Last Updated on November 27, 2025 by Bilal Hasdemir

Getting a prostate cancer diagnosis can be scary, and a Gleason score of 7 makes it even more daunting. At Liv Hospital, we know how important clear and caring support is during tough times. A Gleason score of 7 means you’re at a higher risk of cancer growing, which helps us decide how to treat you.
When you find out you have prostate cancer with a Gleason score of 7, it’s a big moment. Our team is here to help you understand your options and make choices that are right for you. We’ll look at all the possible treatments and work with you to pick the best one.
Key Takeaways
- A Gleason score of 7 indicates intermediate-risk prostate cancer.
- Treatment decisions are guided by this score and individual patient factors.
- Liv Hospital offers patient-focused, evidence-based care for prostate cancer.
- Various treatment modalities are available, including radiation therapy.
- Our team works closely with patients to determine the best treatment plan.
Understanding the Gleason Scoring System

The Gleason grading system was created in the 1960s. It helps doctors understand how serious prostate cancer is. They look at how the cancer cells are arranged and how different they are from normal cells.
The History and Development of Gleason Grading
Doctor introduced the Gleason grading system in the 1960s. It was made to give a standard way to rate prostate cancer. Over time, it has been updated to better match what doctors see in real life.
At first, the score was from 2 to 10. Lower scores meant the cancer was less aggressive. Now, scores range from 6 to 10, showing a better understanding of cancer’s aggressiveness.
How Pathologists Identify and Grade Cancer Patterns
Pathologists look at biopsy samples under a microscope. They find the main patterns of cancer cell growth. The Gleason system rates these patterns from 1 to 5, with 1 being the least aggressive and 5 the most.
They look at how the tumor cells form glands and how they look compared to normal prostate cells. They pick the two most common patterns and add their grades to get the Gleason score.
The Significance of Primary and Secondary Patterns in Diagnosis
The primary and secondary patterns are key in finding the Gleason score. The primary pattern is the most common, and the secondary is the second. The score is the sum of these two grades.
For example, if the primary pattern is Grade 3 and the secondary is Grade 4, the score is 3+4=7. Knowing if it’s 3+4 or 4+3 matters a lot because it affects the prognosis.
| Gleason Score | Description | Prognosis |
|---|---|---|
| 6 or less | Low-grade cancer | Favorable |
| 7 | Intermediate-grade cancer | Variable |
| 8-10 | High-grade cancer | Poor |
Knowing about the Gleason scoring system is important for both patients and doctors. It helps decide on treatments and gives clues about how the cancer might behave.
What Does a Gleason Score of 7 Mean for Prostate Cancer?

A Gleason 7 prostate cancer diagnosis is complex for both patients and doctors. It’s tough to get this news, and it’s key to understand what it means. A Gleason score of 7 shows the cancer is somewhat aggressive, but it’s not all the same.
Interpreting Gleason Score 7 in the Context of Cancer Aggressiveness
A Gleason score of 7 means the cancer cells are graded as 3+4 or 4+3. The primary and secondary grades are key to knowing how aggressive the cancer is. We’ll look at how these grades affect the cancer’s outlook.
The difference between Gleason 3+4=7 and Gleason 4+3=7 is big. It shows how the cancer acts and how it might affect the patient.
Gleason 3+4=7 vs. Gleason 4+3=7: Critical Differences in Prognosis
Gleason 3+4=7 means the cancer is mostly grade 3 with some grade 4. Gleason 4+3=7 shows a more aggressive cancer, mostly grade 4. This difference is important because Gleason 4+3=7 cancers are more likely to spread and grow.
Risk Classification and Stratification for Gleason 7 Patients
For patients with Gleason 7 prostate cancer, knowing the risk is key. We look at PSA levels, clinical staging, and biopsy results to sort patients. This helps us choose the best treatment for each patient.
Knowing the risk helps doctors give treatments that fit each patient. This way, we balance the benefits of treatment with possible side effects.
Diagnostic Process and Additional Testing for Gleason Score 7
Patients with a Gleason score of 7 prostate cancer go through several steps and tests. Accurate diagnosis is key to finding the best treatment.
Prostate Biopsy Procedures and Pathology Interpretation
A prostate biopsy is the main way to diagnose prostate cancer and get the Gleason score. Urologists take tissue samples from the prostate. Then, pathologists examine these samples under a microscope.
The biopsy results show if there’s cancer and how aggressive it is. A Gleason score of 7 means the cancer is intermediate-risk. More tests are needed to understand its behavior.
Complementary Tests for Accurate Staging
After a Gleason score of 7, more tests are done to stage the cancer. These tests check if the cancer has spread. They help decide the best treatment.
- PSA Testing: Prostate-Specific Antigen (PSA) levels are checked to see if the cancer might spread or come back.
- Digital Rectal Examination (DRE): A DRE is done to look for any prostate gland abnormalities.
- Bone Scans: Bone scans are done to find any bone metastases, if the PSA level is high.
Advanced Imaging: MRI, PET Scans, and Bone Scans
Advanced imaging is key in staging Gleason score 7 prostate cancer. These technologies give detailed images of the prostate and nearby areas. They help find any cancer spread.
Some important imaging methods include:
- MRI (Magnetic Resonance Imaging): Gives detailed images of the prostate. It helps find any cancer spread outside the prostate or to the seminal vesicles.
- PET Scans (Positron Emission Tomography): Good for finding metastatic disease. They work best with specific tracers like PSMA.
- Bone Scans: Important for checking bone health and finding any metastatic lesions.
Healthcare providers use all this information to create a treatment plan that fits the patient’s needs.
Surgical Approaches for Treating Gleason 7 Prostate Cancer
Surgery is a key treatment for Gleason 7 prostate cancer, giving patients hope for a cure. It’s important for those with this condition to know about the surgical options. This knowledge helps them make informed decisions about their care.
Radical Prostatectomy: Open, Laparoscopic, and Robotic Techniques
Radical prostatectomy, or removing the prostate gland, is a common treatment for Gleason 7 prostate cancer. There are different ways to do this surgery:
- Open Radical Prostatectomy: This traditional method uses one big incision in the abdomen or perineum to remove the prostate.
- Laparoscopic Radical Prostatectomy: A minimally invasive method that uses small incisions and a laparoscope to remove the prostate.
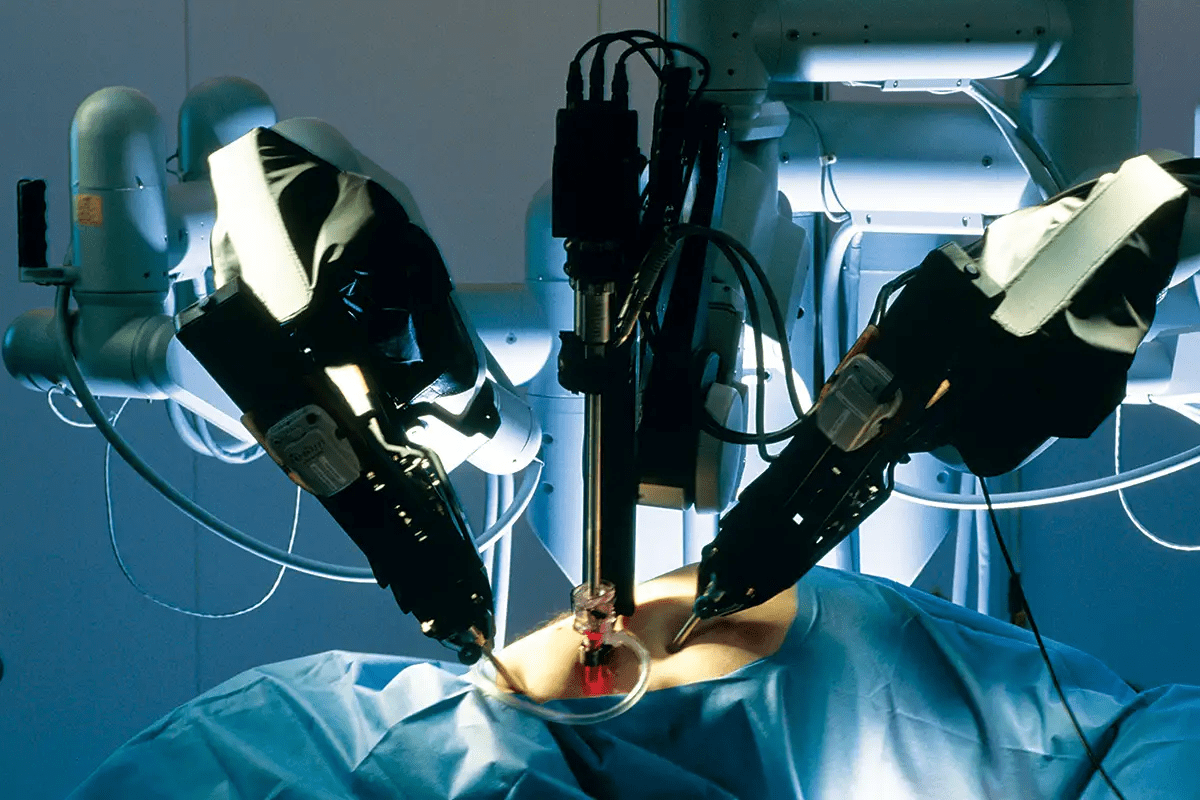
- Robotic-Assisted Laparoscopic Prostatectomy: An advanced laparoscopic surgery that uses a robotic system for better precision and visibility.
Each method has its own benefits and drawbacks. The choice depends on the patient’s health and the surgeon’s skill.
Nerve-Sparing Procedures and Functional Outcomes
Nerve-sparing radical prostatectomy tries to save the nerves around the prostate. These nerves are important for sexual function and urinary continence. Saving these nerves can improve sexual function after surgery and reduce urinary incontinence risk.
The success of nerve-sparing procedures depends on several factors. These include the patient’s age, the extent of nerve damage, and the surgeon’s experience. We talk to our patients about the benefits and risks to set realistic expectations for their recovery.
Pelvic Lymph Node Dissection Considerations
Pelvic lymph node dissection (PLND) is often done during radical prostatectomy. It checks if the cancer has spread to the lymph nodes. This information helps accurately stage the cancer and decide on further treatments.
The extent of PLND can vary. Some surgeons do a more extensive dissection for better cancer staging. Others may choose a limited approach to lower the risk of complications.
Recovery Timeline and Post-Surgical Monitoring
The recovery time after radical prostatectomy varies, but most patients can get back to normal in a few weeks. After surgery, regular check-ups are important. They help monitor for cancer recurrence and manage any side effects.
We stress the importance of post-operative care. We give our patients detailed instructions on how to monitor their recovery. We also tell them when to seek medical attention if they have any concerning symptoms.
Radiation Therapy Options for Gleason Score 7
Patients with Gleason score 7 prostate cancer have several radiation therapy options. Each treatment is tailored to fit the patient’s needs. This ensures the best care for each individual.
External Beam Radiation Therapy (EBRT) Protocols
External Beam Radiation Therapy (EBRT) is a common treatment for prostate cancer. It uses beams from outside the body to kill cancer cells. For Gleason score 7, EBRT can target cancer precisely, protecting healthy tissues.
Some key aspects of EBRT protocols include:
- Intensity-Modulated Radiation Therapy (IMRT): Allows for precise shaping of the radiation beam to fit the tumor.
- Image-Guided Radiation Therapy (IGRT): Utilizes imaging technologies to ensure accurate targeting of the tumor during treatment.
Brachytherapy: High-Dose Rate vs. Low-Dose Rate
Brachytherapy places radioactive material inside or near the tumor. It’s effective for Gleason score 7 prostate cancer. There are two types:
- High-Dose Rate (HDR) Brachytherapy: Delivers high doses of radiation over a short period, typically requiring multiple sessions.
- Low-Dose Rate (LDR) Brachytherapy: Involves permanent implantation of radioactive seeds that emit lower doses of radiation over an extended period.
Both HDR and LDR brachytherapy have their advantages. They are chosen based on the patient’s specific condition and preferences.
Hypofractionated Radiation and Stereotactic Body Radiation Therapy
Hypofractionated radiation therapy delivers larger doses of radiation over fewer sessions. Stereotactic Body Radiation Therapy (SBRT) is a type of hypofractionated radiation. It precisely targets the tumor with high doses of radiation.
These advanced techniques offer effective treatment with fewer side effects and shorter treatment durations.
Adjuvant vs. Salvage Radiation After Surgery
After surgery, some patients may need additional radiation therapy. There are two main scenarios:
- Adjuvant Radiation Therapy: Administered after surgery to eliminate any remaining cancer cells and reduce the risk of recurrence.
- Salvage Radiation Therapy: Used when cancer recurs after surgery, aiming to control the disease.
Understanding the differences between adjuvant and salvage radiation therapy is key for making informed treatment decisions.
Hormone Therapy and Systemic Treatments for Gleason 7 Prostate Cancer
Hormone therapy is key in treating Gleason 7 prostate cancer. It’s often used with other treatments. This is important for patients with high-risk cancer.
Androgen Deprivation Therapy: Indications and Approaches
Androgen deprivation therapy (ADT) is a main part of hormone therapy for prostate cancer. ADT lowers male hormones like testosterone. This slows down cancer growth.
ADT is used for patients with high-risk or advanced cancer. There are different ways to do ADT:
- Orchiectomy: Surgery to remove the testicles to lower testosterone.
- Gonadotropin-releasing hormone (GnRH) agonists: Medications that first increase, then lower testosterone.
- GnRH antagonists: Drugs that block testosterone production directly.
- Anti-androgens: Medications that stop androgens from working at the cell level.
Neoadjuvant and Adjuvant Hormone Therapy with Radiation
Neoadjuvant hormone therapy is given before radiation to shrink tumors. Adjuvant hormone therapy is after radiation to kill any left-over cancer cells. This helps prevent cancer from coming back.
Combining hormone therapy with radiation helps patients with Gleason 7 prostate cancer. It’s most beneficial for those with higher-risk disease.
Managing Side Effects of Hormone Therapy
Hormone therapy can cause side effects like hot flashes and fatigue. It’s important to manage these to keep patients’ quality of life good.
Ways to manage side effects include diet, exercise, and medications. These help reduce symptoms.
Emerging Systemic Treatment Options
New treatments for prostate cancer are being researched. These include new hormone therapies and immunotherapies. They aim to help patients with advanced or high-risk cancer.
Clinical trials are key to testing these new treatments. Patients with Gleason 7 prostate cancer might be eligible. This gives them access to new therapies.
Active Surveillance for Select Gleason 7 Patients
Gleason 7 prostate cancer patients might find active surveillance helpful. This method watches the disease without starting treatment right away. It’s good for those with low-risk disease, as it avoids treatment side effects.
Patient Selection Criteria for Surveillance of Gleason 3+4=7
Choosing the right patients for active surveillance is key. For Gleason 3+4=7 prostate cancer, patient selection criteria include:
- Low PSA density
- Favorable PSA kinetics
- Limited cancer burden on biopsy
- No adverse features on imaging studies like MRI
These criteria help find patients with less aggressive disease. They can safely watch their cancer instead of getting treatment right away.
Monitoring Protocols: PSA, MRI, and Repeat Biopsies
Good monitoring is essential for active surveillance. The plan usually includes:
- Regular PSA tests to watch PSA levels
- Periodic MRI scans to check tumor size and type
- Repeat biopsies at set times to check for cancer growth
These tools help spot any disease growth. This allows for quick action if needed.
Triggers for Intervention During Surveillance
Certain triggers for intervention during active surveillance include:
- Significant increase in PSA velocity
- Upgrade in Gleason score on repeat biopsy
- Increase in tumor size or aggressiveness on imaging
If these triggers happen, patients are reviewed for treatments like surgery or radiation.
Quality of Life During Active Surveillance
Active surveillance can greatly affect a patient’s quality of life. It lets patients keep their health and avoid treatment side effects. But, the mental impact of having untreated cancer is important. Support systems should help with anxiety and other worries.
Managing Treatment Side Effects and Quality of Life Considerations
Managing side effects is key for patients with Gleason 7 prostate cancer. Treatment can affect daily life and well-being. It’s important to keep quality of life high.
Sexual Function After Prostate Cancer Treatment
Prostate cancer treatment can harm sexual function. Surgery and radiation can damage nerves and blood vessels. This can lead to erectile dysfunction (ED).
Nerve-sparing techniques and penile rehabilitation programs can help. Medications like sildenafil can also manage ED well.
Urinary Continence: Prevention and Management of Issues
Urinary incontinence is a side effect of prostate cancer treatment, mainly after surgery. It can range from mild to severe.
Pelvic floor exercises (Kegel exercises) can help. Sometimes, medication or surgery is needed for persistent incontinence.
Bowel Function Following Radiation Therapy
Radiation therapy can change bowel habits. Symptoms include diarrhea, urgency, and rectal bleeding. These can be hard to deal with.
Changing your diet can help. Avoiding spicy or fatty foods is a good start. Medications can also help with specific issues.
Psychological Support and Coping Strategies
The mental impact of prostate cancer is big. Anxiety, depression, and fear of recurrence are common.
Counseling and support groups offer a safe space. They help patients share and learn from others. Mindfulness and relaxation techniques can also help manage stress.
By focusing on these areas, we can improve life for Gleason 7 prostate cancer patients. It helps them deal with treatment challenges and more.
Conclusion: Navigating Treatment Decisions for Gleason Score 7 Prostate Cancer
Choosing a treatment for Gleason score 7 prostate cancer can be tough. We’ve looked at the Gleason scoring system, how doctors diagnose it, and treatment choices like surgery, radiation, and hormone therapy.
When deciding on treatment, the patient’s health and wishes are key. A Gleason score of 7 means the cancer is moderately aggressive. But, the outlook can differ based on whether it’s 3+4=7 or 4+3=7.
It’s vital to tailor treatment to each patient. Some might choose active surveillance, while others need more intense treatment. Knowing what does a Gleason score of 7 mean helps make better choices.
In the end, level 7 prostate cancer treatment plans should be made with a doctor. They consider new research and the patient’s specific needs. This way, we can create a treatment plan that fits the patient’s unique situation.
FAQ
What does a Gleason score of 7 mean for prostate cancer?
A Gleason score of 7 shows the cancer is moderately different from normal cells. This score is found by adding the grades of the two most common cell patterns in the tumor.
What is the difference between Gleason 3+4=7 and Gleason 4+3=7?
Gleason 3+4=7 has grade 3 as the main pattern and grade 4 as the secondary. Gleason 4+3=7 has grade 4 as the main pattern and grade 3 as the secondary. Gleason 4+3=7 is seen as more aggressive because it has more grade 4 cells.
What are the treatment options for Gleason score 7 prostate cancer?
For Gleason score 7 prostate cancer, treatments include surgery, radiation therapy, hormone therapy, active surveillance, or a mix of these. The choice depends on the patient’s health, cancer stage, and personal preferences.
Is Gleason score 7 prostate cancer curable?
Yes, Gleason score 7 prostate cancer can be cured if caught early and treated right. The treatment choice depends on the patient’s age, health, and cancer details.
What is active surveillance for Gleason 7 prostate cancer?
Active surveillance for Gleason 7 prostate cancer means watching the cancer closely. This includes regular PSA tests, digital rectal exams, and biopsies. It’s often for patients with low-risk or favorable intermediate-risk cancer.
How does the Gleason score affect treatment decisions?
The Gleason score is key in deciding how aggressive the cancer is. A higher score means more aggressive cancer, which might need more intense treatment.
What are the side effects of treatments for Gleason 7 prostate cancer?
Treatments for Gleason 7 prostate cancer can cause side effects. These include urinary incontinence, erectile dysfunction, bowel problems, and hormonal changes. Managing these side effects is important in prostate cancer care.
Can Gleason score 7 prostate cancer be treated with radiation alone?
Yes, radiation therapy alone or with hormone therapy is a treatment option for Gleason score 7 prostate cancer. The choice of radiation therapy depends on the cancer’s stage and the patient’s health.
What is the role of hormone therapy in treating Gleason 7 prostate cancer?
Hormone therapy, or androgen deprivation therapy, lowers testosterone levels. This can slow cancer growth. It’s often used with radiation therapy or alone for advanced cases.
How is Gleason score 7 prostate cancer diagnosed?
Diagnosis involves a prostate biopsy to take tissue samples. These are then examined to find the Gleason score. MRI and PET scans may also be used to stage the cancer and plan treatment.
References
- Sakr WA, Tefilli MV, Grignon DJ, et al. Gleason score 7 prostate cancer: a heterogeneous entity? Correlation with pathologic parameters and disease‑free survival. Urology. 2000 Nov;56(5):730–4. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11068289/ (PubMed)
- Virginia Cancer Specialists Blog. Understanding the prostate biopsy Gleason score. Retrieved from https://blog.virginiacancer.com/understanding-the-prostate-biopsy-gleason-score
- American Association for Cancer Research (AACR). What is a Gleason score for prostate cancer? (May 22, 2025). Retrieved from https://www.aacr.org/blog/2025/05/22/what-is-a-gleason-score-for-prostate-cancer/