At Liv Hospital, we know how vital accurate diagnosis and treatment planning are for prostate cancer patients. PSMA PET imaging has changed the game, being more sensitive and specific than old methods. Many patients ask what does psma uptake mean, which refers to how much the prostate cancer cells are absorbing the PSMA tracer, indicating tumor activity and aggressiveness.
PSMA uptake means radiotracers bind to the Prostate-Specific Membrane Antigen (PSMA) on prostate cancer cells. This is key to finding prostate cancer in the body. It helps us pinpoint and assess cancer sites for diagnosis, staging, or if it has come back.
Using PET imaging with PSMA-targeting radiotracers boosts our ability to diagnose prostate cancer. It can change how we manage treatment in up to 30% of cases. Knowing about PSMA uptake is essential for those seeking advanced medical care and support.
Key Takeaways
- PSMA PET imaging offers greater sensitivity and specificity than conventional imaging methods.
- PSMA uptake refers to the accumulation of radiotracers that bind to the Prostate-Specific Membrane Antigen.
- High PSMA uptake highlights possible prostate cancer sites in the body.
- PET imaging with PSMA-targeting radiotracers can greatly improve diagnostic accuracy.
- Understanding PSMA uptake is key to effective prostate cancer diagnosis and treatment planning.
The Basics of PSMA and Its Role in Prostate Cancer
PSMA is a protein found on prostate cancer cells. It’s key for detecting cancer through imaging. Knowing about PSMA helps doctors understand PET scans better.
What is Prostate-Specific Membrane Antigen (PSMA)?
PSMA is a protein found in prostate cancer cells. It’s also known as glutamate carboxypeptidase II or folate hydrolase. PSMA is not exclusive to prostate cancer, as it’s found in other tissues too, but at lower levels.
PSMA is important because it’s more active in aggressive prostate cancer. This makes it a great marker for finding and tracking prostate cancer.
Expression Patterns in Normal and Cancerous Tissue
In normal tissue, PSMA is present but not much. But in prostate cancer, it’s much more active. The amount of PSMA varies with the cancer type and stage.
- High-grade prostate cancers have more PSMA, making them easier to spot with PSMA-targeted PET imaging.
- Metastatic prostate cancer also shows more PSMA, helping find cancer in other parts of the body.
- Some research links PSMA to castration-resistant prostate cancer, where cancer grows despite hormone therapy.
Knowing how PSMA works helps doctors understand PET scan results. This leads to better treatment plans.
Understanding PET Imaging Technology
Positron Emission Tomography (PET) imaging is a cutting-edge tool for diagnosing diseases. It shows how cells in the body work. This helps doctors find and treat diseases like cancer.
How PET Scans Work
PET scans use tiny amounts of radioactive tracers. These tracers go to areas where cells are very active, like in cancer. The scanner picks up signals from these tracers, making detailed images of the body’s metabolic processes.
The steps to get these images are:
- Injecting a radioactive tracer that cells absorb in a certain way.
- The tracer releases positrons that collide with electrons, making gamma rays detected by the scanner.
- The scanner turns this data into images showing where the tracer is in the body.
Integration with CT and MRI
PET scans are often used with CT and MRI to get a full picture of the body. This mix helps doctors see both how the body works and its structure. It makes diagnosing diseases more accurate.
Benefits of Integrated Imaging:
- It combines functional and anatomical info for better diagnoses.
- It helps find and stage diseases, like cancer, better.
- It guides biopsies and treatments by showing exactly where to go.
Using PET with CT or MRI gives doctors a clearer view of what’s going on in the body. This helps make treatment plans more informed. It’s a big step forward in medical imaging, helping both patients and doctors make better decisions.
PSMA-Targeted Radiotracers in PET Imaging
In the world of prostate cancer imaging, PSMA-targeted radiotracers are key. They are made to stick to the Prostate-Specific Membrane Antigen (PSMA). This is a protein often found in more in prostate cancer cells. Thanks to these radiotracers, PET imaging can now better find and understand prostate cancer.
Types of PSMA Radiotracers
Many PSMA radiotracers are used in clinics, each with its own benefits. Some top ones are Ga-PSMA-11, F-PSMA-1007, and F-DCFPyL. They differ in how well they stick to PSMA, how they spread in the body, and how long they last.
| Radiotracer | Binding Affinity | Biodistribution | Half-life |
| Ga-PSMA-11 | High | Renal excretion | 68 minutes |
| F-PSMA-1007 | High | Hepatobiliary excretion | 110 minutes |
| F-DCFPyL | High | Renal excretion | 110 minutes |
How Radiotracers Bind to PSMA
PSMA radiotracers attach to the outside part of the PSMA protein. This protein is abundant in prostate cancer cells. This precise sticking lets us clearly see prostate cancer spots. A study on PMC shows these radiotracers are very good at finding prostate cancer.
What Does PSMA Uptake Mean in Clinical Context
PSMA uptake in PET scans gives us clues about prostate cancer. It helps doctors know if the cancer is present and how aggressive it is. This knowledge is key to making the right diagnosis and treatment plan.
Normal vs. Abnormal PSMA Uptake Patterns
PSMA is not just found in cancer cells. It can also show up in some normal tissues and benign conditions. Normal PSMA uptake is seen in salivary glands, lacrimal glands, and parts of the gut. On the other hand, abnormal PSMA uptake is linked to prostate cancer, mainly in cases of metastasis or recurrence.
It’s important to look at the intensity, location, and pattern of PSMA uptake. For example, high PSMA uptake in the prostate or pelvic lymph nodes might mean cancer. But mild uptake in some normal tissues is usually okay.
Correlation with Disease Presence and Aggressiveness
The level and pattern of PSMA uptake tell us a lot about prostate cancer. Research shows that higher PSMA uptake is linked to more aggressive cancer and a higher chance of spreading.
| PSMA Uptake Pattern | Clinical Implication |
| Low-level uptake in the prostate | May indicate low-risk or localized disease |
| High-level uptake in the prostate | Suggests potentially aggressive or locally advanced disease |
| Uptake in pelvic lymph nodes | May indicate regional metastasis |
| Uptake in distant sites (e.g., bone, distant lymph nodes) | Indicative of metastatic disease |
By studying PSMA uptake patterns, doctors can understand how widespread and aggressive prostate cancer is. This helps them make better treatment choices and improve patient care.
Interpreting PSMA PET Scan Results
When we look at PSMA PET scans, we check the standardized uptake value (SUV) and how the scan looks. Getting this right is key to managing prostate cancer well.
Standardized Uptake Value (SUV) Explained
The Standardized Uptake Value (SUV) shows how much PSMA is taken up in PET scans. It helps us see how much of the tracer is in different parts of the body. A higher SUV means more uptake, which might mean cancer.
When we look at SUV values, we must think about the patient’s weight, the tracer dose, and when the scan was done. These things can change SUV numbers and need to be the same for fair comparisons.
Visual Assessment Criteria
Looking at the scan’s pattern and how much PSMA is taken up is called visual assessment. This method helps spot abnormal areas that might be cancer. We look at where the lesions are, how big they are, and how intense they are. We also watch out for any false positives or artifacts.
Using both visual assessment and SUV values makes PSMA PET scans more accurate. It gives a clearer picture of how much cancer there is and how aggressive it might be.
Common Reporting Systems and Scales
There are many ways to report PSMA PET scan results. The PET Prostate Reporting and Data System (PERS) is one. These systems help sort findings based on how likely they are to be cancer.
Using these systems helps doctors talk clearly and make the same decisions. It makes sure PSMA PET scan results are always reported the same way. This helps patients get better care.
Patient Experience and Preparation for PSMA PET Imaging
Understanding the steps for PSMA PET imaging can make the experience better. Getting ready right is important for a good scan. This helps doctors make accurate diagnoses and plans for treatment.
Before the Scan: Preparation Guidelines
There are key steps to take before a PSMA PET scan. Always follow your doctor’s specific instructions because they can change based on your situation.
- Tell your doctor about any medicines you’re taking. Some might need to be changed or stopped before the scan.
- Drink plenty of water before the scan. This can make the images clearer.
- Don’t eat big meals or drink caffeine close to the scan time. These can mess with the radiotracer’s spread.
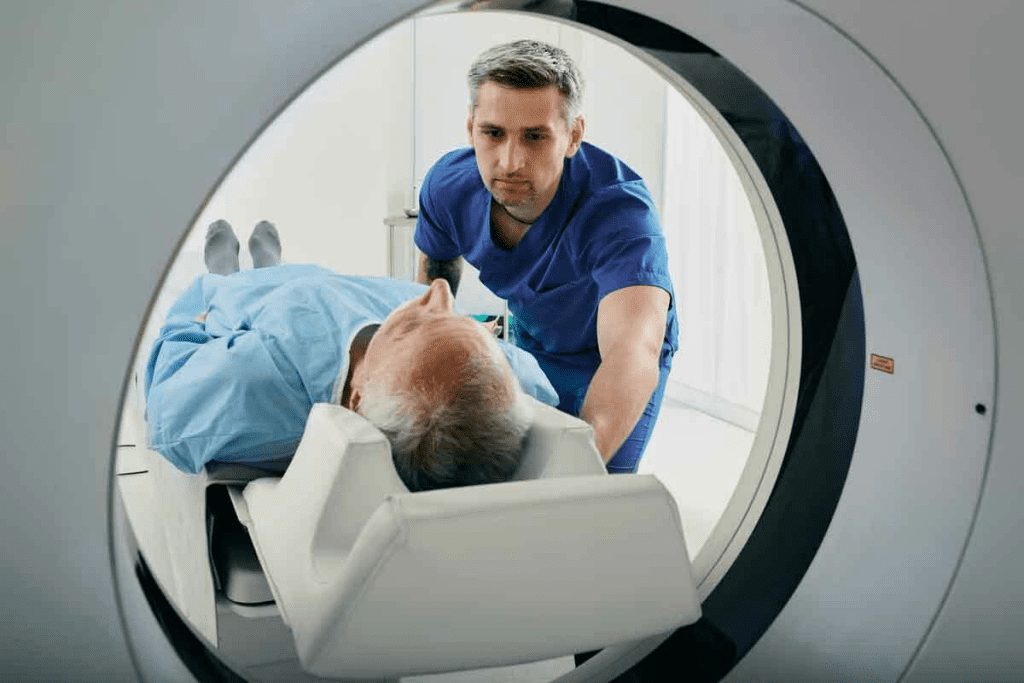
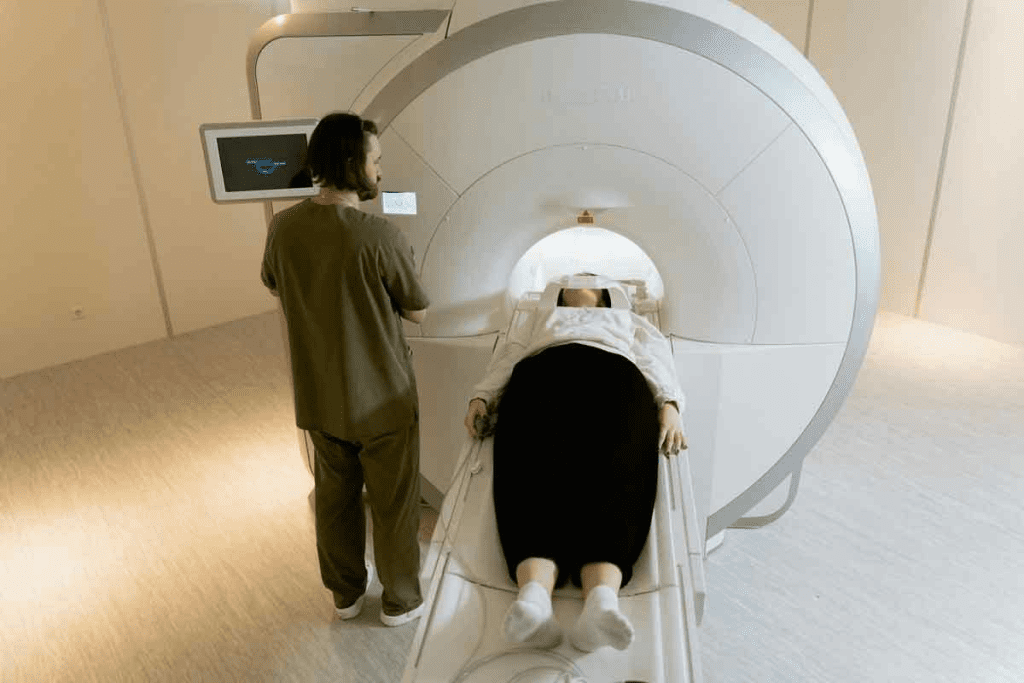
During and After the Procedure
During the scan, you’ll get a small dose of radioactive material. This targets PSMA. The scan uses a PET/CT scanner to mix functional PET info with CT anatomy.
The scan is usually easy to handle. Most people don’t feel any bad effects. You’ll need to stay very quiet and calm on the table for 30-60 minutes.
After that, you can go back to your usual activities unless your doctor says not to. Drink lots of water to get rid of the radiotracer.
Knowing what happens during and after the scan can reduce stress. It helps you feel more ready for the procedure.
Clinical Applications of PSMA PET Imaging
PSMA PET imaging is a key tool in fighting prostate cancer. It’s very good at finding cancer and planning treatments. This makes it very important in doctors’ offices.
Initial Diagnosis and Staging
PSMA PET imaging is vital for starting to treat prostate cancer. It shows where the cancer is and if it has spread. This helps doctors know how to treat it best.
- Detection of primary prostate cancer
- Identification of lymph node metastases
- Detection of distant metastases
This info is key for figuring out how far the cancer has spread. It helps doctors plan the best treatment.
Biochemical Recurrence Detection
For those with cancer coming back, PSMA PET imaging is a great tool. It finds cancer even when PSA levels are low. This means doctors can act fast.
- Early detection of recurrence
- Localization of recurrent disease
- Guiding salvage therapy
Treatment Planning and Monitoring
PSMA PET imaging is also key in planning and checking on treatments. It helps see how well treatments are working. This helps doctors make changes if needed.
- Assessing treatment response
- Monitoring disease progression
- Guiding targeted therapies
Using PSMA PET imaging in care makes treatment more personal and effective. This is great news for prostate cancer patients.
Comparing PSMA PET to Conventional Imaging Methods
PSMA PET imaging is much better than old methods like CT scans and bone scans for finding prostate cancer. These old methods can miss small cancer spots or not show how far the cancer has spread.
PSMA PET, though, gives a clearer picture by focusing on the Prostate-Specific Membrane Antigen. It’s more accurate, helping find cancer in lymph nodes and when it comes back.
Sensitivity and Specificity Advantages
PSMA PET is way more sensitive and specific than old imaging. It can spot cancer coming back even when PSA levels are very low. This is something old methods can’t do.
Key advantages include:
- Higher detection rate of metastatic sites
- Improved accuracy in identifying lymph node involvement
- Better differentiation between benign and malignant lesions
| Imaging Modality | Sensitivity | Specificity |
| PSMA PET | 85-95% | 90-98% |
| Conventional CT | 60-70% | 70-80% |
| Bone Scan | 70-80% | 60-70% |
Impact on Clinical Management Decisions
PSMA PET’s better accuracy changes how doctors plan treatment. It helps doctors see exactly how far the cancer has spread. This means they can make more precise treatment plans.
For example, finding cancer in just a few places means doctors can use targeted treatments like SBRT. This can lead to better results and fewer side effects for patients.
In short, PSMA PET is a big step up from old imaging methods. It helps doctors make better treatment plans, which is good for patients with prostate cancer.
Potential False Positives and Limitations
PSMA PET imaging has changed how we diagnose prostate cancer. But, it’s important to know its possible false positives and limits. Understanding these helps us give the best care to our patients.
Non-Prostatic PSMA Expression
PSMA PET imaging faces a big challenge: non-prostatic PSMA expression. This can cause false positives. PSMA is found in prostate cancer cells, but also in normal tissues and other cancers. For example, PSMA expression has been observed in certain benign conditions like osteoblastic activity and in some non-prostate cancers.
Examples of non-prostatic PSMA expression include:
- Certain types of kidney and thyroid tissues
- Some benign bone conditions
- Other malignancies, such as renal cell carcinoma
Knowing these patterns is key to correctly reading PSMA PET scans.
Technical and Interpretive Challenges
Technical and interpretive challenges also affect PSMA PET imaging. Things like image resolution, radiotracer uptake time, and reader experience can change how accurate scans are.
Also, differences in scanner technology and image algorithms can make scans hard to compare. Healthcare providers need to know these technical aspects when reading PSMA PET scans.
To tackle these issues, standardized protocols for getting and reading images are being made. Also, keeping radiologists and nuclear medicine doctors up-to-date is important. This helps make PSMA PET imaging more accurate and reliable.
Current Guidelines and Implementation at Leading Institutions
The world of PSMA PET imaging is always changing. Current guidelines come from the top professional societies. These rules help make sure patients get the best care.
Professional Society Recommendations
Groups like the Society of Nuclear Medicine and Molecular Imaging (SNMMI) are key in setting guidelines. They use the newest research and evidence.
Some important points from these groups include:
- PSMA PET imaging is recommended for initial staging in high-risk prostate cancer patients.
- It’s also used to find biochemical recurrence in patients with rising PSA levels.
- It helps plan treatment and check how well it’s working.
LivHospital’s Approach to PSMA PET Imaging
LivHospital follows the guidelines from professional societies for PSMA PET imaging. This ensures patients get the latest in care. The hospital’s nuclear medicine team works with doctors to make PSMA PET fit each patient’s needs.
At LivHospital, PSMA PET imaging is used in many ways, such as:
- For initial diagnosis and staging of prostate cancer.
- To find biochemical recurrence.
- To check how well the treatment is working.
Liv Hospital stays up-to-date with guidelines and uses its team’s knowledge. This puts them at the top in prostate cancer care, giving patients the best results.
Conclusion: The Future of PSMA PET in Prostate Cancer Management
PSMA PET imaging is changing how we diagnose and manage prostate cancer. It accurately finds cancer cells. This helps doctors plan treatments and track how the disease grows.
The future of PSMA PET looks bright. More research and better radiotracers will make it even more useful. Hospitals like Liv Hospital are already using it to help patients more.
PSMA PET is a key tool in fighting prostate cancer. It will keep being important as it becomes part of regular care. This will help patients live better lives.
FAQ
What does PSMA uptake mean in PET imaging?
PSMA uptake in PET imaging shows how much a radioactive tracer is absorbed by cells with Prostate-Specific Membrane Antigen (PSMA). This is often seen in prostate cancer cells. The amount and pattern of uptake can tell us about the cancer’s presence, size, and how aggressive it is.
How is PSMA PET imaging used in prostate cancer diagnosis?
PSMA PET imaging helps find prostate cancer when other methods don’t work. It shows where the main tumor is, how far the disease has spread, and if it has come back.
What are the different types of PSMA radiotracers used in PET imaging?
There are several PSMA radiotracers for PET imaging, like Gallium-68 PSMA-11 and Fluorine-18 PSMA-1007. These tracers stick to PSMA on prostate cancer cells, making tumors visible.
How do I prepare for a PSMA PET scan?
To prepare for a PSMA PET scan, you’ll need to drink water, avoid certain medicines, and possibly empty your bladder or bowel. Your healthcare provider or the imaging center will give you specific instructions.
What are the advantages of PSMA PET imaging over conventional imaging methods?
PSMA PET imaging is better at finding prostate cancer, even when it’s not easily seen by other methods. It helps get a more accurate picture of the disease, which can change treatment plans.
Can PSMA PET imaging have false positives?
Yes, PSMA PET imaging can show false positives. This can happen if PSMA is found in non-cancerous conditions or other cancers. There can also be technical issues that lead to incorrect results.
How is PSMA PET imaging used in treatment planning?
PSMA PET imaging helps plan treatments by showing how far the disease has spread. It helps decide if surgery, radiation, or systemic therapy is best for the patient.
What is the role of LivHospital in PSMA PET imaging?
LivHospital follows the latest guidelines for PSMA PET imaging. This ensures patients get top-notch diagnostic services and care.
What does a high SUV value mean in PSMA PET imaging?
A high SUV value in PSMA PET imaging means the cancer cells are taking up a lot of the tracer. This usually means the cancer is more aggressive or larger.
Are there any limitations to PSMA PET imaging?
While PSMA PET imaging is very accurate, it’s not perfect. It can show false positives and has technical challenges like image quality and tracer availability.
References
- Fendler, W. P., et al. (2023). PSMA PET/CT: joint EANM procedure guideline/SNMMI procedure standard for prostate cancer imaging 2.0. European Journal of Nuclear Medicine and Molecular Imaging, 50(10), 1-30. https://pubmed.ncbi.nlm.nih.gov/36619738/








