When we talk about myocardial infarction, we’re referring to a serious medical condition commonly known as a heart attack. This occurs when the blood flow to the heart is suddenly blocked, causing damage to the heart muscle. According to global health research, cardiovascular diseases, including myocardial infarction, are the leading cause of death worldwide.
At Liv Hospital, we understand the significance of myocardial infarction in cardiovascular health. Our team of experts is dedicated to providing clarity and care to patients facing this life-altering condition. We believe in empowering our patients with knowledge, so they can make informed decisions about their health.
Key Takeaways
- Myocardial Infarction (MI) is commonly known as a heart attack.
- MI occurs when blood flow to the heart is blocked, damaging the heart muscle.
- Cardiovascular diseases are the leading cause of global deaths.
- Liv Hospital provides expert care and support for patients with MI.
- Understanding MI is crucial for maintaining cardiovascular health.
What Does MI Mean in Medical Terms
Understanding the term “MI” in medical terms is crucial for patients and healthcare professionals alike. Myocardial Infarction (MI) is a serious medical condition that occurs when the blood flow to the heart is severely blocked, causing damage to the heart muscle.
Definition and Medical Terminology
Myocardial Infarction (MI), commonly known as a heart attack, occurs when the flow of blood to a part of the heart is blocked for a long enough time that part of the heart muscle is damaged or dies. This is most often caused by a blockage in one or more of the coronary arteries due to plaque (a mix of fat, cholesterol, and other substances). The medical term “Myocardial Infarction” is derived from the Greek words “myo” (muscle), “cardia” (heart), and “infarction” (death of tissue due to lack of blood supply).
MI vs. Other Cardiac Conditions
It’s essential to distinguish MI from other cardiac conditions such as cardiac arrest. While both are serious heart conditions, they are different in their causes and effects. Cardiac arrest occurs when the heart suddenly stops beating, which can be due to various reasons, including MI. MI is specifically related to the blockage of blood flow to the heart muscle, leading to tissue damage or death.
Common Terminology Variants and Translations
MI is known by different terms in various languages and medical contexts. For instance, in French, it’s referred to as “infarctus du myocarde.” Understanding these variations is crucial for effective communication among healthcare professionals globally. The table below highlights some common terminology variants and translations.
| Language | Term for Myocardial Infarction (MI) |
|---|---|
| English | Myocardial Infarction (MI) |
| French | Infarctus du Myocarde |
| Spanish | Infarto de Miocardio |
As healthcare continues to become more global, understanding these terms can help in providing better care for international patients.
The Historical Understanding of Myocardial Infarction

Historically, the understanding and diagnosis of MI have undergone substantial transformations. The journey to our current understanding of myocardial infarction has been long and complex, involving numerous discoveries and advancements in medical science.
Evolution of MI Diagnosis Through History
The diagnosis of MI has evolved significantly over the decades. Initially, MI was identified through clinical presentation and basic diagnostic tools. Advances in electrocardiography (ECG) and biochemical markers have revolutionized the diagnosis, enabling healthcare providers to identify MI more accurately and promptly.
Key Discoveries in Understanding Heart Attacks
Several key discoveries have shaped our understanding of heart attacks. The recognition of coronary artery disease as a primary cause of MI and the development of cardiac biomarkers such as troponin have been crucial. These advancements have improved diagnostic accuracy and guided treatment strategies.
Development of Modern Cardiac Care
Modern cardiac care has been influenced by historical insights and technological advancements. The development of coronary care units (CCUs) and reperfusion therapies such as thrombolysis and percutaneous coronary intervention (PCI) has significantly improved outcomes for patients with MI.
| Decade | Major Advancements in MI Diagnosis and Treatment |
|---|---|
| 1960s | Introduction of Coronary Care Units (CCUs) |
| 1980s | Development of Thrombolytic Therapy |
| 1990s | Advancements in Percutaneous Coronary Intervention (PCI) |
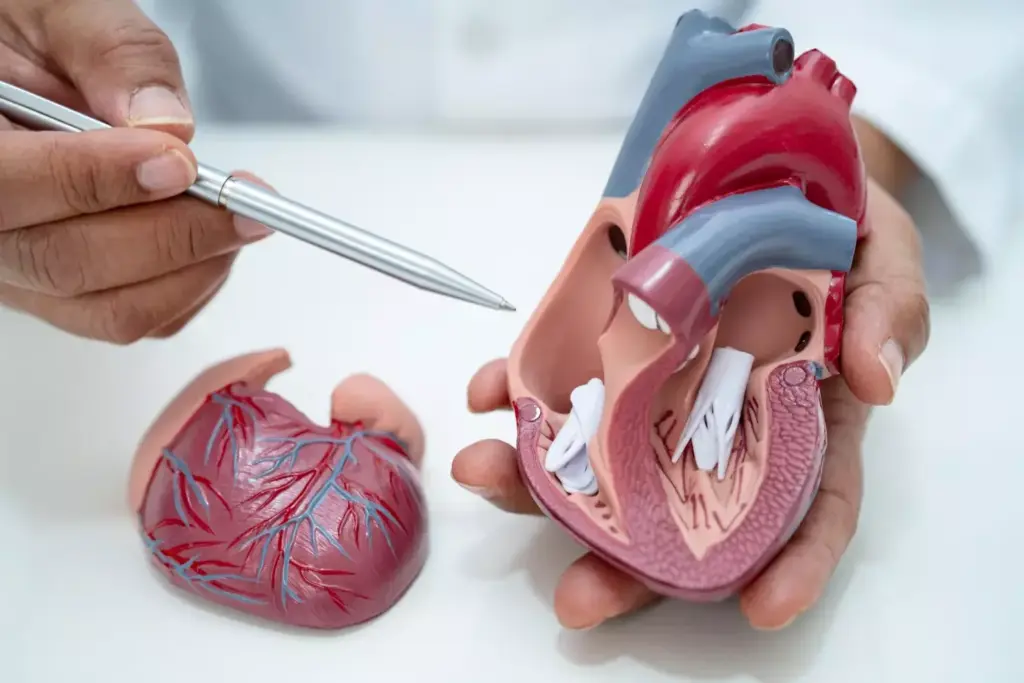
Anatomy of the Heart and Coronary Circulation
The anatomy of the heart, particularly its coronary circulation, is fundamental to understanding cardiac conditions like MI. The heart is a muscular organ that pumps blood throughout the body, and its function is highly dependent on its intricate structure.
Structure and Function of the Myocardium
The myocardium is the middle layer of the heart wall, composed of cardiac muscle cells. It is responsible for the heart’s ability to contract and pump blood. The myocardium requires a constant supply of oxygen and nutrients to function properly.
Coronary Arteries and Their Role
The coronary arteries supply blood to the heart muscle itself. The two main coronary arteries are the left and right coronary arteries, which branch off into smaller arteries. These arteries are crucial for delivering oxygen and nutrients to the myocardium.
Blood Supply to the Heart Muscle
The blood supply to the heart muscle is essential for its function. The coronary arteries ensure that the myocardium receives the necessary oxygen and nutrients. Any blockage in these arteries can lead to myocardial infarction.
| Coronary Artery | Region Supplied | Function |
|---|---|---|
| Left Coronary Artery | Anterior and lateral walls of the heart | Supplies blood to a significant portion of the heart muscle |
| Right Coronary Artery | Right atrium, right ventricle, and parts of the left ventricle | Supplies blood to the right side of the heart and parts of the left ventricle |
Understanding the anatomy of the heart and its coronary circulation is vital for comprehending the mechanisms behind myocardial infarction and for developing effective treatment strategies.
Pathophysiology of Acute Myocardial Infarction (AMI Disease)
The pathophysiology of AMI involves a multifaceted process that ultimately leads to the blockage of coronary arteries, resulting in heart muscle damage. This complex process is initiated by the rupture of an atherosclerotic plaque within a coronary artery, which exposes highly thrombogenic lipid-rich material to the bloodstream.
The Process of Coronary Artery Blockage
When a plaque ruptures, it triggers the activation of platelets and the coagulation cascade, leading to the formation of a thrombus that can occlude the coronary artery. This occlusion severely reduces or completely blocks blood flow to the downstream myocardium, causing ischemia and eventually infarction.
Myocardial Infarction Zones
The area affected by the myocardial infarction can be divided into distinct zones, each with different pathological characteristics. The necrotic core is the central area where the cells have died due to prolonged ischemia. Surrounding this core is the area of injury, where cells are severely damaged but may still be salvageable with prompt treatment. The outermost zone is the ischemic zone, where cells are ischemic but not yet infarcted.
Cellular Changes During Myocardial Infarction
During AMI, the lack of blood flow leads to a series of cellular changes. Initially, the cells switch from aerobic to anaerobic metabolism, leading to a buildup of lactic acid and a decrease in ATP production. As the ischemia persists, cellular damage progresses, leading to cell death and the release of various biomarkers into the bloodstream, such as troponin.
Understanding these cellular changes and the different zones of myocardial infarction is crucial for developing effective treatment strategies and improving patient outcomes.
Types and Classifications of MI
Understanding the different types of myocardial infarction is crucial for accurate diagnosis and effective treatment. Myocardial infarction, commonly known as a heart attack, occurs when blood flow to the heart is severely blocked, causing damage to the heart muscle.
STEMI: ST-Elevation Myocardial Infarction
STEMI is a type of MI characterized by a complete blockage of a coronary artery, leading to significant damage to the heart muscle. It is diagnosed based on ST-segment elevation on an electrocardiogram (ECG).
NSTEMI: Non-ST-Elevation Myocardial Infarction
NSTEMI occurs when there is a partial blockage of a coronary artery. The ECG does not show ST-segment elevation, but cardiac biomarkers are elevated, indicating heart muscle damage.
The distinction between STEMI and NSTEMI is critical because it guides treatment decisions. STEMI typically requires immediate reperfusion therapy, such as thrombolysis or primary percutaneous coronary intervention (PCI).
The Five Clinical Types of MI
The universal definition of myocardial infarction recognizes five clinical types of MI, each with different pathophysiological mechanisms:
- Type 1: Spontaneous MI related to ischemia due to a primary coronary event.
- Type 2: MI secondary to ischemia due to either increased oxygen demand or decreased supply.
- Type 3: Sudden unexpected cardiac death, including cardiac arrest.
- Type 4: MI associated with PCI.
- Type 5: MI associated with coronary artery bypass grafting (CABG).
Differentiating MI from Cardiac Arrest
While MI can lead to cardiac arrest, they are distinct clinical entities. Cardiac arrest is a sudden loss of cardiac function, whereas MI refers specifically to the damage caused by interrupted blood flow to the heart muscle.
Here’s a comparison of STEMI and NSTEMI in a tabular format:
| Characteristics | STEMI | NSTEMI |
|---|---|---|
| ECG Findings | ST-segment elevation | No ST-segment elevation |
| Coronary Artery Status | Complete blockage | Partial blockage |
| Immediate Treatment | Reperfusion therapy (thrombolysis or PCI) | Antithrombotic therapy, possible PCI |
Clinical Presentation and Symptoms
Understanding the clinical presentation of myocardial infarction is crucial for timely medical intervention. Myocardial infarction, or heart attack, occurs when the blood flow to the heart is severely blocked, causing damage to the heart muscle. Recognizing the symptoms promptly can significantly improve patient outcomes.
Classic Symptoms of Myocardial Infarction
The classic symptoms of myocardial infarction include chest pain or discomfort, often described as a pressure or tightness in the chest that may radiate to the arm, neck, or jaw. Other common symptoms are shortness of breath, cold sweats, nausea, and lightheadedness. These symptoms can vary in intensity and may not always be typical.
Atypical Presentations
Atypical presentations of MI can be more subtle and may not always include chest pain. Some individuals may experience fatigue, dizziness, or confusion, particularly in older adults or those with diabetes. These atypical symptoms can make diagnosis more challenging, emphasizing the need for a thorough medical evaluation.
Silent Myocardial Infarctions
Silent myocardial infarctions occur without noticeable symptoms and are often discovered during later medical evaluations. These events are more common in people with diabetes or those who have had a previous MI. Regular check-ups and screening tests are crucial for detecting silent MIs.
When to Seek Emergency Care
If you or someone else is experiencing symptoms of myocardial infarction, it is essential to seek emergency care immediately. Prompt treatment can minimize damage to the heart muscle and improve survival chances. We emphasize the importance of acting quickly if symptoms persist or worsen over time.
Risk Factors and Prevention
Understanding the risk factors associated with myocardial infarction is crucial for effective prevention and management. Myocardial infarction, commonly known as a heart attack, occurs when the flow of blood to a part of the heart is blocked for a long enough time that part of the heart muscle is damaged or dies. This condition is a leading cause of morbidity and mortality worldwide.
Modifiable Risk Factors
Several risk factors for myocardial infarction can be modified through lifestyle changes or medical interventions. These include:
- Smoking: Smoking is a significant risk factor for MI, as it damages the inner lining of blood vessels and makes them more susceptible to blockage.
- Hypertension: High blood pressure can cause damage to the arteries, making them more prone to narrowing and blockage.
- High Cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol can lead to plaque buildup in arteries, increasing the risk of MI.
- Diabetes: Diabetes mellitus is a risk factor for cardiovascular disease, including MI, due to its effects on blood vessels and nerves.
- Obesity and Physical Inactivity: Being overweight or obese and leading a sedentary lifestyle can increase the risk of developing conditions that contribute to MI.
Non-Modifiable Risk Factors
Some risk factors cannot be changed, including:
- Age: The risk of MI increases with age, particularly after the age of 45 for men and 55 for women.
- Family History: A family history of early heart disease is a risk factor for MI.
- Gender: Men are generally at higher risk of MI than women, although the risk for women increases after menopause.
Primary Prevention Strategies
Primary prevention involves measures to prevent the occurrence of MI in the first place. This includes:
- Lifestyle Modifications: Adopting a healthy diet, engaging in regular physical activity, maintaining a healthy weight, and quitting smoking.
- Management of Risk Factors: Controlling hypertension, diabetes, and high cholesterol through lifestyle changes and, when necessary, medication.
Secondary Prevention After MI
For individuals who have already experienced an MI, secondary prevention is crucial to prevent recurrence. This includes:
- Medication: Use of antiplatelet agents, beta-blockers, ACE inhibitors, and statins as prescribed by a healthcare provider.
- Cardiac Rehabilitation: Participation in a structured program that includes exercise training, education on heart-healthy living, and counseling.
- Lifestyle Changes: Continuing the lifestyle modifications initiated during primary prevention.
By understanding and addressing both modifiable and non-modifiable risk factors, we can significantly reduce the incidence of myocardial infarction and improve outcomes for those affected.
Diagnosis and Modern Cardiac Care Protocols
Accurate diagnosis of myocardial infarction is crucial for effective management and relies on a combination of clinical evaluation, ECG analysis, and biomarker assessment. We will outline the key steps and modern protocols used in diagnosing MI.
Initial Assessment and Triage
The initial assessment of a patient suspected of having an MI involves a rapid evaluation of symptoms, medical history, and risk factors. We use this information to determine the likelihood of MI and guide further diagnostic testing.
Electrocardiogram (ECG) Findings
The electrocardiogram is a critical tool in diagnosing MI, providing immediate information about the heart’s electrical activity. We look for specific changes such as ST-segment elevation or depression, Q-waves, and T-wave inversion, which can indicate ischemia or infarction.
Cardiac Biomarkers
Cardiac biomarkers, particularly troponin, are essential for diagnosing MI. Elevated levels of these biomarkers in the blood indicate myocardial damage. We measure troponin levels to confirm or rule out MI.
Advanced Imaging Techniques
Advanced imaging techniques, including echocardiography and cardiac MRI, provide valuable information about cardiac structure and function. We use these techniques to assess the extent of myocardial damage and guide treatment decisions.
| Diagnostic Tool | Primary Use in MI Diagnosis | Key Findings |
|---|---|---|
| Electrocardiogram (ECG) | Initial assessment of ischemia or infarction | ST-segment changes, Q-waves, T-wave inversion |
| Cardiac Biomarkers | Detection of myocardial damage | Elevated troponin levels |
| Echocardiography | Assessment of cardiac function and structure | Wall motion abnormalities, ejection fraction |
| Cardiac MRI | Detailed assessment of myocardial damage | Extent of infarction, viability assessment |
By combining these diagnostic approaches, we can accurately diagnose MI and develop an effective treatment plan tailored to the individual patient’s needs.
Treatment Approaches and Interventions
Treating myocardial infarction effectively necessitates a comprehensive strategy that encompasses emergency response, pharmacological treatment, and reperfusion techniques. We will explore the various approaches and interventions used to manage MI.
Emergency Management
Emergency management is critical in the treatment of myocardial infarction. It involves immediate actions to stabilize the patient, including cardiac monitoring and administration of oxygen if necessary. We also provide initial pharmacological interventions to alleviate symptoms and prevent further damage.
Pharmacological Interventions
Pharmacological interventions play a crucial role in managing MI. These include:
- Antiplatelet therapy to prevent further clot formation
- Anticoagulation to prevent new clots and reduce the risk of existing clot enlargement
- Beta-blockers to reduce myocardial oxygen demand
- ACE inhibitors or ARBs to reduce blood pressure and decrease the heart’s workload
Reperfusion Strategies
Reperfusion strategies aim to restore blood flow to the affected myocardium. The primary methods include:
- Thrombolysis: Administering thrombolytic agents to dissolve the occluding thrombus
- Primary Percutaneous Coronary Intervention (PCI): A catheter-based procedure to mechanically open the occluded artery
Rehabilitation After MI
Rehabilitation after myocardial infarction is essential for improving outcomes and reducing morbidity. It typically involves a multidisciplinary approach, including exercise training, dietary counseling, and psychological support. We tailor rehabilitation programs to individual patient needs, aiming to enhance cardiovascular health and overall well-being.
By combining emergency management, pharmacological interventions, reperfusion strategies, and rehabilitation, we can significantly improve the prognosis for patients with myocardial infarction.
Complications and Long-Term Prognosis
The aftermath of a myocardial infarction can be complex, involving immediate complications and long-term effects on the heart. Understanding these aspects is crucial for managing patient care effectively.
Immediate Complications
Immediate complications following MI can be life-threatening. These include arrhythmias, heart failure, and mechanical complications such as ventricular septal defect or free wall rupture. Prompt medical intervention is critical to mitigate these risks.
Long-Term Sequelae
Long-term sequelae of MI can significantly impact a patient’s quality of life. Reduced left ventricular function is a common consequence, potentially leading to heart failure. We must monitor patients closely to manage these conditions effectively.
Factors Affecting Survival and Recovery
Several factors influence survival and recovery after MI, including the extent of cardiac damage, presence of comorbid conditions, and the timeliness and effectiveness of initial treatment. Early intervention and rehabilitation play a crucial role in improving outcomes.
Quality of Life After Myocardial Infarction
Improving quality of life after MI involves a multifaceted approach, including lifestyle modifications, medication adherence, and ongoing medical care. We work closely with patients to develop personalized care plans that address their specific needs and goals.
By understanding the complications and long-term prognosis of MI, we can provide comprehensive care that enhances patient outcomes and improves quality of life.
Conclusion: The Importance of Understanding MI for Cardiovascular Health
Understanding myocardial infarction (MI) is crucial for maintaining cardiovascular health. Throughout this article, we have explored the definition, diagnosis, and treatment of MI, highlighting its significance in the context of heart health.
The importance of understanding MI lies in its impact on our ability to prevent, diagnose, and manage heart attacks effectively. By recognizing the risk factors and symptoms associated with MI, individuals can seek timely medical intervention, thereby improving outcomes and reducing the risk of complications.
Promoting awareness and education about MI is essential for enhancing cardiovascular health. We emphasize the need for continued research and education in this area to support individuals in making informed decisions about their heart health.
By fostering a deeper understanding of MI and its implications for cardiovascular health, we can work towards reducing the incidence of heart attacks and improving the quality of life for those affected.
What does MI stand for in medical terms?
MI stands for Myocardial Infarction, commonly known as a heart attack, which occurs when the blood flow to the heart is blocked, causing damage to the heart muscle.
What is the difference between MI and cardiac arrest?
MI refers to the damage to the heart muscle due to a blockage in the coronary arteries, while cardiac arrest is a sudden loss of heart function, often due to abnormal heart rhythms. Although related, they are distinct conditions.
What are the classic symptoms of a myocardial infarction?
Classic symptoms include chest pain or discomfort, shortness of breath, lightheadedness, and pain or discomfort in one or both arms, the back, neck, jaw, or stomach. However, symptoms can vary and some MIs can be silent.
What are the risk factors for developing MI?
Risk factors include modifiable factors such as smoking, hypertension, high cholesterol, diabetes, and obesity, as well as non-modifiable factors like age, family history, and genetic predisposition.
How is MI diagnosed?
Diagnosis involves initial assessment and triage, electrocardiogram (ECG) findings, cardiac biomarkers such as troponin, and advanced imaging techniques like echocardiography and cardiac MRI.
What are the treatment approaches for MI?
Treatment includes emergency management with pharmacological interventions like antiplatelet therapy and anticoagulation, reperfusion strategies such as thrombolysis and primary percutaneous coronary intervention (PCI), and rehabilitation after MI.
What are the complications of MI?
Immediate complications can include arrhythmias and heart failure, while long-term sequelae may involve reduced left ventricular function. Factors affecting survival and recovery include the severity of the MI, promptness and effectiveness of treatment, and ongoing management of risk factors.
How can MI be prevented?
Primary prevention involves lifestyle modifications such as a healthy diet, regular exercise, not smoking, and managing conditions like hypertension and diabetes. Secondary prevention after MI includes medication, cardiac rehabilitation, and continued lifestyle changes to prevent recurrent MI.
What is the significance of understanding MI for cardiovascular health?
Understanding MI is crucial for promoting cardiovascular health, as it allows for the recognition of risk factors, prompt identification of symptoms, and appropriate management and prevention strategies to reduce morbidity and mortality.



































