerosis in the brain’s arteries can cause cerebrovascular disease. This can lead to a stroke or transient ischemic attack (TIA). A stroke happens when brain blood flow is cut off, causing brain tissue damage. TIAs are temporary and don’t usually cause lasting harm.
Managing risk factors is key to avoiding these serious brain conditions.
Peripheral Artery Disease: Extremity Complications
Atherosclerosis can also harm the arteries to the limbs, causing peripheral artery disease (PAD). PAD leads to intermittent claudication, pain in the legs when walking. Severe cases can cause critical limb ischemia, leading to gangrene and amputation if not treated.
It’s important to recognize PAD symptoms and treat the underlying atherosclerosis to prevent these serious issues.
Renal Artery Stenosis: Kidney Damage Pathways
Atherosclerosis can also narrow the renal arteries, leading to renal artery stenosis. This can cause renovascular hypertension, high blood pressure, and ischemic nephropathy, where kidneys don’t work right due to poor blood flow.
Managing atherosclerosis and its effects on the kidneys is key to keeping kidneys working and controlling blood pressure.
What Causes Atherosclerosis: The Inflammatory Process Explained
To understand atherosclerosis, we must look at the inflammation that leads to plaque buildup in arteries. It’s not just about lipids; it’s an active process involving many cells and molecules.
The Initial Endothelial Injury
The first step in atherosclerosis is damage to the endothelium, the blood vessel’s inner layer. This damage can come from high blood pressure, smoking, and high LDL cholesterol. When the endothelium is hurt, it lets lipids and inflammatory cells into the artery wall.
This damage starts an inflammatory response. Monocytes and other leukocytes stick to the endothelium and move into the intima. There, they become macrophages, taking in lipids and turning into foam cells.
Cholesterol Deposition and Plaque Formation
As inflammation goes on, cholesterol starts to build up, leading to plaque. LDL cholesterol, when oxidized, is key in this process. Lipid-filled macrophages and smooth muscle cells moving into the intima make the plaque grow.
Plaque growth is complex, involving lipids, smooth muscle cell growth, matrix production, and calcification. Over time, this narrows the artery and cuts off blood flow to important organs.
The Role of Inflammation in Disease Progression
Inflammation is not just a side effect of atherosclerosis; it drives the disease. The ongoing inflammation in the plaque makes it unstable, increasing the risk of rupture. A rupture can cause sudden blockages, like heart attacks or strokes.
Inflammation’s role in atherosclerosis is clear, with markers like C-reactive protein (CRP) showing up in cardiovascular disease. CRP is linked to a higher risk of heart events.
From Fatty Streaks to Complex Lesions
The move from fatty streaks to complex lesions is key in atherosclerosis. Fatty streaks are early lesions filled with lipid-laden macrophages. They can grow into complex lesions with a fibrous cap, lipid core, and calcification over time.
Complex lesions are more inflamed, unstable, and risky. Knowing how they form helps in finding ways to prevent and treat atherosclerosis.
Risk Factor #1: Dyslipidemia and Cholesterol Imbalance
Dyslipidemia is a major risk factor for atherosclerosis. It happens when cholesterol and triglycerides in the blood are not balanced. This imbalance can cause plaque to build up in arteries.
Understanding LDL vs. HDL Cholesterol
Cholesterol is a fat in the blood that our bodies need. But, not all cholesterol is the same. LDL (Low-Density Lipoprotein) cholesterol, or “bad” cholesterol, can cause plaque in arteries. On the other hand, HDL (High-Density Lipoprotein) cholesterol, or “good” cholesterol, helps remove excess cholesterol from the blood and artery walls.
Medical Expert, a cardiologist, once said,
“The balance between LDL and HDL cholesterol is key to avoiding atherosclerosis.”
Triglycerides and Their Impact
Triglycerides are fats in the blood. High levels of triglycerides can also lead to atherosclerosis. When we eat more calories than we burn, our body turns the extra into triglycerides. High triglyceride levels increase the risk of heart disease.
Genetic Factors in Cholesterol Regulation
Genetics play a big role in our lipid profiles. Some people may have conditions like familial hypercholesterolemia, leading to very high LDL cholesterol. Knowing your family history is important for understanding your risk of dyslipidemia and atherosclerosis.
Dietary Influences on Blood Lipid Profiles
What we eat affects our blood lipid levels. Eating too much saturated and trans fats can increase LDL cholesterol. But, eating fruits, vegetables, and whole grains can improve HDL levels and overall lipid profiles. It’s vital to eat a balanced diet to lower the risk of dyslipidemia.
By knowing what causes dyslipidemia, we can take steps to manage cholesterol levels. This can help reduce the risk of atherosclerosis.
Risk Factor #2: Hypertension’s Role in Arterial Damage
High blood pressure damages arterial walls, leading to atherosclerosis. We’ll look at how high blood pressure speeds up atherosclerosis. We’ll also talk about why managing blood pressure is key to avoiding heart disease.
How High Blood Pressure Accelerates Atherosclerosis
Hypertension affects arterial walls in several ways. Increased pressure damages the inner lining of arteries. This makes arteries more likely to collect lipids and inflammatory cells.
The shear stress from turbulent blood flow also plays a role. It can cause atherosclerotic plaques to form.
Hypertension and atherosclerosis are linked in a cycle. High blood pressure can cause atherosclerosis, and atherosclerosis can make blood pressure worse. This cycle is dangerous.
The Vicious Cycle: Atherosclerosis and Worsening Hypertension
The cycle between hypertension and atherosclerosis is vicious. Atherosclerosis makes arteries stiffer, raising blood pressure. This higher blood pressure then speeds up atherosclerosis, creating a cycle.
It’s important to break this cycle to manage heart risk. Keeping blood pressure under control is key to slowing atherosclerosis and reducing heart disease risk.
Blood Pressure Targets for Prevention
To stop atherosclerosis from getting worse, managing blood pressure is essential. The American Heart Association suggests keeping blood pressure below 130/80 mmHg. This requires lifestyle changes and, if needed, medication.
- Lifestyle changes include eating right, exercising, managing weight, and reducing stress.
- Medications like ACE inhibitors, ARBs, diuretics, and calcium channel blockers are also used.
Understanding hypertension’s role in atherosclerosis is vital. Effective blood pressure management can greatly reduce heart disease risk and improve health outcomes.
Risk Factor #3: Diabetes and Metabolic Syndrome
Diabetes and metabolic syndrome are key risk factors for atherosclerosis. Diabetes mellitus can lead to heart disease death, mainly due to faster atherosclerosis. We’ll look at how diabetes and metabolic syndrome cause vascular damage through insulin resistance and other factors.
Insulin Resistance and Vascular Damage
Insulin resistance is a big problem in type 2 diabetes and metabolic syndrome. It causes many metabolic changes that harm the blood vessels, leading to atherosclerosis. Insulin resistance is linked to more inflammation, oxidative stress, and bad lipid profiles, speeding up plaque buildup.
The damage from insulin resistance is complex. It harms the blood vessel lining, increases sticky molecules, and makes vessels more open. These changes let lipids and inflammatory cells get into the artery walls, starting and keeping atherosclerosis going.
Glycation End Products and Their Effects
Advanced glycosylation end-products (AGEs) form when blood sugar sticks to proteins or fats. They play a big role in atherosclerosis in diabetics. AGEs build up in artery walls, causing more oxidative stress and inflammation, speeding up plaque growth and instability.
The AGE receptor (RAGE) is key in AGE effects. When AGEs bind to RAGE, it starts a chain of inflammatory signals, adding to vascular damage. This shows how diabetes and atherosclerosis are closely linked.
Why Diabetics Face Higher Atherosclerotic Risk
Diabetics are at higher risk for atherosclerosis because of many factors. These include constant high blood sugar, insulin resistance, and bad lipid levels. Managing diabetes well is key to controlling atherosclerosis, along with other heart disease risk factors.
| Risk Factor | Effect on Atherosclerosis |
| Insulin Resistance | Increases inflammation and oxidative stress, promoting plaque formation. |
| Hyperglycemia | Leads to the formation of AGEs, accelerating vascular damage. |
| Dyslipidemia | Alters lipid profiles, increasing the risk of plaque development. |
Knowing these factors is key to fighting atherosclerosis in diabetics. By managing diabetes and its related metabolic issues, we can lower heart disease risks.
Risk Factors #4 and #5: Smoking and Obesity
Lifestyle choices like smoking and obesity greatly increase the risk of atherosclerosis. These factors can lead to heart disease on their own. But when combined, they raise the risk even more. We’ll look at how smoking and obesity impact atherosclerosis and the reasons behind it.
Tobacco’s Direct Damage to Arterial Walls
Smoking is a big risk for atherosclerosis. It harms the blood vessel walls, making them more likely to block. Tobacco smoke changes how blood vessels work, leading to more inflammation and plaque.
Stopping smoking is key to lowering atherosclerosis risk. Quitting can greatly reduce heart disease risk in just a few years.
How Smoking Accelerates Plaque Formation
Smoking speeds up plaque buildup in several ways. It raises “bad” cholesterol and lowers “good” cholesterol. It also causes more inflammation in blood vessel walls, adding to plaque.
Obesity’s Metabolic Consequences
Obesity is a big risk for atherosclerosis. It often comes with metabolic syndrome, raising the risk of diabetes and heart disease. Visceral fat, in particular, is active and releases inflammatory markers that harm blood vessels.
| Risk Factor | Impact on Atherosclerosis |
| Smoking | Damages arterial walls, increases LDL cholesterol, and promotes inflammation. |
| Obesity | Associated with metabolic syndrome, increases inflammatory markers, and contributes to plaque formation. |
Visceral Fat and Inflammatory Markers
Visceral fat plays a big role in insulin resistance and metabolic syndrome. It releases inflammatory cytokines like C-reactive protein (CRP) and interleukin-6 (IL-6). These cytokines drive inflammation that leads to atherosclerosis. Losing visceral fat through diet and exercise can help reduce this risk.
Understanding how smoking and obesity lead to atherosclerosis helps us fight it better. Changing our lifestyle, like quitting smoking and managing weight, is essential for preventing atherosclerosis.
Risk Factors #6 and #7: Sedentary Lifestyle and Poor Diet
Regular exercise and a balanced diet are key to avoiding atherosclerosis. This condition quietly harms our heart health. It shows how changing our lifestyle can help a lot.
Exercise’s Protective Effects Against Atherosclerosis
Exercise is a strong ally against atherosclerosis. It boosts blood flow, lowers blood pressure, and improves cholesterol levels. Moderate-intensity exercise, like brisk walking, cycling, or swimming, for at least 150 minutes a week is advised for adults to lower heart disease risk.
The Minimum Activity Requirements for Prevention
To get the most from exercise, knowing the basics is key. The American Heart Association suggests at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity weekly. Adding strength training exercises at least twice a week can also boost heart health.
Dietary Patterns That Promote Arterial Health
Eating lots of fruits, vegetables, whole grains, and lean proteins is good for your arteries. The Mediterranean diet, rich in these foods, can lower heart disease risk. It focuses on monounsaturated fats, like those in olive oil, and less on saturated and trans fats.
Specific Foods and Nutrients to Avoid
Some foods can increase atherosclerosis risk. Limit foods high in saturated fats, trans fats, and cholesterol. Stay away from processed and fried foods, and those with lots of added sugars and salt. Avoiding these can greatly lower your risk of atherosclerosis.
Conclusion: Comprehensive Approach to Atherosclerosis Prevention
Stopping atherosclerosis needs a plan that covers all its main risks. Knowing what causes and affects this condition helps us act early to keep our hearts healthy.
To prevent atherosclerosis, we must change our lifestyle and get medical help. Keeping cholesterol levels in check, managing blood pressure, and eating well are key. A diet full of fruits, veggies, and whole grains is best.
Exercising regularly, like walking, is also vital. Staying away from tobacco and keeping a healthy weight are important too. These steps help keep your heart in top shape.
Most people can stop or slow atherosclerosis by following these steps. It’s important to work with doctors to make a plan that fits you. This plan helps manage risks and keeps your heart healthy.
By taking a full approach to prevention, we can control our heart health. This reduces the chance of heart problems and makes life better.
FAQ:
What is atherosclerosis?
Atherosclerosis is a condition where plaque builds up in artery walls. This can lead to heart diseases.
What is the difference between atherosclerosis and arteriosclerosis?
Atherosclerosis is a specific type of arteriosclerosis. It’s when plaque builds up in arteries. Arteriosclerosis is the hardening of arteries. So, all atherosclerosis is arteriosclerosis, but not all arteriosclerosis is atherosclerosis.
How does atherosclerosis develop?
Atherosclerosis starts with plaque buildup in arteries. It takes decades to develop and can cause serious health problems as people get older.
What are the risk factors for atherosclerosis?
Risk factors include high cholesterol, high blood pressure, diabetes, smoking, obesity, not being active, and eating poorly.
How does dyslipidemia contribute to atherosclerosis?
Dyslipidemia, or an imbalance of cholesterol and triglycerides, helps plaque form. This is a major contributor to atherosclerosis.
What is the role of hypertension in atherosclerosis?
High blood pressure damages arteries and speeds up atherosclerosis. This creates a cycle that makes both conditions worse.
How does diabetes increase the risk of atherosclerosis?
Diabetes raises the risk of atherosclerosis through insulin resistance and damage from glycation end products. These harm blood vessels.
What is the impact of smoking on atherosclerosis?
Smoking damages artery walls and speeds up plaque buildup. This increases the risk of atherosclerosis.
How can lifestyle changes prevent atherosclerosis?
Being active and eating well can prevent atherosclerosis. They reduce the risk factors for the condition.
What are the benefits of exercise in preventing atherosclerosis?
Exercise protects against atherosclerosis. Even a little bit of activity can help prevent it.
What dietary patterns promote arterial health?
Eating lots of fruits, vegetables, and whole grains promotes arterial health. It also lowers the risk of atherosclerosis.
References:
Pahwa, R., & Jialal, I. (2023). Atherosclerosis. In StatPearls. StatPearls Publishing.https://www.ncbi.nlm.nih.gov/books/NBK507799/


































