
At Liv Hospital, we understand the vital role of hematopoiesis. It’s how our bodies make billions of new blood cells every day. This complex process mainly happens in the bone marrow of adults. There, stem cells turn into different types of blood cells.
Hematopoiesis is key to keeping our blood cells healthy. These cells are essential for carrying oxygen, fighting off infections, and stopping bleeding. This detailed process is what keeps us alive, and any problems with it can cause health issues.

Hematopoiesis is the amazing way our bodies make blood cells. It’s key for keeping the right mix of blood cells. These cells carry oxygen, fight off infections, and help our blood clot.
Let’s dive into what hematopoiesis means. The words “hematopoiesis,” “hemopoiesis,” and “haematopoiesis” all mean the same thing. They come from Greek words for “blood” and “making.” So, hematopoiesis means “making blood.”
Over time, how we talk about hematopoiesis has changed. This change shows how much we’ve learned about making blood cells. Now, “hematopoiesis” and its friends are common in medical writing. They help us talk about how hematopoietic stem cells turn into different blood cells.
Hematopoiesis is vital for our health. It makes all blood cells: red, white, and platelets. Without it, our blood wouldn’t be healthy, causing many problems.
This process is very important. It changes how it makes blood cells based on what our body needs. For example, when we get sick, it makes more white blood cells to fight the infection.
Hematopoiesis, the process of making blood cells, has a long and changing history. Our knowledge of this complex process has grown a lot over time. It has moved from simple ideas to detailed scientific knowledge.
Looking back at the history of hematopoiesis helps us see how our understanding of blood cell creation has grown. This journey through hematopoietic science history shows us the key moments that have shaped what we know today.
In ancient times, how blood was made was a big mystery. People thought different organs made blood, with the liver being a top choice. But, our understanding was very basic until the microscope came along.
The microscope’s arrival in the 17th century was a big change. It let scientists see blood cells up close, helping them understand where they came from and what they did. The finding of red and white blood cells was a big step forward for studying hematopoiesis.
As science got better, so did our understanding of hematopoiesis. The 20th century brought big leaps, like finding hematopoietic stem cells. These cells are key for making all blood cell types. This finding changed the field, showing how all blood cells come from one source.
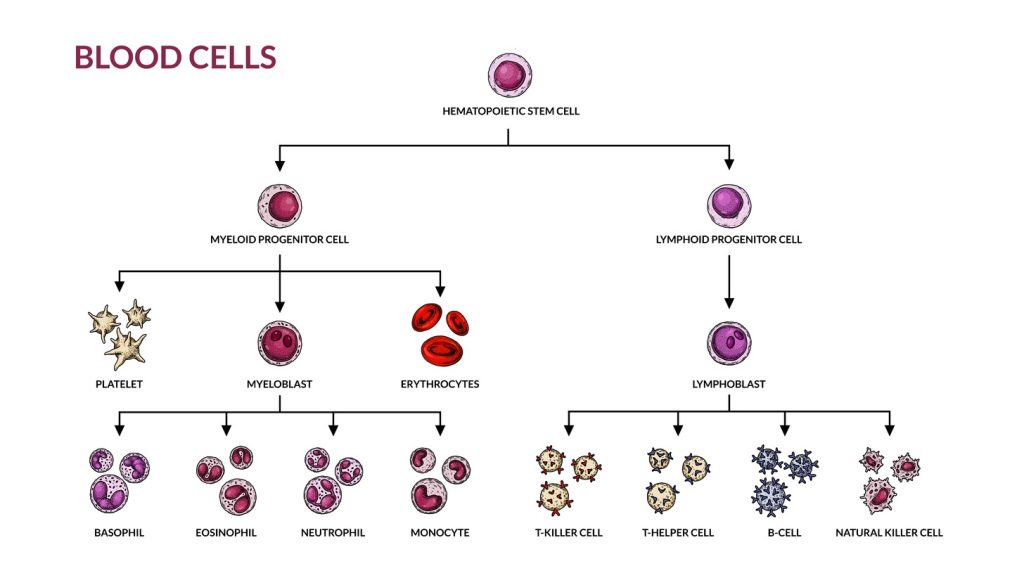
New lab tools and hematopoiesis charts or hematopoietic charts have also helped a lot. These tools make it easier to see how blood cells are made, from stem cells to fully formed cells.
Today, we keep adding to what we know about hematopoiesis. We’re learning more about it and how it affects health and disease. The history of hematopoiesis shows how far medical science has come. It helps us find better ways to treat blood-related problems.
Hematopoiesis is how stem cells turn into different blood cells. It’s a complex process that makes all blood cell types from hematopoietic stem cells. This is key for making red blood cells, white blood cells, and platelets. These cells are vital for carrying oxygen, fighting off infections, and clotting blood.
The journey of a hematopoietic stem cell to a mature blood cell has many stages. Stem cells can self-renew and turn into all blood cell types. As they change, they become more specific, leading to myeloid and lymphoid progenitor cells.
“The process of hematopoiesis is tightly regulated by a complex interplay of growth factors, cytokines, and transcription factors,” as noted in medical literature. These elements make sure the right blood cells are made in the right amounts.
The process of turning stem cells into specific blood cells is tightly controlled. Important factors include:
A hematopoiesis diagram or diagram of hematopoiesis shows this complex process. It shows how stem cells become all blood cell types. Knowing the blood cell lineage helps us understand how different blood cells are made and work.
Hematopoiesis, the creation of blood cells, happens in different places in our bodies. It changes as we grow from a baby to an adult. This process is complex and vital for our health.
In the early stages of development, blood cell creation starts in the yolk sac. Later, it moves to the liver and then to the bone marrow. The yolk sac is the first place where blood cells are made, starting around the third week of pregnancy. The liver takes over around the second month and keeps making blood cells until birth.
In adults, hematopoiesis mainly happens in the bone marrow of specific bones. The bone marrow, found in bones like the hips and thighbones, makes blood cells. It uses hematopoietic stem cells to create different types of blood cells.
In some diseases, blood cell creation happens outside the bone marrow, known as extramedullary hematopoiesis. This can occur in organs like the liver and spleen when the bone marrow is damaged. This can happen in conditions like myelofibrosis or other bone marrow problems.
| Stage of Development | Primary Site(s) of Hematopoiesis |
|---|---|
| Embryonic | Yolk sac, then liver |
| Fetal | Liver, then bone marrow |
| Adult | Bone marrow (specific bones like hips and femurs) |
| Disease States | Liver, spleen (extramedullary hematopoiesis) |
Hematopoietic stem cells are at the core of blood cell creation. They can renew themselves and turn into different blood cell types. These cells are key to hematopoiesis, keeping blood cell levels steady throughout our lives.
Hematopoietic stem cells have special traits that help them make blood cells. Self-renewal lets them keep their numbers up, ensuring a constant blood cell supply. They also have differentiation ability, turning into more specific cells that grow into different blood types.
Keeping a balance between self-renewal and differentiation is vital. Self-renewal keeps the stem cell pool steady, while differentiation makes mature blood cells. This balance is controlled by both the cells themselves and signals from their environment.
“The hematopoietic stem cell niche is a complex microenvironment that provides the necessary support for hematopoietic stem cell survival, self-renewal, and differentiation.”
The bone marrow has a special area called the stem cell niche. It supports hematopoietic stem cells. This niche includes osteoblasts, endothelial cells, and mesenchymal stromal cells. These cells make factors that help control the stem cells.
| Component | Function |
|---|---|
| Osteoblasts | Produce factors that support hematopoietic stem cell maintenance. |
| Endothelial Cells | Regulate hematopoietic stem cell homing and mobilization. |
| Mesenchymal Stromal Cells | Provide structural support and produce regulatory factors. |
Hematopoiesis diagrams are key to understanding blood cell formation. They show how blood cells are made from stem cells.
A hematopoietic chart maps out blood cell development. It starts with stem cells and ends with mature blood cells. It shows how stem cells turn into different blood cells, like red and white blood cells, and platelets.
To grasp a hematopoietic chart, we must know the cell types and their connections. The chart begins with hematopoietic stem cells. It then branches into different paths. For example, the myeloid lineage leads to red blood cells and platelets. The lymphoid lineage produces lymphocytes, like B and T cells.
The chart points out key blood cell production paths. These include:
Knowing these paths is vital for diagnosing and treating blood issues. For instance, problems in erythropoiesis can cause anemia. Issues in granulopoiesis can lead to low neutrophil counts. To learn more, visit this page.
The creation of red blood cells is vital for oxygen transport in our bodies. We’ll look into how these cells are made, the steps involved, and how the body controls their production.
Erythropoiesis starts with hematopoietic stem cells turning into erythroblasts. These cells go through several stages, like normoblasts and reticulocytes, before becoming mature red blood cells. This complex process involves significant changes to make cells ready to carry oxygen.
The stages of erythropoiesis are carefully managed to produce healthy red blood cells. Any problem in this process can cause blood disorders.
Erythropoietin is a hormone key to controlling erythropoiesis. It’s mainly made in the kidneys and tells the bone marrow to make more red blood cells. When oxygen levels drop, more erythropoietin is made, boosting red blood cell production to meet oxygen needs.
For more details on what triggers hematopoietic stem cells, see this resource: https://int.livhospital.com/what-stimulates-hematopoietic-stem-cells/.
In adults, hematopoiesis mainly happens in the bone marrow. The bone marrow is where hematopoietic stem cells turn into different blood cells, including red blood cells.
The bone marrow’s role in making new red blood cells is key for healthy blood counts and oxygen delivery to our tissues.
White blood cells are key in fighting infections. They are a vital part of our immune system. They help defend against harmful substances and pathogens.
There are different types of white blood cells. Each type has its own role and way of developing. We will look at granulocytes, monocytes, and lymphocytes and their roles in defending the body.
Granulocytes include neutrophils, eosinophils, and basophils. They have granules in their cells. These cells are important in fighting infections and in inflammatory reactions.
Monocytes are large white blood cells. They turn into macrophages, which clean up debris and pathogens. Macrophages are key in the innate immune response and help present antigens to lymphocytes.
Monocytes develop from hematopoietic stem cells. They then become monoblasts and mature into monocytes. These monocytes move into tissues, where they become macrophages.
Lymphocytes, including B cells, T cells, and NK cells, are vital in the adaptive immune response. They recognize and fight specific antigens. This is key in defending against infections.
The development of these lymphocytes is complex. It involves gene rearrangement to create diverse antigen receptors. This allows the immune system to recognize many pathogens.
Platelet production, or thrombopoiesis, is a complex process. Thrombopoiesis is key for making platelets. These platelets help stop bleeding and form blood clots.
The journey of thrombopoiesis starts with megakaryocytes. These large cells in the bone marrow make platelets. They grow and their nuclei get more complex as they mature.
As they mature, megakaryocytes send out proplatelet extensions. These thin, branching structures break into platelets. This process is controlled by growth factors and cytokines.
The release of platelets is carefully managed. The hormone thrombopoietin, made by the liver and kidneys, plays a big role. It helps megakaryocytes grow and release platelets.
Other factors also affect thrombopoiesis. Cytokines and growth factors help megakaryocytes develop and platelets form.
It’s important to understand how these factors work together. This helps us see how thrombopoiesis is managed and how problems can arise.
Understanding hematopoiesis is key to diagnosing and treating blood disorders. This process is vital for our health. Problems in it can lead to many clinical challenges.
Disorders in blood cell formation cause conditions like anemia and leukemia. These issues often stem from problems with stem cells or their environment. For example, aplastic anemia happens when the bone marrow can’t make blood cells.
Myeloproliferative neoplasms occur when there’s too much production of certain blood cells. Diagnosing these disorders involves clinical checks, lab tests, and sometimes bone marrow biopsies.
Diagnosing blood cell disorders has gotten better with new technologies. Tools like flow cytometry, genetic testing, and imaging studies are used. Flow cytometry helps identify abnormal cells.
Genetic tests find mutations linked to blood cancers, guiding treatments. Imaging, like PET scans, checks disease spread and treatment success. These tools help tailor treatments.
Treatments for blood cell disorders vary based on the condition. Some get supportive care like blood transfusions to manage symptoms. Others need stronger treatments like chemotherapy or stem cell transplants.
Stem cell transplants can cure some blood cancers by replacing bad cells with healthy ones. In summary, knowing about hematopoiesis is vital for managing blood disorders. Advanced diagnostics and treatments improve patient care and life quality.
Hematopoiesis is a complex process that keeps our blood healthy. It’s essential for delivering oxygen, fighting infections, and stopping bleeding.
The journey starts with hematopoietic stem cells. These cells turn into different blood cell types through detailed cellular processes.
Knowing about hematopoiesis helps us understand human physiology better. It also aids in diagnosing and treating blood-related disorders.
Learning about blood cell formation shows us the amazing processes that keep us alive. It also highlights the progress in hematology.
Hematopoiesis is how our body makes blood cells. This includes red blood cells, white blood cells, and platelets. It happens in the bone marrow and keeps our blood healthy.
Adults make blood cells in the bone marrow of certain bones. These bones are in the pelvis, vertebrae, and femur.
Hematopoietic stem cells are key in making blood cells. They can grow more of themselves and turn into different blood cell types.
Diagrams of hematopoiesis show how blood cells are made. They show the steps from stem cells to different blood cell types.
Erythropoiesis is making red blood cells. It happens in the bone marrow and is controlled by erythropoietin. New red blood cells are made here.
Thrombopoiesis is making platelets. It involves growing and maturing megakaryocytes. It’s controlled by thrombopoietin and other factors.
Disorders of hematopoiesis can cause blood diseases. Knowing about these disorders helps us find new treatments and tests.
Extramedullary hematopoiesis is making blood cells outside the bone marrow. It happens when the body is sick or under stress.
Hematopoiesis is controlled by many factors. These include growth factors, cytokines, and other molecules. They help blood cells grow, change, and live.
Knowing about hematopoiesis helps us understand how blood cells are made. It’s key for finding new ways to treat blood diseases.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us