Last Updated on December 3, 2025 by Bilal Hasdemir

Every year, millions of people worldwide get life-saving blood transfusions for different medical issues, like cancer. We count on donors to give the blood needed for these treatments. A clear and simple medical definition answering the fundamental question: What is a blood transfusion?
A blood transfusion, sometimes referred to as a blood infusion, is when a patient gets donated blood or blood parts. This is key for those getting cancer treatment, surgery, or dealing with blood problems.
Key Takeaways
- Blood transfusions are a life-saving medical procedure used to treat various medical conditions.
- Donated blood or blood components are used to replace lost or damaged blood.
- Blood transfusions are critical for patients getting cancer treatment or surgery.
- The procedure involves putting blood or blood parts into a patient’s bloodstream.
- Blood transfusions need careful matching of blood types to ensure compatibility.
Understanding Blood Transfusions
When someone’s body doesn’t have enough blood or certain blood parts, a transfusion might be needed. Blood transfusions are key in treating many health issues. These include anemia, cancer, and blood loss during surgery.
Definition and Purpose
A blood transfusion is when blood or blood parts from a donor are given to a patient. It’s done to replace or add to a patient’s blood or specific parts of it.
There are many reasons someone might need a blood transfusion. These include:
- Replacing blood lost during surgery or injury
- Treating certain health conditions like anemia or cancer
- Increasing red blood cells, platelets, or clotting factors in the blood
We use blood transfusions to help patients recover from many medical issues. By understanding why and how blood transfusions work, patients can see their importance in their care.
How Blood Transfusions Work
The blood transfusion process starts with checking the patient’s blood type. This is to make sure the donated blood is compatible. This step is key to avoid any bad reactions.
| Blood Component | Purpose | Common Use |
| Red Blood Cells | Carries oxygen throughout the body | Treating anemia, blood loss |
| Platelets | Essential for blood clotting | Preventing or treating bleeding |
| Plasma | Contains clotting factors and proteins | Treatments for clotting disorders, burns |
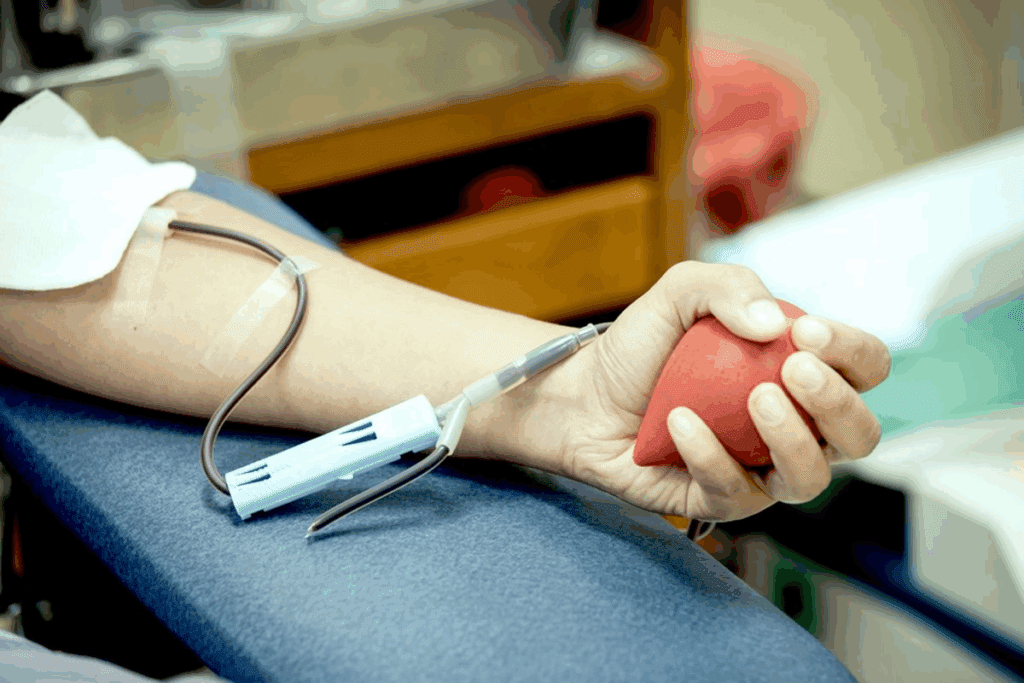
After checking compatibility, the transfusion is given through an IV. This usually happens in a hospital or clinic. Our medical team watches the patient closely during and after the transfusion to make sure it’s safe and works well.
The Process of Blood Donation
Blood donation is a detailed process with many steps. It starts with screening the donor and ends with storing the blood. We make sure each step is done right to keep the blood safe and good quality.
Types of Blood Donations
Blood donations can be split into two main types: whole blood and component donations. Whole blood donations collect all blood parts, like red cells, plasma, and platelets. Component donations focus on specific parts, like platelets or plasma, using apheresis.
Each donation type has its own use. Whole blood is often used in surgeries. Component donations are key for patients needing specific blood parts, like those with cancer.
Safety Measures in Blood Donation
Keeping donors and recipients safe is our top priority. We use strict safety steps, like thorough donor screening, to lower disease risk. Donors are checked for health history, travel, and lifestyle to keep the blood safe.
After blood is collected, it’s tested for diseases like HIV, hepatitis, and malaria. This testing is vital to ensure the blood is safe for transfusions. We also follow strict rules for storing and handling blood to keep it quality and safe.
Learning about blood donation and safety shows us the effort and care in providing safe blood for medical needs.
Why Oncology Patients May Need Transfusions
Oncology patients might need blood transfusions because of cancer and its treatments. These can mess with the body’s blood-making abilities. This can lead to complications that might need transfusions.
Common Reasons for Transfusions in Cancer Care
Oncology patients may need blood transfusions for a few reasons. Anemia is a big one. It happens when treatments like chemotherapy and radiation hurt the bone marrow’s red blood cell making.
Some cancers, like those in the bone marrow, can also mess with blood cell production. Transfusions can help with symptoms like tiredness, weakness, and shortness of breath. This makes life better for the patient.
| Reason for Transfusion | Description | Benefit of Transfusion |
| Anemia | Low red blood cell count due to chemotherapy or radiation | Increased energy levels, reduced fatigue |
| Thrombocytopenia | Low platelet count, increasing the risk of bleeding | Reduced risk of bleeding, faster recovery |
| Neutropenia | Low white blood cell count, increasing the risk of infection | Enhanced immune response, reduced infection risk |
Impact of Cancer Treatments on Blood Levels
Cancer treatments, like chemotherapy and radiation, really affect blood cell making. They target fast-growing cells, which includes cancer and blood-making cells in the bone marrow.
The effect on blood levels depends on the cancer type, treatment, and how the patient reacts. It’s key to keep an eye on these effects to give the best care.
- Chemotherapy can cause a decrease in blood cell counts.
- Radiation therapy, when aimed at the pelvis or spine, can harm bone marrow.
- Some targeted therapies may also impact blood cell production.
Understanding why blood transfusions are needed in cancer care helps doctors help patients more. It improves treatment results and quality of life.
Types of Blood Products Used
Blood transfusions use different blood products for various needs. The right product depends on the patient’s health and the treatment they need. This can include their medical condition, surgery type, or health issues.
Red Blood Cells
Red blood cells (RBCs) are often transfused. They help carry oxygen to tissues and organs. This is key for patients with anemia or blood loss, or those undergoing surgery.
Platelets
Platelets are vital for blood clotting. They are given to patients with low platelet counts or clotting problems. This is common in cancer patients due to chemotherapy’s effects on platelets.
Plasma
Plasma carries proteins and clotting factors. It’s used for patients with clotting issues or significant blood loss. Plasma helps maintain blood balance and clotting.
The table below shows the main uses of different blood products:
| Blood Product | Primary Use |
| Red Blood Cells | Treats anemia, improves oxygen delivery |
| Platelets | Manages bleeding, treats thrombocytopenia |
| Plasma | Restores clotting factors, treats clotting disorders |
Knowing about blood products and their uses is key for patient care. Healthcare providers can choose the right product for each patient. This helps improve their health outcomes.
Signs a Patient May Need a Blood Transfusion
It’s important to know when a patient might need a blood transfusion. This is because it can save lives, mainly for those with cancer or who have lost a lot of blood.
Symptoms Indicating Low Blood Counts
Low blood counts can show up in different ways. Here are some common signs:
- Fatigue and weakness: Not having enough red blood cells makes it hard to do simple things.
- Shortness of breath: When your body doesn’t get enough oxygen, you might feel out of breath even when sitting.
- Dizziness and lightheadedness: Low blood pressure can make you feel like you’re going to fall over.
- Pale skin: Not enough red blood cells can make your skin look pale or tired.
These symptoms can really affect how well a patient feels. It’s key to watch for them to see if a transfusion is needed.
Monitoring and Assessment Procedures
We use several ways to figure out if a blood transfusion is needed. Here are a few:
- Complete Blood Count (CBC): A CBC checks the different parts of your blood, like red and white cells and platelets.
- Regular check-ups: Keeping an eye on how patients are doing and their blood counts helps us spot when they might need a transfusion.
- Symptom assessment: We check how patients are feeling and tell their doctor if anything seems off.
By watching blood counts and symptoms closely, we can tell when a transfusion is needed. This helps support their treatment and improves their health.
Risk Factors for Oncology Patients
Oncology patients face many risks because of their cancer and treatment. These risks can harm their health and affect their treatment plans. They can come from the cancer itself or the treatments used to fight it.
Specific Risks Associated with Cancer
Cancer can cause many complications that raise the risk for oncology patients. For example, cancer-related anemia is a common issue. It can greatly affect a patient’s life quality and how well they respond to treatment.
Other risks include:
- Infections due to weakened immune system
- Bleeding problems from low platelet counts
- Organ damage from cancer or treatment side effects
How Risk Factors Affect Treatment Decisions
Risk factors can greatly shape treatment choices for oncology patients. For instance, a patient at high risk of bleeding might need platelet transfusions to prevent serious bleeding. Patients with anemia might get red blood cell transfusions to help their oxygen levels and ease symptoms.
A leading oncologist says, “Knowing the risks linked to cancer and treatment is key for making smart patient care decisions.” Treatment plans are often customized to manage these risks. This ensures patients get the best and most effective care possible.
“Managing risk factors in oncology patients needs a team effort. It involves oncologists, nurses, and other healthcare experts to give full care.”
– Expert in Oncology
The Benefits of Blood Transfusions
Blood transfusions provide vital blood components to manage cancer complications. They improve patients’ quality of life and help their treatment responses. This is a big help for those fighting cancer.
Improvements in Quality of Life
Blood transfusions can greatly improve patients’ lives. They help with symptoms like fatigue, shortness of breath, and dizziness. These symptoms often come from low blood counts.
Transfusions boost red blood cell counts. This ensures tissues and organs get the oxygen they need. It helps them work better.
Transfusions also significantly reduce the risk of bleeding. This makes patients feel safer and more stable. It improves their mental and emotional health, helping them cope better with their condition.
Supporting Treatment Responses
Blood transfusions also support treatment responses. They keep blood cell counts healthy. This lets patients keep up with their treatments without breaks.
This is very important for cancer patients. Uninterrupted treatment is key to the best results.
The following table highlights some key benefits of blood transfusions for oncology Page Page patients:
| Benefit | Description | Impact on Patients |
| Improved Oxygen Delivery | Enhanced red blood cell count | Reduced fatigue and shortness of Page breath |
| Reduced Risk of Bleeding | Platelet Page transfusions | Minimized risk of hemorrhage and related complications |
| Support for Treatment | Maintenance of healthy blood cell counts | Uninterrupted treatment and improved outcomes |
Blood transfusions have many benefits. They can significantly improve patients’ quality of life and treatment outcomes. Healthcare providers can better support cancer patients with these benefits in mind.
Potential Risks and Side Effects
It’s important to know the risks of blood transfusions for patient care. Blood transfusions are key in medical treatment, but they can have complications.
Common Side Effects of Transfusions
Blood transfusions can cause side effects, from mild to severe. Some common reactions include:
- Febrile non-hemolytic reactions: These are marked by fever and chills. They are usually treated with medicine.
- Allergic reactions: Symptoms can be hives and itching. Antihistamines are often used to treat them.
- Transfusion-related acute lung injury (TRALI): This is a severe reaction that can lead to breathing problems.
These side effects show why it’s key to watch patients closely during and after transfusions.
Managing Risks Effectively
We use several ways to lower the risks of blood transfusions:
- Careful donor screening: We make sure donated blood is safe and matches the recipient’s blood type.
- Advanced testing techniques: We use the latest tech to find infectious agents in blood donations.
- Personalized patient care: We customize transfusion plans for each patient, based on their health history and current state.
By using these methods, we can greatly reduce the risks of blood transfusions. This ensures patients get the best care possible.
Alternatives to Blood Transfusions
Oncology patients have many options instead of blood transfusions. These choices depend on their health and needs. They can help avoid some risks of blood transfusions and improve health outcomes.
Options Available for Oncology Patients
There are several alternatives for oncology patients needing blood transfusions. These include:
- Medications that stimulate blood production: Erythropoiesis-stimulating agents (ESAs) can boost red blood cell production. This reduces the need for transfusions.
- Iron supplements: Iron supplements can help patients with iron deficiency anemia. They improve red blood cell counts.
- Growth factors: Certain growth factors can help produce more platelets and white blood cells. This supports patients going through chemotherapy.
When Alternatives May Be Appropriate
Choosing alternatives to blood transfusions depends on several factors. These include the patient’s health, the type and stage of cancer, and the treatments they’re getting.
For example, ESAs are used for patients with anemia caused by chemotherapy. But, their use must be carefully thought about. This is because they can increase the risk of blood clots.
We carefully look at each patient’s situation to find the best alternative to blood transfusions. This personalized approach makes sure patients get the safest and most effective treatment for their needs.
Post-Transfusion Care
We know that care after a blood transfusion is key. It’s about the patient’s recovery and feeling good. We watch for any bad reactions or complications. This ensures the patient’s safety and the treatment’s success.
Monitoring After a Transfusion
Patients are watched closely after a transfusion. Vital signs like temperature, blood pressure, and heart rate are checked often. This makes sure the patient is doing well.
We also check the patient’s overall health. This includes looking for bleeding or bruising. We make sure the blood components are working right.
Signs of Complications to Watch For
Blood transfusions are usually safe, but complications can happen. It’s important to spot these signs early for quick action.
Some complications to watch for include:
- Fever or chills
- Shortness of breath or trouble breathing
- Rash or itching
- Swelling or pain at the transfusion site
- Dizziness or fainting
| Signs to Watch For | Possible Complications | Action to Take |
| Fever, chills | Transfusion reaction | Notify healthcare provider immediately |
| Shortness of breath | Transfusion-related acute lung injury (TRALI) | Seek medical attention right away |
| Rash, itching | Allergic reaction | Inform healthcare team; may require medication |
Knowing what to look for and acting fast helps patients get the best care after a transfusion.
The Role of Healthcare Providers
Healthcare providers are key in caring for patients getting blood transfusions. We teach patients about the process and its effects. This makes sure they know what to expect and are ready.
Collaborative Care
Oncologists and nurses are essential in managing blood transfusions. Our team works together to give full care. Oncologists plan the treatment, and nurses provide direct care and support.
Educating Patients
Teaching patients is a big part of our job. We tell them about the good and bad sides of blood transfusions. We also teach them to watch for any problems.
This way, patients can help decide their treatment. Together, we aim to give the best care. This improves their life and treatment results.
FAQ
What is a blood transfusion?
A blood transfusion is when donated blood is given to a patient. It’s used to replace or add to their own blood.
Why do oncology patients need blood transfusions?
Oncology patients might need blood transfusions because of cancer treatments. These treatments can lower blood counts, leading to anemia or low platelets.
What are the signs that indicate a need for a blood transfusion?
Signs that might mean a patient needs a blood transfusion include fatigue and shortness of breath. Dizziness, pale skin, and easy bruising or bleeding are also signs.
What types of blood products are used in transfusions?
Transfusions use red blood cells, platelets, and plasma. Each type helps in different ways, like improving oxygen delivery or supporting clotting.
How is blood donation processed and ensured safe for transfusion?
Blood donation is tested for diseases and checked for compatibility. This ensures the blood is safe and matches the recipient’s blood type.
What are the benefits of blood transfusions for oncology patients?
Blood transfusions can greatly improve the lives of oncology patients. They help alleviate symptoms of anemia and support treatment, leading to better overall well-being.
Are there any risks or side effects associated with blood transfusions?
While rare, blood transfusions can have risks like allergic reactions or iron overload. These are managed with careful monitoring and patient care.
Are there alternatives to blood transfusions available for oncology patients?
Yes, there are alternatives like erythropoiesis-stimulating agents (ESAs) for anemia. Medications to boost platelet production are also options, depending on the patient’s condition and treatment plan.
How is post-transfusion care managed?
After a transfusion, patients are watched for complications. They are also taught what to look for and report to their healthcare providers.
What role do healthcare providers play in managing blood transfusions?
Healthcare providers, like oncologists and nurses, are key in managing blood transfusions. They assess the need, administer the transfusions, monitor responses, and educate patients.
Can a person have multiple blood transfusions?
Yes, a person can have multiple blood transfusions. The need and frequency depend on their medical condition and treatment plan, decided by healthcare providers.
What is the difference between infusion and transfusion?
An infusion is when medications or fluids are given into the bloodstream. A transfusion, on the other hand, involves giving blood or blood components to replace or supplement a patient’s own blood.
How are patients monitored during and after a blood transfusion?
Patients are closely watched during and after a transfusion for any adverse reactions. Their vital signs are checked regularly. They are also taught to watch for signs of complications after they go home.
National Institutes of Health. Evidence-Based Medical Insight. Retrieved from https://www.nhlbi.nih.gov/health/blood-bone-marrow-treatments
References
World Health Organization. Evidence-Based Medical Insight. Retrieved from https://www.who.int/news-room/fact-sheets/detail/blood-transfusion-safety





