At Liv Hospital, our ophthalmology team sees patients with blurred optic disc margins. This finding can mean serious health issues or just normal variations. It’s very important to understand what it means for your eyes and brain health.
Papilledema is a big worry. It’s when the optic disc swells because of too much pressure inside the brain. We know many things can cause this, so we use detailed checks and scans to find out.
Key Takeaways
- Blurred optic disc margins can signal serious underlying conditions or benign variations.
- Accurate diagnosis is critical to protect vision and identify life-threatening conditions.
- Papilledema is a condition characterized by swelling of the optic disc due to elevated ICP.
- Multiple causes can lead to papilledema, requiring a thorough examination and imaging.
- Early detection and proper management are essential for preserving vision and overall health.
Understanding the Optic Disc and Normal Anatomy
To understand blurred optic disc margins, we need to know the optic disc’s normal anatomy. The optic disc, or optic nerve head (ONH), is where optic nerve fibers leave the eye. It’s key for our vision.
Structure and Function of the Optic Disc
The optic disc has retinal ganglion cell axons and glial cells. It’s covered by all three meningeal layers, connecting to the brain’s subarachnoid space. This structure is vital for sending visual info to the brain. It’s usually round or oval with a central depression called the physiological cup.
The nasal margin of the optic disc often blurs first in conditions like papilledema. This is a key sign of increased intracranial pressure.
Normal Variations in Optic Disc Appearance
Optic discs can look different from person to person. Size, cup depth, and neuroretinal rim shape vary. For example, some have a bigger physiological cup than others.
Characteristic | Normal Variation | Clinical Significance |
Size of Optic Disc | Can range from small to large | Affects cup-to-disc ratio interpretation |
Depth of Physiological Cup | Variability in cupping | Important for diagnosing glaucoma |
Neuroretinal Rim | Variability in thickness and configuration | Thinning may indicate glaucoma |
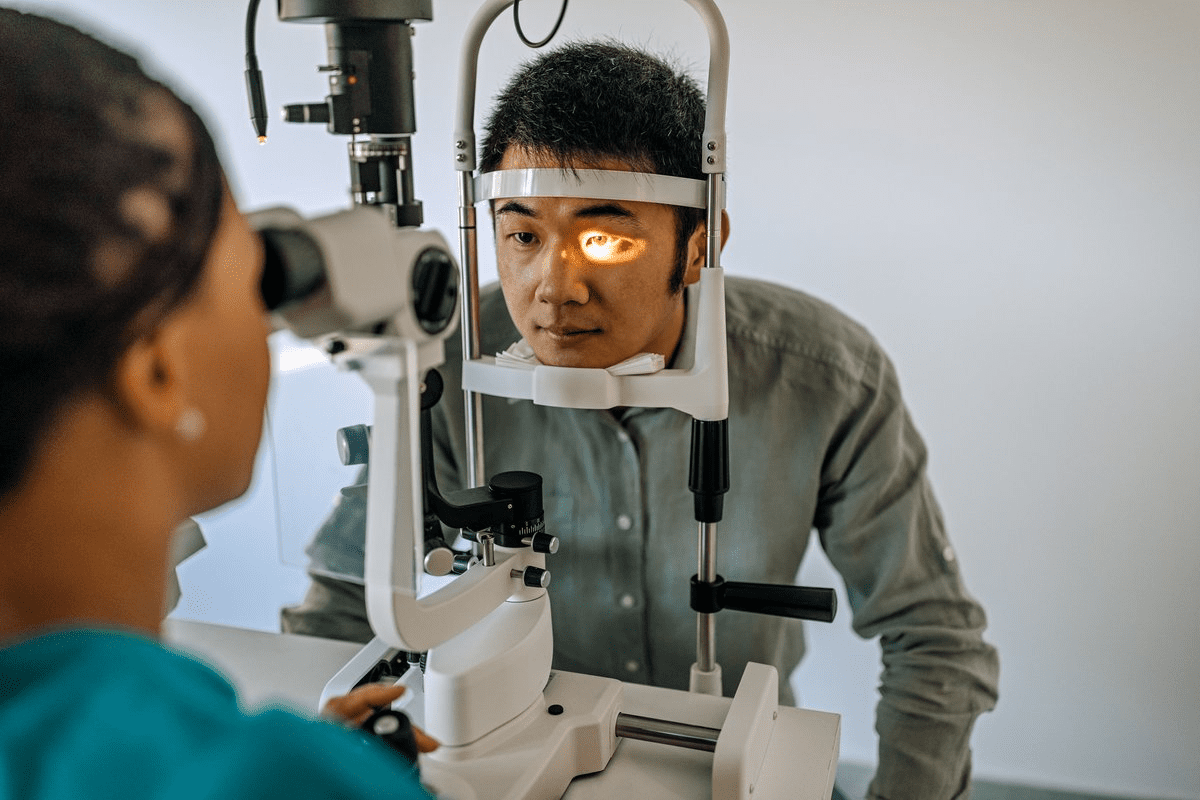
How to Properly Examine the Optic Disc
Examining the optic disc needs a careful method. Ophthalmologists use ophthalmoscopy or fundus photography. They check the disc’s color, shape, and clarity, looking for any issues like hemorrhages.
Knowing the optic disc’s normal anatomy helps doctors spot problems and diagnose vision issues.
Clinical Significance of Blurred Optic Disc Margins
Blurred optic disc margins are a subtle but important sign. They need a detailed check-up. These margins alone don’t mean a specific disease. They can point to many conditions, from simple to serious.
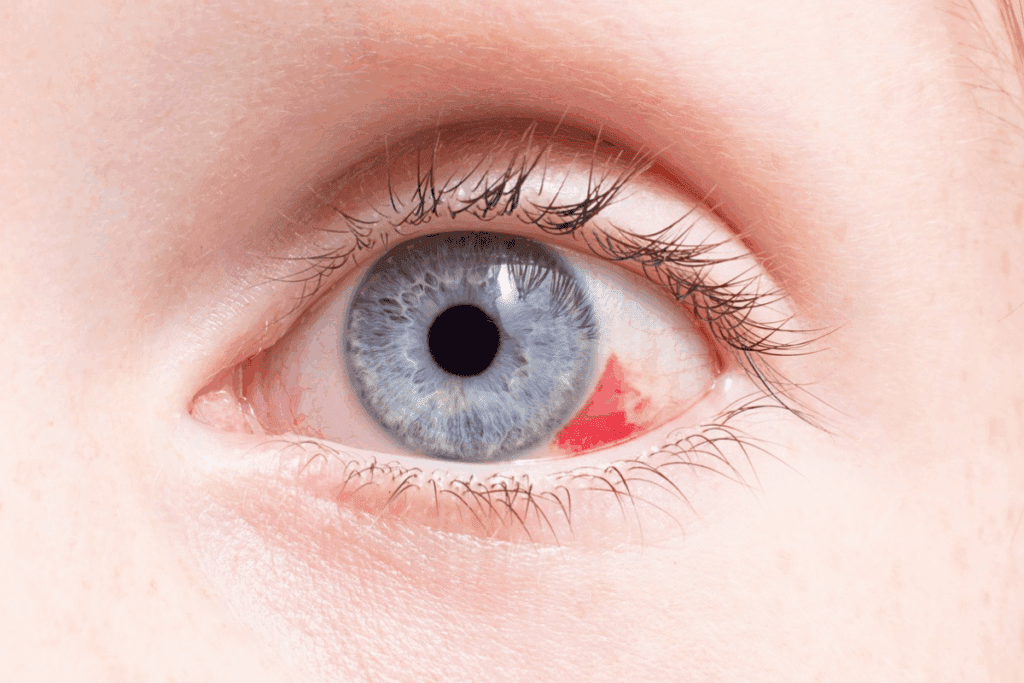
Visual Characteristics of Disc Margin Blurring
Disc margin blurring means the optic disc and retina don’t have a clear edge. This can be mild or severe. It might also show other changes like swelling or bleeding.
For example, papilledema shows up with swollen discs and blurred edges. It often comes with headaches and vision problems. But, drusen on the optic disc can also blur the edges without swelling or symptoms.
Importance of the Nasal Margin
The nasal margin of the optic disc is key when checking for blurring. It’s often the first to show signs of problems like papilledema. So, it’s vital to look closely at this area early on.
Research shows the nasal margin is more likely to blur because of its shape. Doctors should focus on this area during eye exams to catch early signs of blurring.
Associated Symptoms to Monitor
When a patient has blurred optic disc margins, watch for other symptoms. Symptoms like headache, transient visual obscurations, and diplopia suggest serious issues like high pressure in the brain.
- Headache
- Transient visual obscurations
- Diplopia
- Visual field defects
Patients with these symptoms need quick and thorough checks. This includes scans and brain tests to find out why their optic disc margins are blurred.
In summary, blurred optic disc margins are a big deal that needs careful attention. Knowing how to spot these signs, the role of the nasal margin, and what symptoms to watch for helps doctors treat patients better.
Pathophysiology Behind Blurred Optic Disc Margins
The look of the optic disc can change due to intracranial pressure and blood vessel health. Knowing about these factors helps doctors diagnose and treat blurred optic disc margins.
Mechanisms Leading to Disc Margin Blurring
Blurred optic disc margins happen for several reasons. These include:
- Increased intracranial pressure
- Vascular changes and inflammation
- Structural anomalies of the optic disc
The Monro-Kellie hypothesis explains how pressure inside the skull is kept stable. It says that the total volume of blood, cerebrospinal fluid, and brain must stay balanced. If this balance is upset, it can cause high pressure inside the skull. This high pressure can lead to swelling of the optic disc, making it blurry.
Role of Intracranial Pressure
High pressure inside the skull is a big reason for blurred optic disc margins. Problems like space-occupying lesions, venous sinus thrombosis, and idiopathic intracranial hypertension can raise this pressure. This pressure increase makes the optic nerve sheath swell, causing the disc margins to blur.
Vascular and Inflammatory Factors
Conditions affecting blood vessels and inflammation also play a part in blurred optic disc margins. Inflammation of the optic nerve (optic neuritis) or nearby tissues can blur the disc margins. Vascular issues, like diabetic papillopathy or ischemic optic neuropathy, can also change how the optic disc looks.
It’s important to understand how these factors work together. This knowledge helps doctors accurately diagnose and treat patients with blurred optic disc margins.
Papilledema: A Serious Cause of Blurred Optic Disc Margins
Seeing blurred optic disc margins can mean you have papilledema. This is a serious condition that needs quick medical help. It happens when the optic disc swells due to high pressure in the brain. This pressure can come from brain tumors, blocked cerebrospinal fluid, or a condition called idiopathic intracranial hypertension.
Definition and Diagnostic Criteria
Papilledema is when the optic disc swells because of high brain pressure. To diagnose it, doctors look for swelling in both optic discs, normal vision, and no other eye or brain problems. They use eye exams, visual field tests, and scans like MRI or CT to confirm it.
Stages of Papilledema Development
Papilledema goes through stages. It starts with mild swelling and little vision loss. As it gets worse, the swelling grows, and vision problems get more serious. The last stage, atrophic papilledema, makes the optic disc pale and can cause permanent vision loss.
Epidemiology and Risk Factors
Papilledema affects about 13 per 100,000 women aged 20 to 44 who are overweight or obese. Other risks include brain tumors, blood clots in the brain, and a condition called idiopathic intracranial hypertension. Knowing these risks helps catch papilledema early.
It’s important to spot papilledema and its causes to avoid lasting vision damage. We’ll look at more conditions that can cause papilledema next.
Underlying Conditions That Cause Papilledema
Papilledema is caused by many things that raise intracranial pressure. We’ll look at the main reasons for papilledema, which is swelling of the optic disc.
Intracranial Space-Occupying Lesions
Lesions like tumors, cysts, or abscesses can push up intracranial pressure. They take up space in the skull. This can cause swelling of the optic disc, known as papilledema. Tumors, whether they’re benign or cancerous, can press on the optic nerve.
Venous Sinus Thrombosis
Venous sinus thrombosis can also cause papilledema. It happens when a blood clot blocks the venous sinuses. These sinuses drain blood from the brain. The blockage leads to blood buildup and higher pressure inside the skull.
Idiopathic Intracranial Hypertension
Idiopathic intracranial hypertension (IIH) is when pressure inside the skull goes up without a known reason. It often happens in obese women of childbearing age. IIH can cause papilledema and is a big reason for vision problems.
Other Neurological Causes
Other brain issues can also cause papilledema. These include swelling from injuries or infections like meningitis. Problems with cerebrospinal fluid flow can also raise pressure and lead to papilledema.
Knowing the causes of papilledema is key to treating it. Doctors can then focus on the specific problem. This helps to ease symptoms and prevent more issues.
Pseudopapilledema: Benign Causes of Blurred Optic Disc Margins
Pseudopapilledema looks like papilledema but doesn’t have the swelling of the optic nerve head. It’s important to tell the difference to avoid extra tests and worry for patients.
Distinguishing Pseudopapilledema from True Papilledema
It’s important to know the difference between pseudopapilledema and true papilledema. Pseudopapilledema can be caused by optic nerve head drusen, birth defects, or tilted optic discs. Unlike true papilledema, it doesn’t have swelling of the optic nerve head.
Here are the main differences:
- Pseudopapilledema doesn’t have swelling of the nerve layer
- People with pseudopapilledema usually have normal vision
- They don’t have symptoms like headaches or vision problems seen in true papilledema
Optic Nerve Head Drusen
Optic nerve head drusen often cause pseudopapilledema. These are calcified spots in the optic nerve head that look like swelling. Diagnostic imaging like B-scan ultrasonography or OCT can spot drusen.
Drusen have these characteristics:
- They can be seen with the naked eye
- They glow on fluorescein angiography
- They show up as calcification on CT scans
Congenital Disc Anomalies
Congenital disc anomalies can also lead to pseudopapilledema. These include tilted discs, optic disc pits, and other unusual shapes. A detailed check and sometimes imaging are needed to find these.
“Congenital anomalies of the optic disc can mimic papilledema, making it key to tell them apart from serious disc swelling causes.”
Tilted Optic Discs
Tilted optic discs are another reason for pseudopapilledema. This happens when the optic nerve attaches to the globe in an odd way. It makes the disc look like it’s swelling and the edges are fuzzy.
Here are the signs of tilted optic discs:
- The optic nerve attaches at an angle
- The disc looks raised
- It’s often linked with myopic astigmatism
Diagnostic Approach to Evaluating Blurred Disc Margins
Diagnosing blurred optic disc margins requires a mix of clinical checks and advanced imaging. When we see a patient with this issue, we need to carefully examine them. This helps find the real cause.
Clinical Examination Techniques
First, we do a detailed check-up. We start with a patient’s medical history and check their vision. Looking at the optic disc with fundoscopy is key. We also test their visual field to spot any problems.
Key Clinical Examination Techniques:
- Fundoscopy
- Visual acuity testing
- Visual field testing
- Pupillary reflex assessment
Imaging Studies
Imaging is very important in diagnosing blurred optic disc margins. We often use optical coherence tomography (OCT) first. It gives us clear images of the optic nerve and retina. This helps us tell if the problem is real or not.
Imaging Modality | Primary Use | Key Findings |
Optical Coherence Tomography (OCT) | Assess optic nerve head and retinal thickness | Retinal thickening, optic disc elevation |
Magnetic Resonance Imaging (MRI) | Evaluate for intracranial pathology | Mass lesions, venous sinus thrombosis |
Magnetic Resonance Venography (MRV) | Assess venous sinus patency | Venous sinus thrombosis |
Laboratory Tests
We also use lab tests to help diagnose. These tests check for inflammation, infections, or metabolic issues. They help us rule out other problems.
Key Laboratory Tests:
- Complete Blood Count (CBC)
- Erythrocyte Sedimentation Rate (ESR)
- C-reactive Protein (CRP)
- Serum glucose and electrolyte levels
Treatment and Management Strategies
Accurate diagnosis and tailored management are key to treating blurred optic disc margins. Finding the cause of the condition is essential for effective treatment.
Managing Papilledema
Managing papilledema means treating the cause of high intracranial pressure (ICP). We use a multi-faceted approach that includes:
- Medication: Acetazolamide helps by reducing ICP by decreasing cerebrospinal fluid production.
- Lifestyle Modifications: Weight loss is advised for those with idiopathic intracranial hypertension.
- Surgical Interventions: In severe cases, procedures like optic nerve sheath fenestration or CSF shunting may be needed.
Approach to Pseudopapilledema
Pseudopapilledema is usually not serious and doesn’t need aggressive treatment. Our strategy includes:
- Watching for any changes in vision or new symptoms.
- Doing imaging studies to confirm optic nerve head drusen or other issues.
- Informing patients that it’s a benign condition.
When to Refer to a Specialist
Referring to a specialist is important in certain situations. This includes:
- When the diagnosis is unclear.
- If there’s a sign of worsening vision.
- In cases of severe papilledema needing surgery.
Early referral helps ensure patients get the right care, leading to better outcomes.
Follow-up Protocols
Regular check-ups are vital for monitoring and adjusting treatment. We suggest:
- Visual field tests and acuity checks at set times.
- Regular eye exams to watch the disc margin clarity.
- Changing treatment based on how the patient responds and any new symptoms.
By sticking to these protocols, we can manage blurred optic disc margins effectively.
Conclusion: Red Flags and Reassurance for Blurred Optic Disc Findings
It’s important to understand why blurred optic disc margins happen. We’ve looked at different reasons, like papilledema and pseudopapilledema. Knowing the difference between them is key.
Quick action to treat the cause can stop problems and help patients get better. It’s vital to watch for signs of serious issues, like bad headaches or vision problems.
Healthcare teams can reassure patients with simple conditions. But, they must act fast if a serious issue is found. Our aim is to offer top-notch care to all patients, no matter where they’re from. We want to guide them with kindness and accuracy.
FAQ
What are blurred optic disc margins?
Blurred optic disc margins mean the edges of the optic disc look fuzzy. This can be a sign of several health issues, like papilledema or pseudopapilledema.
What is the significance of the nasal margin in optic disc examination?
The nasal margin is key in checking the optic disc. It can show signs of papilledema early. This is because its blurring can signal optic nerve elevation.
How is pseudopapilledema distinguished from true papilledema?
Doctors use clinical exams, imaging, and lab tests to tell pseudopapilledema from true papilledema. This helps find the real cause of the fuzzy optic disc edges.
What are optic nerve head drusen, and how do they relate to pseudopapilledema?
Optic nerve head drusen are harmless calcium deposits in the optic nerve head. They can cause pseudopapilledema, which looks like true papilledema but isn’t linked to high brain pressure.
Is pseudopapilledema dangerous?
Pseudopapilledema is usually not dangerous. But, it might mean there’s an underlying issue that needs attention and care.
What is the role of intracranial pressure in blurred optic disc margins?
High brain pressure is a big factor in blurred optic disc margins, like in papilledema. It can push the optic nerve up and blur the disc edges.
How is papilledema diagnosed?
Doctors use eye exams, imaging like MRI or CT scans, and lab tests to spot papilledema. These steps help figure out what’s causing the problem.
What are the stages of papilledema development?
Papilledema goes through stages, from early to chronic. Each stage has its own signs and what it means for treatment.
What is the importance of follow-up protocols in managing blurred optic disc margins?
Keeping up with follow-up plans is key for managing blurred optic disc margins. It lets doctors track the condition, tweak treatments, and avoid serious issues.
When should patients with blurred optic disc margins be referred to a specialist?
If the cause of blurred optic disc margins is unclear or the condition is serious, see a specialist. A neuro-ophthalmologist can offer the needed care and expertise.
What is the optic nerve head (ONH) and how does it relate to blurred disc margins?
The optic nerve head (ONH) is what you see of the optic nerve when you look into someone’s eye. Its look can change in conditions like papilledema or pseudopapilledema, causing blurred disc margins.
What is the difference between optic disc margin blurring and optic disc blurring?
Optic disc margin blurring means the edges of the optic disc are fuzzy. Optic disc blurring is a broader term that includes swelling or color changes in the disc, not just the edges.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538291/
National Center for Biotechnology Information. Blurred Optic Disc Margins: Causes and When to Worry. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2920662/