Knowing the normal aortic valve gradient and aortic stenosis severity classification is key for good treatment plans. At Liv Hospital, we follow global standards and the newest echocardiographic methods. This helps us accurately grade and tailor care for each patient.
A normal aortic valve gradient is usually when the mean gradient is under 10 mmHg and the peak is under 20 mmHg. We use these echocardiographic numbers to figure out and classify aortic stenosis severity. This ensures our patients get the best care possible.
Key Takeaways
- Normal aortic valve gradient is characterized by a mean gradient
- Aortic stenosis severity is classified using echocardiographic measurements.
- Liv Hospital follows international standards for accurate grading and patient care.
- Echocardiographic techniques are key for diagnosing aortic stenosis.
- Good treatment decisions depend on knowing aortic stenosis severity.
Understanding the Aortic Valve and Its Function
It’s key to know how the aortic valve works to spot and fix heart problems. This valve is vital for blood to move right from the heart to the body.
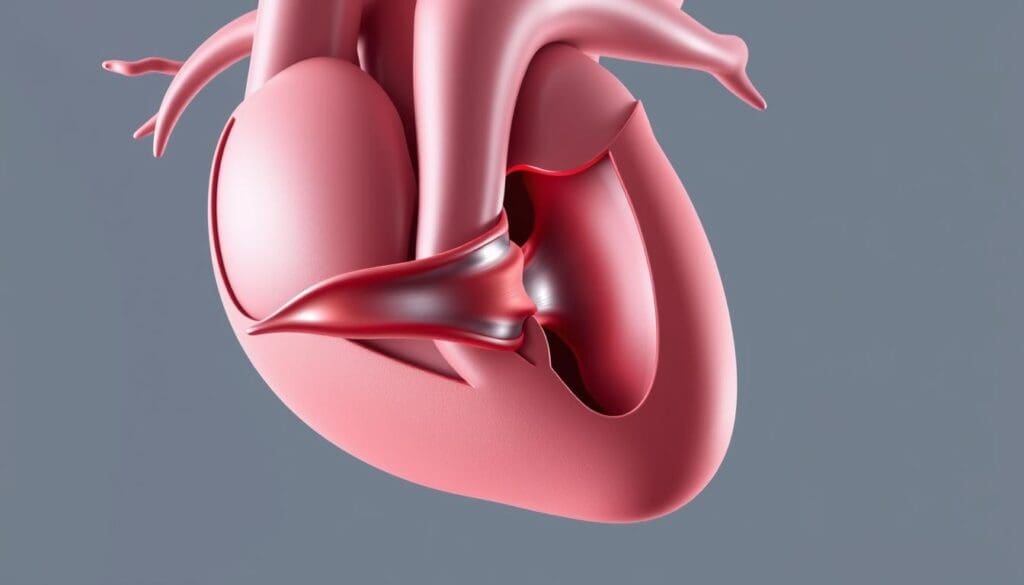
Anatomy of the Aortic Valve
The aortic valve sits between the left ventricle and the aorta. It has three cusps that open and close to control blood flow. The normal aortic valve area is about 3.0 to 4.0 cm, helping blood flow well during heart contraction.
The valve’s design stops blood from flowing back into the left ventricle when the heart relaxes.
Normal Blood Flow Through the Aortic Valve
When the left ventricle contracts, it pushes blood through the aortic valve into the aorta. The valve opens wide, letting blood flow easily. Good valve function means blood flows only one way, from the heart to the body.
This flow is key for keeping blood pressure right and organs well-fed.
Importance of Proper Valve Function
A healthy aortic valve is essential for heart health. Problems like stenosis or regurgitation can cause serious issues, like heart failure. Keeping the aortic valve working right is vital for the heart’s best performance.
We’ll look at what happens when the aortic valve doesn’t work right next.
What Is a Normal Aortic Valve Gradient?
Knowing the normal gradient of the aortic valve is key for diagnosing and treating heart issues. The aortic valve gradient shows the pressure difference between the left ventricle and the aorta during heart contraction. It helps doctors understand how severe aortic stenosis is.
Definition of Valve Gradient
The valve gradient is the pressure difference across the aortic valve. It’s measured with Doppler echocardiography, showing peak and mean gradients. The peak gradient is the highest pressure difference during heart contraction. The mean gradient is the average pressure difference during that time.
Normal aortic valve function has a low gradient, meaning little to no blockage of blood flow. Any big change from normal gradient values could mean the valve is not working right.
Normal Mean Gradient Values
A normal mean gradient across the aortic valve is less than 10 mmHg. This shows the valve is working well and there’s no big stenosis. A mean gradient under 10 mmHg means the valve area is normal and blood flow is not blocked much.
Normal Peak Gradient Values
The normal peak gradient across the aortic valve is below 20 mmHg. This is the standard to tell if the valve is working right or if there’s stenosis. If the peak gradient is over 20 mmHg, it might mean aortic stenosis needs to be checked further.
To wrap up, knowing the normal aortic valve gradient values is very important for doctors. Here’s a quick table of these values:
| Gradient Type | Normal Value |
|---|---|
| Mean Gradient | Less than 10 mmHg |
| Peak Gradient | Below 20 mmHg |
A top cardiologist says, “Knowing the normal and abnormal gradients of the aortic valve is key for diagnosing and treating aortic stenosis.” This shows how critical it is to measure gradients accurately in medical practice.
“Checking the aortic valve gradient is vital for diagnosing and treating aortic stenosis. It helps doctors make important decisions.”
Understanding Aortic Stenosis
To understand aortic stenosis, we need to know its causes and risk factors. This condition happens when the aortic valve opening gets smaller. This can cause serious heart problems.
Pathophysiology of Aortic Valve Stenosis
Aortic stenosis occurs when the aortic valve opening is less than half its normal size. This blocks blood flow from the left ventricle to the aorta. It can happen due to different reasons that affect the valve’s structure and function.
The pathophysiology involves complex interactions between the valve leaflets, annulus, and surrounding cardiac structures. As the stenosis gets worse, it puts more pressure on the left ventricle. This can cause the ventricle to grow thick and not work well.
Common Causes of Aortic Stenosis
Several factors can lead to aortic stenosis. The main causes are:
- Calcification of the aortic valve leaflets, which is common in older adults
- Congenital abnormalities, like a bicuspid aortic valve
- Rheumatic fever, which can scar and fuse the valve leaflets
These causes make the valve orifice narrower, leading to aortic stenosis.
Risk Factors for Developing Aortic Stenosis
Some risk factors increase the chance of getting aortic stenosis. These include:
- Being older, as calcific aortic stenosis is more common in older people
- Having a bicuspid aortic valve or other congenital heart defects
- Having had rheumatic fever
- Having high cholesterol and high blood pressure, which can lead to valve calcification
Knowing these risk factors is key to catching aortic stenosis early and treating it.
Understanding aortic stenosis’s causes, risk factors, and pathophysiology helps doctors diagnose and treat it better. This improves patient outcomes.
Key Measurements in Aortic Stenosis Assessment
Assessing aortic stenosis involves looking at several important factors. Getting these right is key to choosing the right treatment.
Peak Velocity Measurement
Measuring the peak velocity across the aortic valve is a key step. Doppler echocardiography helps find the highest blood flow speed. Higher speeds mean more severe stenosis. A speed over 4 m/s usually shows severe stenosis.
Mean Pressure Gradient
The mean pressure gradient is another vital measurement. It shows the average pressure difference between the left ventricle and the aorta. This is found by adding up the pressure differences over time. A higher gradient means more severe stenosis. A gradient of 40 mmHg or more is usually severe.
Aortic Valve Area (AVA) Calculation
The aortic valve area calculation is important for measuring the valve’s size. The continuity equation is used to find this area. A smaller area means more severe stenosis. An area under 1 cm is usually severe.
Dimensionless Index
The dimensionless index, or velocity ratio, compares blood flow speeds. This index is useful because it’s less affected by flow conditions. A ratio under 0.25 usually shows severe stenosis.
These measurements work together to give a full picture of aortic stenosis. They help doctors make the best treatment plans.
Aortic Stenosis Severity Classification
It’s key to accurately classify aortic stenosis severity to ensure the right treatment. We use specific echocardiographic criteria for this. These criteria help us decide the best course of action for each patient.
Mild Aortic Stenosis Criteria
Mild aortic stenosis is marked by a peak velocity of 2.0-2.9 m/s and a mean gradient under 20 mmHg. These patients usually don’t need immediate treatment but should be watched closely.
Moderate Aortic Stenosis Criteria
Moderate aortic stenosis shows a peak velocity of 3.0-3.9 m/s and a mean gradient of 20-39 mmHg. We keep a close eye on these patients for any signs of worsening. We then decide if they need any interventions.
Severe Aortic Stenosis Criteria
Severe aortic stenosis is when the peak velocity is over 4.0 m/s and the mean gradient is more than 40 mmHg. Patients with severe aortic stenosis often need surgery or a catheter procedure to improve their health.
Here’s a quick summary of aortic stenosis severity levels:
- Mild: Peak velocity 2.0-2.9 m/s, mean gradient
- Moderate: Peak velocity 3.0-3.9 m/s, mean gradient 20-39 mmHg
- Severe: Peak velocity > 4.0 m/s, mean gradient > 40 mmHg
Knowing these criteria helps us make better decisions for our patients. By accurately classifying aortic stenosis, we can tailor care to meet each patient’s unique needs.
Echocardiographic Assessment of Aortic Stenosis
We use echocardiography to check aortic stenosis. This method is non-invasive and gives us important details about the valve. It helps us understand the valve’s structure and how it works.
Doppler Echocardiography Techniques
Doppler echocardiography is key in checking aortic stenosis. It lets us see how fast blood flows through the valve. This is important for knowing how severe the stenosis is.
We use the Doppler principle to find the peak velocity and mean pressure gradient. The peak velocity is the highest speed of blood flow. The mean pressure gradient is found by looking at the velocity over time.
2D and 3D Echocardiography
Two-dimensional (2D) echocardiography gives us clear images of the valve. We can see the shape of the valve, any calcification, and how well it opens. It also helps us measure the left ventricular outflow tract (LVOT) diameter.
Three-dimensional (3D) echocardiography gives us a better view of the valve. It lets us measure the valve area directly. This is helpful when the valve is heavily calcified or irregular.
Transesophageal Echocardiography
Transesophageal echocardiography (TEE) gives us detailed images from the esophagus. It’s great for looking at the valve’s shape and function. TEE is better when TTE images aren’t clear enough.
TEE helps us see how severe the stenosis is. It also helps decide if certain treatments are right. It gives us more information to help us understand the patient’s situation.
The Continuity Equation in AVA Calculation
The continuity equation is key in finding the aortic valve area (AVA). It helps us see how severe aortic stenosis is.
This equation is based on the idea that blood flow doesn’t change as it moves from the left ventricle to the aorta. It’s vital for figuring out the AVA. This is important for diagnosing and treating aortic stenosis.
Understanding the Continuity Equation
The continuity equation is simple: AVA = (LVOT area x LVOT VTI) / AV VTI. VTI stands for velocity time integral. It lets us compare blood flow in the left ventricle to the aorta.
Step-by-Step Calculation Process
To use the continuity equation, we do the following:
- Measure the LVOT diameter to find its area.
- Get the LVOT VTI with pulsed-wave Doppler.
- Measure the AV VTI with continuous-wave Doppler.
- Then, we calculate the AVA using the equation.
Potential Sources of Error
Even though the continuity equation is useful, there are errors to watch out for:
- Wrong measurement of the LVOT diameter.
- Be careful with Doppler beam alignment.
- Look out for big calcifications in the valve or below it.
By knowing and using the continuity equation right, we can get accurate AVA values. This is key for figuring out how bad aortic stenosis is and making treatment plans.
Factors Affecting Aortic Valve Gradient Measurements
Many factors can change how we measure aortic valve gradients. This is important for diagnosing and treating aortic stenosis. Knowing these factors helps us make accurate assessments and treatments.
Operator Technique and Experience
The skill and experience of the person doing the echocardiogram matter a lot. Getting the Doppler beam right is key to getting accurate peak velocity measurements. If it’s not aligned right, the gradient might seem lower than it really is.
How well the Doppler signal is captured also depends on the operator. Adjusting gain settings and wall filters can improve the quality of the Doppler signal. More experienced operators know how to make these adjustments better.
Patient Flow States (Low Flow, Low Gradient)
When patients have low flow, low gradient conditions, it’s harder to tell how severe aortic stenosis is. Low flow states happen when the heart doesn’t pump as much blood as it should. This can make the measured gradient seem lower than it really is.
| Flow State | Characteristics | Impact on Gradient Measurement |
|---|---|---|
| Normal Flow | Normal cardiac output | Accurate gradient measurement |
| Low Flow | Reduced cardiac output | Potential underestimation of gradient |
| Low Gradient | Reduced pressure gradient across the valve | May not accurately reflect stenosis severity |
Technical Limitations and Challenges
There are technical issues that can affect how well we measure aortic valve gradients. Poor acoustic windows can make it hard to get clear images. This makes it tough to get accurate measurements.
Also, calcification and reverberation artifacts can mess with the Doppler signal. This can lead to wrong velocity measurements. It’s important to know about these technical challenges to understand the results correctly.
Special Considerations in Aortic Stenosis Assessment
In aortic stenosis, some conditions need extra attention. They affect how we diagnose and treat the disease. Understanding these complexities helps us give the best care.
Low-Flow, Low-Gradient Aortic Stenosis
Low-flow, low-gradient aortic stenosis is a tough case. It has a small valve area and a low pressure gradient. Getting it right is key for treatment and results.
We use echocardiography and other tests to check the valve and heart. It’s important to look closely at the patient’s blood flow to figure out the stenosis level.
Paradoxical Low-Flow Aortic Stenosis
Paradoxical low-flow aortic stenosis is another tricky case. Patients seem to have a normal heart function but have low flow. Advanced imaging is needed to diagnose and manage them.
Aortic Stenosis with Preserved Ejection Fraction
Aortic stenosis with preserved ejection fraction is when patients have stenosis but their heart looks fine. We use echocardiography and other checks to assess the stenosis.
Knowing about these special cases is key to better care for aortic stenosis patients. By understanding the challenges of each, we can improve treatment plans and outcomes.
Clinical Implications of Aortic Stenosis Severity
Knowing how aortic stenosis severity affects patients is key to good care. The severity of the condition impacts symptoms, how fast it gets worse, and when to intervene.
Symptom Correlation with Stenosis Severity
The severity of aortic stenosis is tied to symptoms. Mild cases might not show symptoms, but severe cases can really affect a person’s life. Symptoms like chest pain, shortness of breath, and fainting are more common in severe cases.
Progression Rates and Monitoring Intervals
Aortic stenosis gets worse at different rates for everyone. People with mild stenosis usually need less frequent checks. But those with moderate or severe stenosis need more regular checks to see how the disease is progressing.
- Regular echocardiograms are key for tracking the disease.
- How often to check depends on the stenosis severity.
- It’s also important to watch symptoms to decide when to intervene.
Indications for Intervention Based on Severity
Deciding to intervene depends on the stenosis severity and symptoms. Severe aortic stenosis, with symptoms, is a clear sign to act. This might mean surgery or a new valve, based on the patient’s health and other factors.
Understanding aortic stenosis severity helps doctors give better care. Regular checks and timely action are essential for managing the condition well.
Advanced Imaging Techniques for Aortic Stenosis
Advanced imaging is key in diagnosing and managing aortic stenosis. These methods give doctors important details. They help figure out how severe the condition is and guide treatment plans. We’ll look at cardiac CT, cardiac MRI, and new technologies for checking aortic stenosis.
Cardiac CT for Valve Assessment
Cardiac CT is a top choice for checking aortic stenosis. It shows the aortic valve’s details, like how much calcium is there. This helps doctors know how bad the stenosis is. It also helps plan for TAVR by measuring the aortic annulus exactly.
Cardiac MRI Applications
Cardiac MRI gives a full view of the aortic valve and nearby areas. It measures how severe the stenosis is and checks the heart’s function. It also looks for heart muscle damage, which is important for predicting the future.
Emerging Technologies in Valve Assessment
New tech like 4D flow MRI and advanced modeling are changing how we check aortic stenosis. They give detailed info on blood flow and let doctors test different treatments. This could lead to better results for patients.
Conclusion
Accurate assessment and management of aortic stenosis are key to better patient outcomes. We’ve covered the importance of aortic stenosis assessment. This includes echocardiographic measurements and advanced imaging techniques.
Knowing the normal aortic valve gradient is vital. It helps in diagnosing and classifying aortic stenosis severity. This knowledge allows healthcare providers to tailor treatment plans for each patient.
In summary, a detailed aortic stenosis assessment is essential for quality patient care. By focusing on accurate diagnosis and management, we can enhance outcomes for those with this condition.
What is a normal aortic valve gradient?
A normal aortic valve gradient is less than 10 mmHg on average. The peak should be below 20 mmHg. This shows the valve is working well and not blocking blood flow.
How is aortic stenosis severity classified?
Aortic stenosis severity is measured by echocardiography. It looks at peak velocity, mean pressure gradient, and aortic valve area (AVA). Based on these, it’s classified as mild, moderate, or severe.
What are the criteria for severe aortic stenosis?
Severe aortic stenosis is when the peak velocity is 4 m/s or more. The mean gradient should be 40 mmHg or higher. An AVA of 1 cm² or less also indicates severe obstruction.
What is the continuity equation used for in aortic stenosis assessment?
The continuity equation helps calculate the aortic valve area (AVA). It considers the flow through the valve and blood velocity. This is key in assessing aortic stenosis severity.
How does low-flow, low-gradient aortic stenosis differ from other forms of aortic stenosis?
Low-flow, low-gradient aortic stenosis has low cardiac output and a mean gradient under 40 mmHg. Despite severe stenosis, it needs special management.
What is the role of echocardiography in diagnosing aortic stenosis?
Echocardiography, including Doppler and 2D/3D techniques, is essential in diagnosing aortic stenosis. It provides vital info on valve function and blood flow.
How do advanced imaging techniques contribute to aortic stenosis assessment?
Advanced imaging like cardiac CT and MRI offer more details on valve anatomy and calcium burden. They help in planning treatments and assessing overall risk.
What are the clinical implications of aortic stenosis severity?
The severity of aortic stenosis impacts symptoms, progression, and treatment needs. Accurate classification is critical for effective management.
How is the dimensionless index used in aortic stenosis assessment?
The dimensionless index compares blood flow velocities through the aortic valve. It helps assess stenosis severity, useful in certain cases.
What factors can affect the accuracy of aortic valve gradient measurements?
Factors like operator technique and patient flow states can impact gradient measurements. It’s important to consider these when interpreting echocardiographic data.
References
- Dr. Oracle AI (What is a Normal Gradient for an Aortic Valve) : https://www.droracle.ai/articles/127284/what-is-a-normal-gradient-for-an-aortic-valve
- Cardioserv (Echo: Top Factors to Consider Evaluating AS) : https://www.cardioserv.net/echo-top-factors-to-consider-evaluating-as
- PMC – PubMed Central : https://pmc.ncbi.nlm.nih.gov/articles/PMC8503314
- ESC (European Society of Cardiology) E-Journal of Cardiology Practice (Aortic valve stenosis evaluation) : https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-15/Aortic-valve-stenosis-evaluation-and-management-of-patients-with-discordant-grading
- Heart Valve Surgery (Echocardiogram: Aortic Stenosis & Regurgitation Diagnosis) : https://www.heartvalvesurgery.com/echocardiogram-aortic-stenosis-regurgitation-diagnosis.php