The endometrium is a thin, soft layer inside the uterus. Its thickness changes during the menstrual cycle. After menstruation, it’s about 3-4 mm thick. It grows to 8-12 mm near ovulation what does thickened endometrium mean.
A thickened endometrium is known as endometrial hyperplasia. It’s when the uterine lining gets too thick. Knowing about this is key for your reproductive health. At Liv Hospital, we offer top-notch care that puts patients first.
Key Takeaways
- The endometrium’s thickness changes throughout the menstrual cycle.
- A thickened endometrium can be a sign of an underlying condition.
- Understanding endometrial hyperplasia is essential for reproductive health.
- Liv Hospital offers complete care for endometrial issues.
- Early evaluation and diagnosis are critical for effective treatment.
Understanding the Endometrium and Its Normal Function
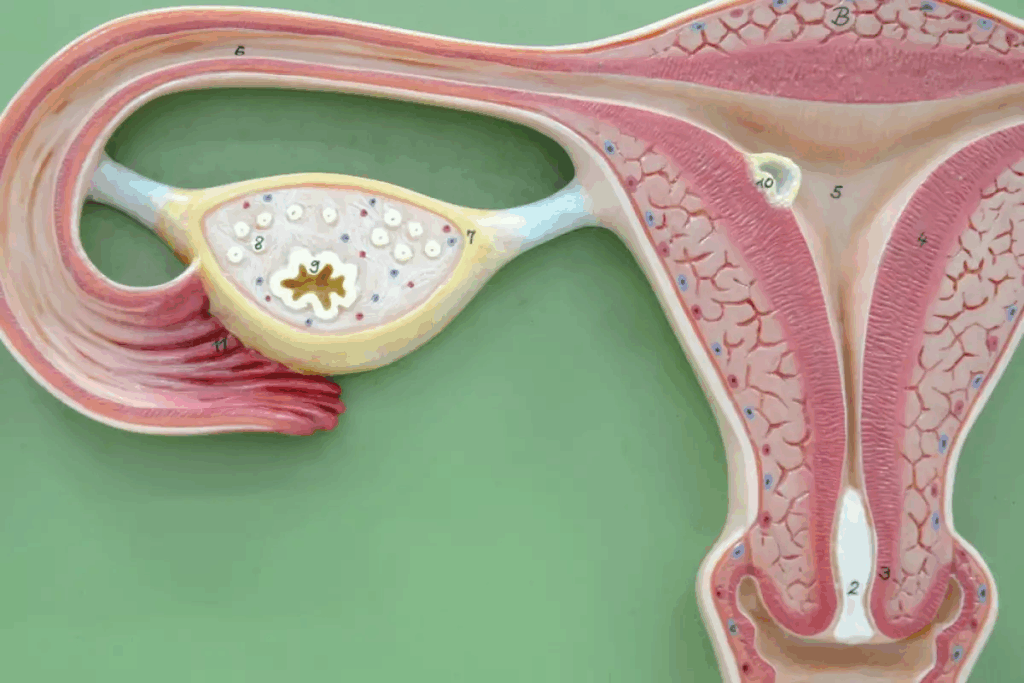
To understand a thickened endometrium, we must first know about its normal role. The endometrium, or endometrial lining, is key to reproductive health. It provides nutrients, helps with conception, and protects the fetus during pregnancy.
The endometrium has two layers: the basal and the functional. The basal layer regenerates the functional layer, which sheds during menstruation if there’s no pregnancy. Normally, the endometrium is about 3-4 mm after menstruation. It thickens to 8-12 mm near ovulation, ready for pregnancy.
Structure and Purpose of the Endometrial Lining
The endometrial lining is not just passive; it’s dynamic, changing with hormonal shifts. Its main job is to support a fertilized egg. As “The endometrium is a highly specialized tissue that undergoes proliferation, differentiation, and shedding in each menstrual cycle”, it’s vital for reproduction.
The functional layer grows and thickens with estrogen in the first half of the cycle. After ovulation, progesterone prepares it for implantation. If implantation fails, the drop in progesterone leads to menstruation, shedding the layer.
Normal Endometrial Thickness Throughout the Menstrual Cycle
Endometrial thickness changes throughout the cycle. It’s thinnest after menstruation, about 3-4 mm. As the cycle moves towards ovulation, it thickens to 8-12 mm, perfect for implantation. Knowing these changes helps spot abnormalities like a thickened endometrium.
Checking endometrial thickness is key to understanding health and spotting issues early. As we explore thickened endometrium, knowing its normal function and thickness is essential.
What Does Thickened Endometrium Mean?
A thickened endometrium means the uterine lining is too thick. This can be a sign of a problem and might need a doctor’s check-up. It’s important to find out why it’s thickened and how to treat it.
Definition of Endometrial Hyperplasia
Endometrial hyperplasia happens when the uterine lining grows too much. Endometrial hyperplasia often comes from too much estrogen and not enough progesterone. This imbalance makes the lining grow thicker than it should.
Doctors sort endometrial hyperplasia into types based on cell changes. Simple hyperplasia is less risky, but complex atypical hyperplasia is more serious and can lead to cancer.
Normal vs. Abnormal Endometrial Measurements
The thickness of the endometrium changes during a woman’s cycle. A thickness under 14 millimeters is usually normal. But, if it’s over 5 mm during certain times, it might be a sign of a problem.
Menstrual Cycle Stage | Normal Endometrial Thickness | Abnormal Endometrial Thickness |
Proliferative Phase | Less than 14 mm | More than 14 mm |
Secretory Phase | Less than 16 mm | More than 16 mm |
Post-Menopause | Less than 5 mm | More than 5 mm |
These numbers can change, and what’s normal can vary. It depends on the cycle stage and if you’re post-menopausal.
If the endometrium gets too thick, it’s important to see a doctor. This is true, even if it’s not during the right time of the cycle or after menopause.
Common Causes of Thickened Endometrium
The thickness of the endometrium can be influenced by several factors. These include hormonal changes and certain medical conditions. We will explore these causes in detail to understand how they contribute to endometrial thickening.
Hormonal Imbalances: Estrogen and Progesterone
Hormonal imbalances, such as an excess of estrogen and insufficient progesterone, are key causes. Estrogen promotes the growth of the endometrial lining. Progesterone helps stabilize and prepare it for pregnancy. Without enough progesterone, the endometrium may keep growing, leading to abnormal thickening.
Estrogen dominance can happen for many reasons. These include hormonal changes during the menstrual cycle, obesity, or exposure to external estrogen. This imbalance can cause endometrial hyperplasia, where endometrial cells grow too much.
Medical Conditions Associated with Endometrial Thickening
Several medical conditions are linked to thickened endometrium. These include:
- Polycystic Ovary Syndrome (PCOS): A hormonal disorder that can lead to irregular menstrual cycles and an increased risk of endometrial thickening.
- Endometrial Polyps: Growths in the endometrial lining that can cause thickening and irregular bleeding.
- Adenomyosis: A condition where endometrial tissue grows into the uterine wall, leading to thickening and other symptoms.
These conditions show why it’s important to diagnose and manage the causes of thickened endometrium. This helps prevent complications and eases symptoms.
Risk Factors for Developing Thickened Endometrium
Several factors can increase the chance of having a thickened endometrium. These include age and overall health. Knowing these risk factors helps identify who might be at higher risk. It also guides the use of preventive measures.
Age-Related Factors
Age is a big factor in thickened endometrium. Women near menopause or in perimenopause face a higher risk. Women over 40 are more likely to have a thickened endometrium because of hormonal changes.
Health Conditions and Lifestyle Factors
Some health conditions and lifestyle choices can raise the risk of thickened endometrium. For example:
- Obesity: Too much body fat can increase estrogen levels, causing the endometrium to thicken.
- Diabetes: Women with diabetes are at higher risk due to metabolic and hormonal imbalances.
- Lifestyle Factors: A sedentary lifestyle and certain diets can also increase the risk.
Keeping a healthy lifestyle is key to reducing the risk of thickened endometrium.
Medications and Hormonal Therapies
Certain medications and hormonal therapies can also raise the risk. Long-term use of estrogen-only hormone replacement therapy (HRT) is a known risk factor. It can lead to unopposed estrogen stimulation of the endometrium. Tamoxifen, used in breast cancer treatment, can also cause endometrial thickening.
Women, and those with risk factors, should be aware of these causes. They should talk to their healthcare provider about their individual risk.
Signs and Symptoms of Thickened Endometrium
Thickened endometrium can show through various symptoms. Women should know these signs to get medical help quickly. We’ll list the common symptoms and when to see a doctor.
Common Symptoms to Watch For
Women with thickened endometrium might have irregular periods, heavy bleeding, and pelvic pain. These symptoms can affect daily life a lot.
Irregular menstrual bleeding is common. Women might bleed between periods or have irregular cycles. Heavy or prolonged menstrual bleeding can cause discomfort and anemia from too much blood loss.
Pelvic pain is another symptom. It can be mild or severe. This pain might be constant or happen at certain times, like during menstruation or sex.
When to Seek Medical Attention
Women should see a doctor if they have persistent or severe pelvic pain, heavy or long bleeding, or irregular bleeding for many cycles.
It’s important to get checked if symptoms don’t go away or get worse. Early check-ups can find the cause and suggest treatments.
- Experiencing persistent or severe pelvic pain
- Heavy or prolonged menstrual bleeding
- Irregular menstrual cycles or bleeding between periods
We advise women to be proactive about their health. If symptoms worry you, get medical help. Early action can greatly improve your health and life quality.
Diagnosis and Evaluation Process
Diagnosing a thickened endometrium involves several steps. These include physical exams, imaging tests, and lab work. We know these steps can make you anxious. So, we’re here to guide you through each one with care and clarity.
Initial Assessment and Physical Examination
The first step is an initial assessment. This includes a detailed medical history and a physical exam. We ask about your symptoms, menstrual cycle, and any health issues. A pelvic exam is also done to check your reproductive organs.
Imaging Tests and Procedures
Imaging tests are key in diagnosing a thickened endometrium. The main test used is transvaginal ultrasound. It lets us measure the endometrium’s thickness. This test is done by inserting an ultrasound probe into the vagina to get clear images of the uterus.
In some cases, more tests like saline infusion sonography (SIS) or hysteroscopy might be needed. These help us look at the uterine cavity more closely.
Biopsy and Laboratory Analysis
An endometrial biopsy might be needed for a clear diagnosis. This involves taking a sample of endometrial tissue for lab tests. The biopsy can spot abnormal cell changes, like hyperplasia or cancer.
Lab tests on the biopsy sample are vital. They help find out if there are any endometrial problems.
Diagnostic Procedure | Purpose | Key Findings |
Transvaginal Ultrasound | Measure endometrial thickness | Thickness measurement, uterine abnormalities |
Endometrial Biopsy | Assess cellular abnormalities | Presence of hyperplasia, cancer, or other cellular changes |
Saline Infusion Sonography (SIS) | Evaluate uterine cavity | Polyps, structural abnormalities |
Treatment Options for Thickened Endometrium
There are many ways to treat thickened endometrium, each one fitting the person’s needs. The right treatment depends on why the endometrium is thick, the person’s age, and their goals for having children.
Hormonal Therapies
Hormonal treatments help balance estrogen and progesterone levels. Progestin therapy is a common choice. It can be taken by mouth or through an intrauterine device (IUD). This helps reduce the endometrium’s thickness by balancing estrogen’s effects.
The table below shows the hormonal therapies used:
Therapy Type | Administration Method | Effect on Endometrium |
Progestin Therapy | Oral or IUD | Reduces thickness by counteracting estrogen |
Estrogen-Progestin Therapy | Oral | Regulates menstrual cycle and reduces thickness |
Surgical Interventions
Sometimes, surgery is needed to treat thickened endometrium. Dilation and Curettage (D&C) removes the uterus lining. It helps diagnose and treat thickening causes.
Other surgical options include:
- Endometrial Ablation: Destroys the endometrial lining to stop thickening.
- Hysterectomy: Removes the uterus, often when there’s a cancer risk.
Lifestyle Modifications and Alternative Approaches
Changing your lifestyle can also help manage thickened endometrium. Eating well, staying active, and keeping a healthy weight can balance hormones and prevent thickening.
Some alternative methods include:
- Dietary Changes: Eating more fruits, vegetables, and whole grains.
- Stress Management: Yoga and meditation can help manage stress and balance hormones.
Potential Complications and Long-Term Health Implications
Thickened endometrium can cause serious health problems if not treated. We will look at the risks, including its link to endometrial cancer and its effects on reproductive health.
Connection to Endometrial Cancer
One big worry with thickened endometrium is its link to endometrial cancer. Research shows that untreated endometrial hyperplasia can raise cancer risk in the endometrium. Regular monitoring and proper treatment are key to lowering this risk.
Factors that increase endometrial cancer risk include too much estrogen without enough progesterone. This can cause uncontrolled cell growth in the endometrium. Women with thickened endometrium should talk to their healthcare provider about these risks.
Impact on Reproductive Health and Fertility
Thickened endometrium can also harm reproductive health and fertility. It can make it harder for women to get pregnant. Hormonal imbalances from thickened endometrium can also mess up ovulation and menstrual cycles.
For women trying to get pregnant, managing thickened endometrium is critical. Treatment might include hormonal therapies to balance estrogen and progesterone. This can help create a better environment for embryo implantation.
We suggest women with thickened endometrium talk to a healthcare provider. They can discuss individual risks and create a treatment plan. By tackling the condition early, women can lower their risk of long-term health issues.
Conclusion: Managing Endometrial Health and When to Consult a Doctor
Knowing about thickened endometrium helps women act fast and get the right medical help. It’s key to keep the endometrium healthy by watching for signs and getting medical advice when needed.
It’s vital to manage endometrial health to avoid serious problems and keep reproductive health in check. If symptoms don’t go away or get worse, seeing a doctor is essential.
Being informed about reproductive health and taking care of ourselves can lower the risk of health problems. Regular health checks and screenings are important for keeping reproductive health in top shape.
FAQ
What is the normal thickness of the endometrium?
The endometrium’s thickness changes throughout the month. It’s usually 8-12 mm during the first part of the cycle. Then, it grows to 12-16 mm in the second part.
What does a thickened endometrium mean?
A thickened endometrium means the uterus lining is too thick. This can happen due to hormonal issues, endometrial hyperplasia, or other health problems.
What causes the endometrium to thicken?
Hormonal imbalances, like too much estrogen, can make the endometrium thick. Other reasons include PCOS, being overweight, and some medicines or therapies.
Is a thickened endometrium a sign of cancer?
A thick endometrium might raise cancer risk, but it’s not a sure sign. Many women with thick endometrium don’t have cancer. A biopsy is needed for a true diagnosis.
How is a thickened endometrium diagnosed?
Doctors use physical exams, ultrasound, and biopsies to find a thick endometrium.
What are the treatment options for a thickened endometrium?
Treatments vary based on the cause. They might include hormones, surgery, or lifestyle changes.
Can a thickened endometrium affect fertility?
Yes, it can. A thick endometrium might make it hard for an embryo to implant or increase miscarriage risk.
How can I manage endometrial health?
Keep a healthy weight, manage stress, and see your doctor regularly. Knowing the signs of a thick endometrium and getting help when needed is key.
What is the relationship between estrogen and endometrial thickness?
Estrogen can make the endometrium grow, leading to thickness. An imbalance with progesterone can cause hyperplasia.
Can certain medications cause a thickened endometrium?
Yes, some medicines, like tamoxifen, and hormonal therapies can make the endometrium thick.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560693/



































