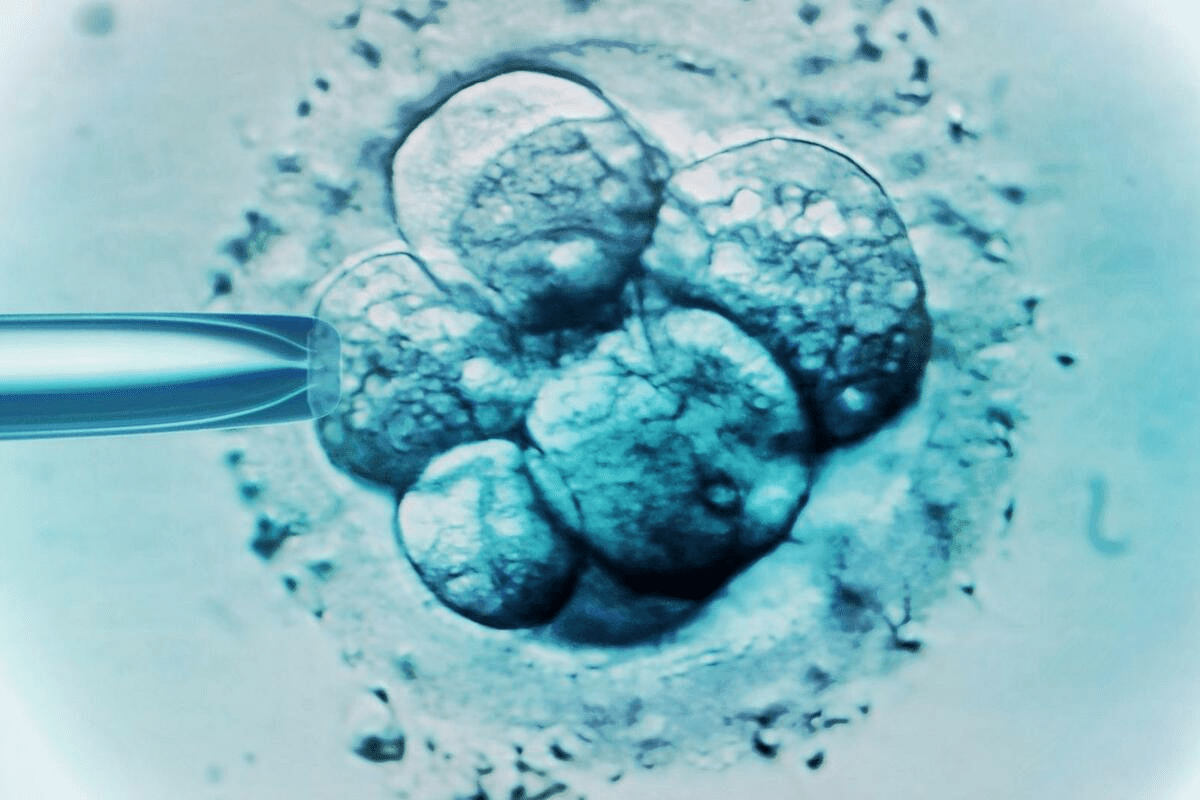
For couples going through IVF, knowing what a blastocyst looks like is key. This is because how an embryo looks can affect its chances of success.
We dive into the details of blastocysts, a vital part of IVF. A blastocyst has an inner cell mass, trophectoderm, and a fluid-filled space. These are seen on days 5 and 6 of the IVF process.
By learning about a blastocyst’s looks, we can judge its quality. This helps us see if it might implant well.
Key Takeaways
- Understanding blastocyst morphology is key for IVF success.
- A blastocyst has an inner cell mass, trophectoderm, and a fluid-filled cavity.
- The Gardner grading system helps judge blastocyst quality.
- Blastocyst development is a critical stage in IVF embryo growth.
- Checking blastocyst quality helps pick the best embryo for transfer.
The Journey to Blastocyst Stage
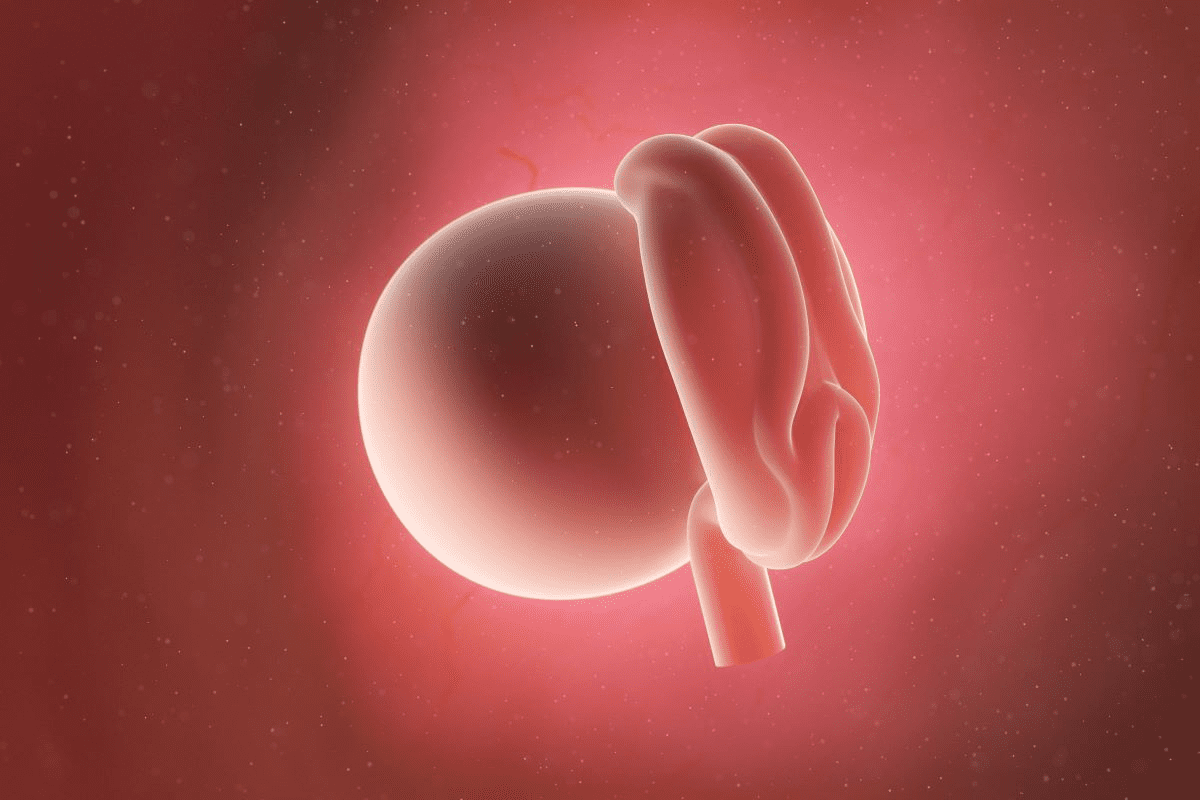
From fertilization to day 5, the embryo goes through big changes. It forms a blastocyst, which is key for IVF success. This time is filled with fast cell division and growth, leading to a complex structure ready to become a fetus.
From Fertilization to Day 5
The trip to the blastocyst stage starts with fertilization. A sperm meets an egg, creating a zygote. This cell then divides many times, moving through different stages:
- Zygote: The first cell after fertilization.
- Cleavage stages: The zygote splits into many cells without growing much.
- Morula: A tight group of cells from more division.
- Blastocyst: A structure with a fluid-filled space and different cell types.
Cell Division and Development Timeline
The change from zygote to blastocyst is carefully controlled. Knowing the timeline helps us understand the stages:
Day | Stage | Description |
1 | Zygote | Fertilized egg |
2-3 | Cleavage | Many cell divisions |
4 | Morula | A tight group of cells |
5 | Blastocyst | A structure with a fluid-filled space and different cell types |
What Does a Blastocyst Look Like?
The look of a blastocyst tells us a lot about its quality and chance of implanting well. We need to know its basic parts and structure to understand it.
Basic Structure and Components
A blastocyst has a big cavity called the blastocoel, filled with fluid. Inside, the inner cell mass (ICM) will grow into the fetus. The trophectoderm (TE) will make the placenta. “The blastocyst stage is a critical milestone in embryo development,” say experts, “and its structure shows if it’s viable.”
Size and Appearance
Blastocysts come in different sizes and looks. A top-quality 5-day embryo blastocyst has a clear inner cell mass and a tight trophectoderm layer. The size of the blastocoel tells us how developed it is.
Experts say, “A fully expanded blastocyst with a big blastocoel and a tight inner cell mass usually has a better chance of implanting.”
When looking at 5 day thawed blastocyst pictures, experts check for these signs. Knowing these visual clues helps them judge the success of IVF treatments.
The Three Key Components of a Blastocyst
A blastocyst has three main parts that are vital for its growth and success. Knowing about these parts helps us see how good a blastocyst is and if it can implant well.
Inner Cell Mass (ICM): Future Baby
The Inner Cell Mass (ICM) is a group of cells in the blastocyst that will become the baby. It’s key for the embryo’s growth, as it forms all the baby’s tissues and organs. A healthy ICM has lots of tightly packed cells, showing strong baby development.
The quality of the ICM is very important for the embryo’s success. Experts check the ICM during grading to see if it can implant and grow well.
Trophectoderm (TE): Future Placenta
The Trophectoderm (TE) is the outer layer of cells around the blastocyst. It will become the placenta and other tissues needed for the baby’s growth. The TE is vital for implantation, as it helps the embryo attach to the uterine lining.
A good TE is essential for a healthy placenta. This is important for giving the baby the nutrients and oxygen it needs. The TE’s quality is also checked during grading, showing the embryo’s implantation chances.
Blastocoel Cavity: Fluid-Filled Center
The Blastocoel cavity is the fluid-filled area inside the blastocyst. It’s important for the blastocyst’s growth and expansion. A big, fully expanded blastocoel cavity means the embryo might implant well.
The size and presence of the blastocoel cavity are looked at during grading. This helps judge the blastocyst’s overall quality.
In summary, the Inner Cell Mass, Trophectoderm, and Blastocoel cavity are key for a blastocyst’s growth and implantation chances. Knowing about these parts is vital for understanding a blastocyst’s quality and viability.
Blastocyst Expansion: Stages 1-6 Explained
Blastocyst expansion stages give us insights into an embryo’s development and health. Understanding these stages is key to knowing if an embryo might implant successfully.
Early Blastocyst (Stage 1-2)
The early stages of the blastocyst start around day 5. At this time, the embryo forms a fluid-filled area called the blastocoel. Stage 1 sees a small blastocoel, less than half the embryo’s size. By Stage 2, the blastocoel grows to at least half the embryo’s size.
Expanded Blastocyst (Stage 3-4)
The blastocyst keeps growing, reaching Stage 3 with a fully expanded cavity. Here, the embryo starts to show signs of different parts. By Stage 4, the blastocyst is fully grown, and the inner cell mass and trophectoderm are clear.
Hatching Blastocyst (Stage 5-6)
The last stages involve the embryo breaking free from its outer shell, the zona pellucida. At Stage 5, the blastocyst begins to push through the zona pellucida. By Stage 6, it has fully hatched and is ready to implant.
Understanding the stages of blastocyst expansion is vital. It helps couples and doctors make better choices about IVF.
- Stage 1-2: Early blastocyst formation with initial blastocoel expansion.
- Stage 3-4: Continued expansion with differentiation of ICM and TE.
- Stage 5-6: Hatching of the blastocyst from the zona pellucida.
The Gardner Blastocyst Grading System
For couples going through IVF, knowing the Gardner blastocyst grading system is very helpful. This system helps check the quality of blastocysts. It gives important info on their chance to implant well.
The Three-Part Grading Method
The Gardner system looks at three main things: expansion grade, inner cell mass (ICM) quality, and trophectoderm (TE) quality. These parts give doctors and scientists key info on the blastocyst’s growth chance.
Expansion Grade: This is how much the blastocyst has grown. It’s scored from 1 to 6, with:
- 1: The blastocyst hasn’t fully grown.
- 2-3: It’s growing but not fully.
- 4-6: It’s fully grown or starting to hatch.
Inner Cell Mass (ICM) Quality: The ICM is scored by the number and how cells are arranged. These cells will become the fetus. The scores are:
- A: Many cells are tightly packed.
- B: Some cells are loosely grouped.
- C: There are few cells.
Trophectoderm (TE) Quality: The TE is checked by the number and arrangement of cells that will make the placenta. The scores are similar to the ICM:
- A: Many cells form a tight layer.
- B: Some cells form a loose layer.
- C: There are very few large cells.
How to Read Blastocyst Grades
It’s key to know how to read blastocyst grades. A grade is shown as a mix of numbers and letters, like “5AA” or “4BC.”
For example, “5AA” means:
- 5: The blastocyst is hatching.
- A: The ICM is of high quality.
- A: The TE is of high quality.
Here’s a table to help understand the grades better:
Grade Component | Description | Grade |
Expansion | Degree of expansion | 1-6 |
ICM Quality | Number and arrangement of cells | A, B, C |
TE Quality | Number and arrangement of cells | A, B, C |
By learning the Gardner blastocyst grading system, couples can understand their embryo’s chances better. This helps them make smart choices in their IVF journey.
Inner Cell Mass (ICM) Grading: A to C
The inner cell mass (ICM) grading tells us a lot about a blastocyst’s quality and health. The ICM is key because it grows into the fetus. So, checking its grade is vital for judging the blastocyst’s overall quality.
Grade A: Many Tightly Packed Cells
A Grade A ICM has lots of cells packed tightly together. This shows a top-notch ICM with a big number of healthy cells. Such a dense cell arrangement is a good sign for the embryo’s chances of implanting and growing well.
Grade B: Several Loosely Grouped Cells
A Grade B ICM has cells that are loosely grouped. This grade means the ICM is of moderate quality. Even though there are fewer cells than in Grade A, there are enough to show promise. The cells’ loose grouping might hint at less-than-ideal conditions, but it’s okay for transferring the embryo.
Grade C: Few Cells
A Grade C ICM has very few cells. This grade points to a lower quality ICM, which might mean the embryo has less chance of implanting and growing. Having few cells in the ICM can hinder the embryo’s development.
Knowing how to grade the ICM is key for doctors and scientists to judge a blastocyst’s quality. By looking at the ICM grade, we can guess the embryo’s chances of success. This helps us choose the best embryos for transfer and improve pregnancy rates.
Trophectoderm (TE) Grading: A to C
Understanding the trophectoderm grading is key to knowing an embryo’s quality. The trophectoderm forms the placenta and other tissues. It’s a vital part of the embryo.
Grade A: Many Cells Forming Cohesive Epithelium
A Grade A trophectoderm shows many cells forming a tight epithelium. This means a high-quality trophectoderm with lots of cells. It shows strong implantation and development chances.
Grade B: Few Cells Forming Loose Epithelium
A Grade B trophectoderm has fewer cells forming a loose epithelium. It’s not as good as Grade A but shows a viable trophectoderm. It has a slightly lower quality.
Grade C: Very Few Large Cells
A Grade C trophectoderm has very few large cells, showing a lower quality. It suggests less chance for successful implantation and development.
Grading the trophectoderm, along with the inner cell mass, gives a full view of the blastocyst’s quality. Knowing these grades helps us understand an IVF cycle’s success chances.
Visual Examples of Different Blastocyst Grades
Looking at pictures of blastocysts can help couples understand their quality. This is important for IVF treatment. Knowing the visual differences in blastocyst grades helps make better decisions.
High-Quality Blastocysts (5AA, 6AA)
High-quality blastocysts, like those graded 5AA or 6AA, have a better chance of implanting. They have a well-developed inner cell mass (ICM) and trophectoderm (TE). This means they have a strong chance of growing well.
The ICM is graded A for its many tightly packed cells. The TE is also graded A for its cohesive cells. This is a sign of a strong embryo.
Key characteristics of high-quality blastocysts:
- Well-developed ICM with many tightly packed cells
- Well-developed TE with many cells forming a cohesive epithelium
- Expanded blastocoel cavity
Good-Quality Blastocysts (4BB, 5BB)
Good-quality blastocysts, like those graded 4BB or 5BB, also have a good chance of implanting. They might not be as developed as high-quality ones. But they show promising signs.
Notable features of good-quality blastocysts:
- Good TE grade with several cells forming a loose epithelium
- ICM with several loosely grouped cells
- Blastocoel cavity that is fully formed
Fair-Quality Blastocysts (3BC, 4BC)
Fair-quality blastocysts, like those graded 3BC or 4BC, have a lower chance of implanting. These embryos might have a less developed ICM or TE. Or their blastocoel cavity might be small. Knowing this can help couples decide on their IVF treatment.
Characteristics of fair-quality blastocysts:
- Less developed ICM with few cells
- TE with few cells forming a loose epithelium
- Smaller or partially formed blastocoel cavity
Day 5 vs. Day 6 Blastocysts: Visual Differences
Day 5 and day 6 blastocysts show different growth stages. This affects their chances of success in IVF. Knowing these differences helps couples make better choices for their treatment.
Development Timeline Comparison
The growth of a blastocyst is complex. By day 5, many embryos have a fluid-filled cavity and two cell groups. But, some take an extra day, reaching this stage by day 6.
Embryos grow at different rates. Both day 5 and day 6 blastocysts can be good for transfer. Research says day 5 blastocysts might be of higher quality.
Success Rates and Implications
Day 5 blastocysts often have better implantation rates. This is because they are more developed and better match the uterus.
But, day 6 blastocysts can also lead to successful pregnancies. Choosing between day 5 or day 6 depends on many factors. These include embryo quality, patient age, and medical history.
In summary, day 5 blastocysts might have a slight edge in success rates. But, day 6 blastocysts should not be ignored. Improvements in IVF have boosted success rates for both stages.
Understanding the visual and growth differences between day 5 and day 6 blastocysts is key. It helps couples and doctors make better decisions for IVF. This can increase the chances of a successful outcome.
How Embryo Appearance Relates to IVF Success
It’s important for couples going through fertility treatment to know how embryo appearance affects IVF success. Grading embryos is a detailed process. It helps doctors figure out if an embryo can implant well.
Correlation Between Grades and Implantation
Studies show a clear link between embryo grades and IVF success. High-quality embryos, like those graded 5AA or 6AA, have better implantation and pregnancy rates. The grading looks at the inner cell mass, trophectoderm, and how much the embryo has grown.
Embryo grading is more than just looks. It’s a key tool for predicting implantation success. Research has shown that embryos with higher grades do better in IVF cycles.
Embryo Grade | Implantation Rate | Pregnancy Rate |
5AA/6AA | 60-70% | 50-60% |
4BB/5BB | 40-50% | 30-40% |
3BC/4BC | 20-30% | 15-25% |
Limitations of Visual Assessment
Embryo grading is useful but has its limits. It’s based on what the eye sees, which can vary. The quality of the microscope and the embryologist’s experience also play a role.
Also, grading mainly looks at how the embryo looks, not its genetic health. Tests like preimplantation genetic testing (PGT) can give more insight into the embryo’s genetic health.
Other Factors Affecting Success
IVF success depends on many things, not just embryo quality. The uterus’s readiness, the embryologist’s skill, and the couple’s health also matter a lot.
Other important factors include:
- Age of the female partner
- Quality of sperm
- Uterine health and receptivity
- Lifestyle factors such as smoking and obesity
Knowing about these factors and how they relate to embryo quality is key. It helps manage expectations and improve IVF treatment.
Advanced Imaging Techniques in Embryo Assessment
Advanced imaging is changing how we check embryos for IVF. These new tools give a clearer view of embryo health. This helps increase the chances of a successful implantation.
Time-Lapse Monitoring
Time-lapse monitoring is a big step forward. It takes pictures of the embryo as it grows. This lets experts see how the embryo develops.
This method shows more than just static images. It spots small issues that might not be seen with the naked eye.
Artificial Intelligence in Embryo Selection
Artificial intelligence (AI) is now used in picking embryos. AI looks at lots of data from time-lapse images. It guesses how well an embryo might do.
This tech makes choosing embryos less about guesswork. It offers a fair and consistent way to pick the best ones.
Future Directions in Visual Assessment
The future of checking embryos looks bright. We’ll see even better imaging and AI tools. These will likely make IVF more successful.
Couples going through IVF should know about these new tools. Talking to their doctor about these advancements is key.
Conclusion: Understanding Your Embryo Report
Understanding your embryo report is key to knowing if your IVF treatment might work. The quality of your blastocysts is very important. This affects how likely you are to have a successful IVF.
Your report will show how your blastocysts are graded. This includes how well they’ve grown, the quality of the inner cells, and the outer cells. A well-developed blastocyst means you might have a better chance of implantation.
But, your report is just one part of the story. Other things like your age, egg quality, and health also matter. It’s smart to talk to your fertility specialist about your report. They can help you understand what it means for your treatment.
Knowing about your embryo report and what affects IVF success helps us make better choices. It also sets realistic hopes for your treatment’s outcome.
Faq
What is a blastocyst and how is it formed?
A blastocyst is an early stage of an embryo, about 5 days after fertilization. It forms through cell divisions and developmental milestones. It has an inner cell mass, trophectoderm, and a fluid-filled cavity.
What are the key components of a blastocyst?
A blastocyst has three main parts. The inner cell mass (ICM) forms the fetus. The trophectoderm (TE) forms the placenta. The blastocoel cavity is a fluid-filled space.
How are blastocysts graded, and what does it mean?
Blastocysts are graded using the Gardner system. It looks at expansion, inner cell mass, and trophectoderm quality. This grading helps predict implantation success.
What is the difference between a day 5 and day 6 blastocyst?
Day 5 blastocysts are more advanced and have a higher success rate in IVF. Day 6 blastocysts are also viable but have a slightly lower success rate.
How does the appearance of an embryo relate to IVF success?
The embryo’s appearance, as graded, is linked to IVF success. Yet, other factors like uterine receptivity and genetic issues also matter for success.
What are the different stages of blastocyst expansion?
Blastocyst expansion stages range from 1 to 6. Stage 1 is an early blastocyst, and stage 6 is fully hatched. Knowing these stages helps evaluate a blastocyst’s development.
What is the significance of inner cell mass (ICM) grading?
ICM grading looks at the cells in the inner cell mass. Grade A means many cells, while Grade C means few. It’s key for assessing a blastocyst’s quality.
How is trophectoderm (TE) grading done?
TE grading checks the cells in the trophectoderm. Grade A shows many cells, while Grade C shows few large cells. It’s important for evaluating a blastocyst.
What are the advanced imaging techniques used in embryo assessment?
Advanced imaging includes time-lapse monitoring and artificial intelligence. These technologies improve embryo selection and can boost IVF success.
How can I understand my embryo report?
To understand your embryo report, learn about the grading system. The report will detail expansion, inner cell mass, and trophectoderm quality. This helps grasp your embryos’ chances.
What is blastocyst expansion, and why is it important?
Blastocyst expansion is when the cavity grows, and the embryo changes. It’s vital for assessing a blastocyst’s development.
References
Medical News Today. (2025, February 26). How to prevent spinal stenosis: Tips, treatments, and more. This article focuses on core strengthening, balanced diet, quitting smoking, and maintaining moderate weight as key prevention strategies. https://www.medicalnewstoday.com/articles/how-to-prevent-spinal-stenosis