Last Updated on November 20, 2025 by Ugurkan Demir
At Liv Hospital, we know how complex sickle cell disease is. It’s a genetic disorder that messes with hemoglobin production. This makes red blood cells stiff and take on a sickle shape.
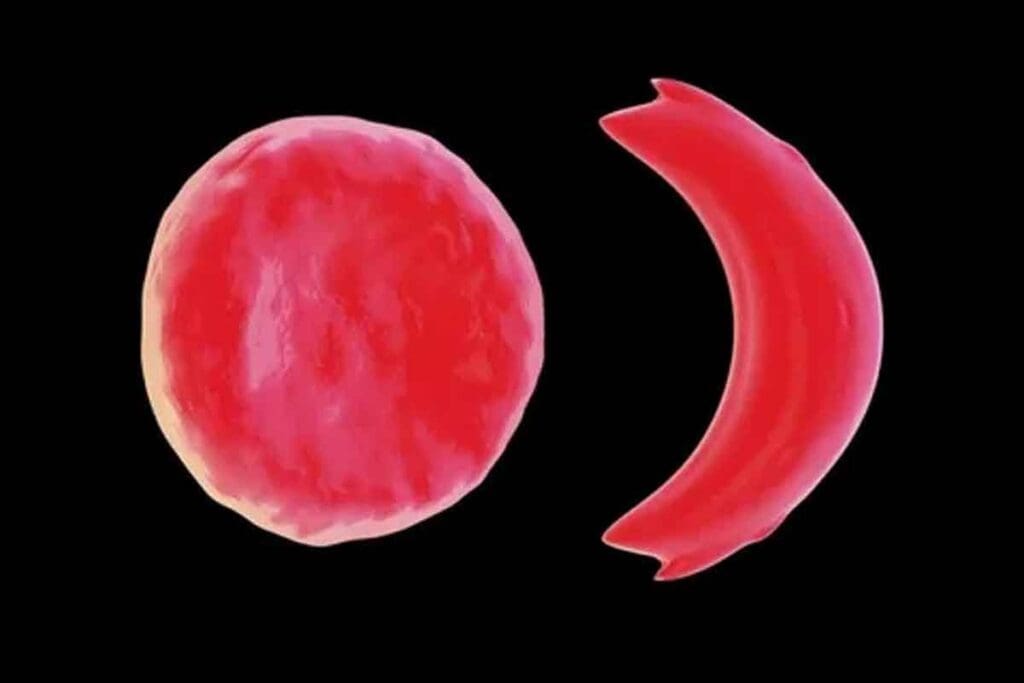
Normally, red blood cells are round and can bend easily. But for people with SCD, the abnormal hemoglobin makes them sickle-shaped. This shape causes blockages in blood flow. It also leads to pain and damage to organs.
The a Medical organization says this shape change comes from a genetic mutation. It affects how hemoglobin is made. We understand how important it is to know this to give our patients the best care.
Key Takeaways
- Sickle cell disease is a genetic disorder affecting hemoglobin production.
- The disease causes red blood cells to become rigid and assume a sickle shape.
- Sickle-shaped cells can lead to blockages in blood flow, causing pain and organ damage.
- Understanding SCD is key for giving top-notch care.
- Liv Hospital is dedicated to providing world-class healthcare for international patients.
What Is a Sickle: From Agricultural Tool to Medical Terminology

The word ‘sickle’ comes from an old tool used for farming. It had a curved shape. Now, it’s used in medicine too. This change shows how our understanding of a common condition has grown.
The Historical Origins and Design of the Sickle Tool
The sickle tool has been around for ages. It was made to cut grain and other crops. Its curved shape helped farmers work more efficiently. This design has stayed the same over time.
The Metaphorical Transition to Medical Science
In medicine, “sickle” means the odd shape of red blood cells in Sickle Cell Disease (SCD). These cells look like crescents or half-moons because of a genetic change. This shape makes it hard for these cells to work right, causing health problems. The term “sickle” moving from farming to medicine shows how words can change in science.
Knowing where the term “sickle” comes from helps us understand SCD better. It shows how a term from farming can describe a complex medical issue well.
The Genetic Foundation of Sickle Cell Disease
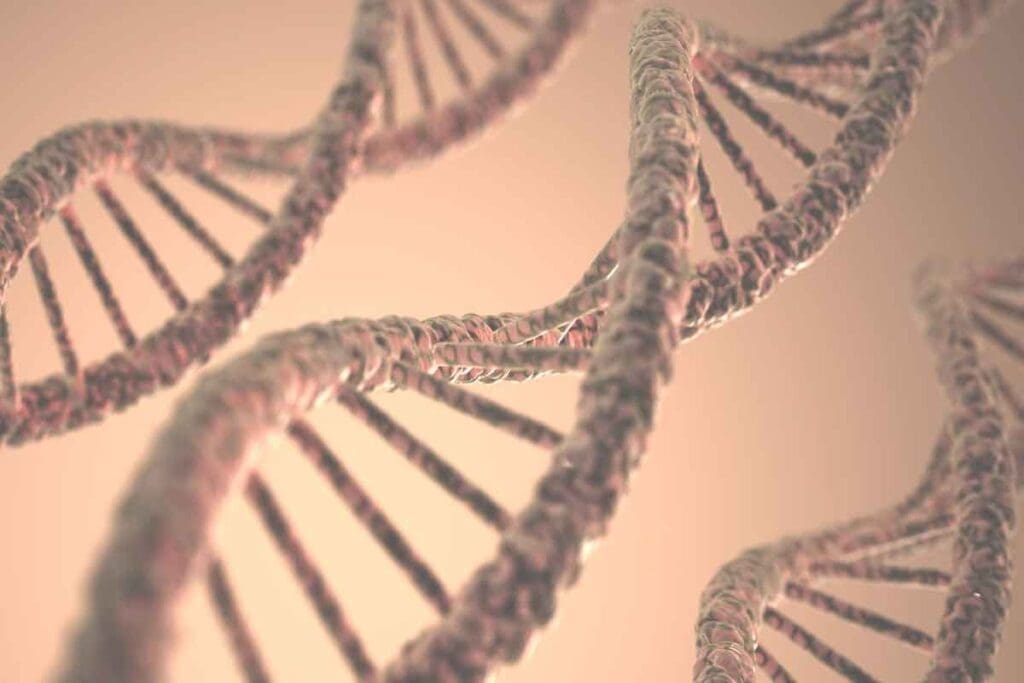
Sickle Cell Disease is caused by a mutation in the HBB gene. This gene is key for making the beta-globin subunit of hemoglobin. The mutation leads to abnormal hemoglobin, known as hemoglobin S (HbS).
The HBB gene tells our bodies how to make the beta-globin subunit of hemoglobin. This protein is in red blood cells and carries oxygen. When the gene mutates, it makes HbS. This can cause red blood cells to bend into a sickle shape.
Understanding the HBB Gene Mutation
The mutation in the HBB gene changes glutamic acid to valine at the sixth position of the beta-globin chain. This change makes hemoglobin prone to polymerization under low oxygen. The polymerization of HbS causes red blood cells to sickle.
Genetic testing can show if someone has this mutation. It helps find carriers and those affected. Knowing the genetic basis of SCD is key for finding new treatments and tests.
Patterns of Inheritance and Genetic Variations
Sickle Cell Disease follows an autosomal recessive pattern. This means you need two mutated HBB genes to have the disease. Carriers have one normal and one mutated gene. They usually don’t show symptoms but can pass the mutated gene to their kids.
Genetic variations can change how SCD shows up. For example, having other hemoglobinopathies like beta-thalassemia can affect the disease’s symptoms. Knowing these variations helps predict how the disease will be and how to manage it.
The Transformation of Red Blood Cells: Normal vs. Sickle-Shaped
It’s important to know the difference between normal and sickle-shaped red blood cells. These cells carry oxygen all over our body. Their shape and flexibility help them move through tiny blood vessels.
Structure and Function of Healthy Red Blood Cells
Normal red blood cells are flexible and shaped like a donut. This shape lets them move well through blood vessels. They can change shape to fit different conditions in the body.
These cells are full of hemoglobin, a protein that carries oxygen. Their shape helps them exchange gases well. This is key for delivering oxygen and removing carbon dioxide.
How Hemoglobin S Alters Cell Structure
In Sickle Cell Disease, a genetic change makes hemoglobin S. When oxygen is low, hemoglobin S sticks together. This makes the red blood cell stiff and sickle-shaped.
This change is permanent. Sickled cells can’t change back. They are more likely to break down and can’t move through narrow places.
Environmental and Physiological Triggers of Sickling
Many things can make red blood cells sickle. Low oxygen, dehydration, and acidosis are examples. When oxygen is low, hemoglobin S sticks together more easily.
Dehydration also makes sickling more likely. It increases the amount of hemoglobin S in cells. Knowing what triggers sickling is key to managing SCD. Avoiding these triggers can help reduce sickling crises and improve life quality.
The Domino Effect: How Sickle Shape Disrupts Blood Circulation
The sickle shape of red blood cells causes many problems. In people with sickle cell disease (SCD), these cells are stiff and stick together. This leads to many issues with blood flow.
Rigidity and Adhesion Properties of Sickle Blood Cells
Sickle-shaped red blood cells are very stiff. This is because of the way hemoglobin S works. They find it hard to move through small blood vessels, causing vascular obstructions.
Also, these cells stick to the walls of blood vessels. This makes blockages worse.
- Increased rigidity due to hemoglobin S polymerization
- Enhanced adhesion to endothelial cells
- Resulting vascular obstructions and reduced blood flow
Vascular Blockages and Resulting Tissue Damage
The stiffness and sticking of sickle blood cells lead to vascular blockages. These blockages stop blood from flowing right. This causes tissues to not get enough oxygen, leading to damage.
This damage can cause pain, harm organs, and lead to other problems related to SCD.
- Vascular blockages cause tissue ischemia
- Ischemia leads to tissue damage and pain crises
- Repeated episodes result in chronic organ damage
It’s important to understand how sickle-shaped red blood cells affect blood flow. This knowledge helps doctors find better ways to treat SCD. By focusing on the causes of blockages and damage, doctors can help patients feel better.
Acute Manifestations of Sickle Cell Disease
SCD has many acute effects, like pain crises, chronic anemia, and a higher risk of infections. These issues can really affect how well patients live, so they need good care plans.
Pain Crises: Mechanisms and Management
Pain crises, or vaso-occlusive crises, are key signs of SCD. They happen when sickled red blood cells block blood vessels, causing pain. This pain is very severe and often leads to hospital stays.
- Triggers: Things like infections, not drinking enough water, cold weather, and stress can start pain crises.
- Management: To manage, patients need to drink lots of water, take pain medicines (like opioids for bad pain), and fix what’s causing the pain.
Chronic Anemia and Its Daily Impact
Chronic anemia is a big problem in SCD because red blood cells die early. This makes people tired, weak, and short of breath. It affects daily life and how well they feel.
To help with chronic anemia, doctors might:
- Give blood transfusions to add healthy red blood cells.
- Prescribe medicines like hydroxyurea to lessen pain crises and maybe help anemia.
Compromised Immunity and Infection Risk
People with SCD are more likely to get sick because their spleen doesn’t work well and their immune system is off. They often get infections like pneumonia, meningitis, and bone infections.
To lower this risk, we suggest:
- Using antibiotics to prevent infections, mainly in kids.
- Keeping vaccinations current, like for pneumococcal, meningococcal, and flu.
- Seeing a doctor right away if they think they have an infection.
Understanding and tackling these issues can really help improve life for SCD patients.
Long-Term Health Complications Caused by Cell Sickling
SCD can lead to many long-term health issues. The sickling and unsickling of red blood cells cause damage. This damage affects many parts of the body.
Multi-Organ Damage and Dysfunction
The sickling of red blood cells can harm organs like the spleen, kidneys, and liver. The spleen is often damaged because of sickled red blood cells. This can lead to the spleen not working.
Kidney damage happens when sickled red blood cells block the kidneys. This makes it hard for the kidneys to work right. It can even lead to chronic kidney disease.
The liver can also be affected. Sickled red blood cells in the liver can cause damage. This can lead to liver problems and scarring.
This damage to organs can really affect a person’s life. It can make everyday activities hard.
Developmental Delays and Growth Issues
Children with SCD might have trouble growing and developing. The anemia from SCD doesn’t give enough oxygen to growing tissues. This can slow down growth.
Pain and hospital stays can also slow down a child’s development. They might miss out on school and other important activities.
Ocular and Neurological Complications
SCD can cause eye problems, like sickle retinopathy. This can lead to vision loss. Sickled red blood cells in the eyes can cause damage.
Neurological problems, like stroke, are also a big worry. Sickled red blood cells can block blood flow in the brain. This can cause a stroke.
Children with SCD are at a higher risk of stroke. It’s important to watch them closely and take steps to prevent it.
In summary, SCD can cause many serious health problems. These problems can greatly affect a person’s life. It’s important to get good care and watch for these issues closely.
Global Distribution and Demographics of Sickle Cell Disease
Sickle Cell Disease (SCD) is found worldwide, shaped by genetics, geography, and demographics. It’s a big health problem in many places, mainly where the sickle cell gene is common.
SCD isn’t just a problem for certain groups. It affects people all over, with different areas having more cases. This is due to history, genetics, and health care access.
High Prevalence Regions: Africa and the Middle East
Africa and the Middle East have the most SCD cases. Here, it’s a big health issue because of poor health care and genetics.
These areas have much higher SCD rates than the world average. In some African countries, up to 30% of people carry the sickle cell trait.
| Region | Prevalence of Sickle Cell Trait | Estimated Number of SCD Births Annually |
| Sub-Saharan Africa | 10%-30% | 230,000 |
| Middle East | 5%-15% | 20,000 |
| Indian Subcontinent | 5%-10% | 50,000 |
Sickle Cell Disease in the Indian Subcontinent
The Indian subcontinent also struggles with SCD. Its prevalence varies, with some areas having more cases due to genetics and tribal populations.
This region faces a unique challenge because of its genetic diversity. Managing SCD here needs a specific approach.
Prevalence and Patterns in the United States
In the U.S., SCD mostly affects people of African descent. But it can also be found in others. About 100,000 people in the U.S. have SCD.
Newborn screening programs help find SCD early. This allows for early treatment and care. The U.S. needs to keep working on public health and awareness.
Breakthrough Advances in Sickle Cell Disease Management
Recent years have seen big changes in how we manage Sickle Cell Disease (SCD). These changes are making a big difference in the lives of those affected. New ways of diagnosing and treating SCD are being introduced, thanks to new technologies and ideas.
Impact of Newborn Screening Programs
Newborn screening programs have been key in catching SCD early. They help start treatments early, which can greatly improve health outcomes.
Early diagnosis through newborn screening leads to better care. It helps avoid serious problems and improves life quality for kids with SCD.
| Benefits of Newborn Screening | Outcomes |
| Early Diagnosis | Timely Medical Intervention |
| Preventive Measures | Reduced Risk of Complications |
| Parental Education | Better Disease Management |
Current Standard Treatment Protocols
Today’s treatments for SCD aim to manage symptoms and prevent problems. They include:
- Hydroxyurea therapy to reduce pain crises
- Blood transfusions to lower hemoglobin S levels
- Strategies for managing pain, like medicine and other therapies
Revolutionary Gene Therapies and Future Directions
Gene therapy is a new hope for SCD treatment. It aims to fix the genetic issue causing the disease. Advances in gene editing, like CRISPR/Cas9, are making this possible.
We are on the verge of a new era in SCD treatment. Gene therapies could change how we treat the disease. Research and trials are key to making these new treatments available to patients.
| Gene Therapy Approaches | Potential Benefits |
| Gene Editing (CRISPR/Cas9) | Potential Cure |
| Gene Expression Modification | Reduced Severity of Symptoms |
| Lentiviral Vector-based Therapies | Stable Correction of Genetic Defect |
Liv Hospital’s Multidisciplinary Approach to Sickle Cell Disease
Liv Hospital is dedicated to fighting Sickle Cell Disease. We use a team effort that combines the latest treatments with learning. Our goal is to meet the full needs of SCD patients.
Innovative Treatment Protocols and Academic Integration
At Liv Hospital, we create new treatment plans based on the latest research. Our team works with experts worldwide. This ensures our treatments are top-notch and follow global standards.
Key Components of Our Treatment Protocols:
- Personalized treatment plans tailored to each patient’s genetic profile and medical history
- Advanced pharmacological interventions, including the latest medications and therapies
- State-of-the-art transfusion therapy and management
We also join in research studies and clinical trials. This means our patients get the newest treatments.
Patient-Centered Care and Ethical Commitments
Our care focuses on the patient. We know SCD impacts not just the person but their family and community too. So, we offer care that covers physical, emotional, and social needs.
| Aspect of Care | Description |
| Comprehensive Support | Multidisciplinary teams providing medical, psychological, and social support |
| Personalized Care Plans | Tailored plans addressing the unique needs of each patient |
| Family Involvement | Engaging family members in the care process to ensure a supportive environment |
We value honesty, respect for patient choices, and fair, accessible care. We aim to make a caring space for patients. Here, they feel important and supported.
By mixing new treatments with a focus on the patient, Liv Hospital wants to better lives of SCD patients. Our goal is to offer top-notch, caring healthcare.
Conclusion: Reshaping the Future for Sickle Cell Patients
As we learn more about Sickle Cell Disease (SCD), the future looks bright. New research and treatments are on the horizon. These advancements aim to better the lives of those with SCD.
New therapies are being developed to tackle SCD’s core issues. Gene therapies and other innovative treatments are making progress. They hope to enhance the lives of SCD patients.
At Liv Hospital, we’re all about top-notch healthcare for international patients. Our team tackles SCD with a full-on approach. We’re committed to leading the way in SCD care, aiming to make a real difference in patient lives.
FAQ
What is Sickle Cell Disease?
Sickle Cell Disease (SCD) is a genetic disorder. It changes the shape of red blood cells. This makes them sickle-shaped and disrupts blood flow.
What causes Sickle Cell Disease?
SCD is caused by a mutation in the HBB gene. This gene codes for a part of hemoglobin. The mutation leads to abnormal hemoglobin S.
How is Sickle Cell Disease inherited?
SCD is inherited in an autosomal recessive pattern. This means you need two copies of the mutated HBB gene. One from each parent.
What are the symptoms of Sickle Cell Disease?
Symptoms include pain crises and chronic anemia. There’s also a risk of infections and long-term damage to organs. Developmental delays can occur too.
How is Sickle Cell Disease diagnosed?
SCD is diagnosed through newborn screening. A blood test checks for abnormal hemoglobin S.
What are the treatment options for Sickle Cell Disease?
Treatments include pain management and blood transfusions. Medications help reduce pain crises. Gene therapies and new treatments are also being developed.
How does Liv Hospital approach Sickle Cell Disease treatment?
Liv Hospital uses a multidisciplinary approach. They combine innovative treatments, patient-centered care, and academic integration. This provides full support for SCD patients.
What is the global prevalence of Sickle Cell Disease?
SCD is a big public health issue worldwide. It’s most common in Africa, the Middle East, and the Indian subcontinent.
What are the long-term complications of Sickle Cell Disease?
Long-term complications include multi-organ damage and developmental delays. There are also ocular and neurological issues. The risk of infections and other health problems increases.
What is the future of Sickle Cell Disease management?
The future looks promising. Research is ongoing into gene therapies and new treatments. These aim to improve patient outcomes and care for those with SCD.
References
- Chu, E. Y., et al. (2022). Sickle cell disease: a review. JAMA, 328(19), 1979-1994. https://pubmed.ncbi.nlm.nih.gov/35788790/
- Kato, G. J., Piel, F. B., Reid, C., Gaston, M. H., Ohene-Frempong, K., Krishnamurti, L., Smith, W. R., Panepinto, J. A., Weatherall, D. J., Costa, F. F., & Vichinsky, E. P. (2018). Sickle cell disease. Nature Reviews Disease Primers, 4, 18010.https://www.nature.com/articles/nrdp201810





