Nearly 1 in 5 patients who get a stent may face stent blockage a few years later. This shows how important it is to understand this issue. What is a stent blockage? It’s called restenosis. Get best facts. Learn how drug-eluting stents prevent this dangerous issue effectively.
Stent placement is a common way to treat blocked or narrowed arteries. But, the chance of stent blockage is a worry for both patients and doctors. An artery with a stent can block again because of different stent complications.
It’s key to know the risks and causes of stent blockage to manage it well. We’ll look into these to help clear up this important topic.
Key Takeaways
- Stent blockage occurs in nearly 1 in 5 patients within a few years after stent placement.
- An artery with a stent can get blocked again due to various stent complications.
- Understanding the risks of stent blockage is key for managing the condition well.
- Stent placement is a common way to treat blocked or narrowed arteries.
- Factors that lead to stent blockage include the patient’s health and the type of stent.
What is a Stent: Definition and Basic Function

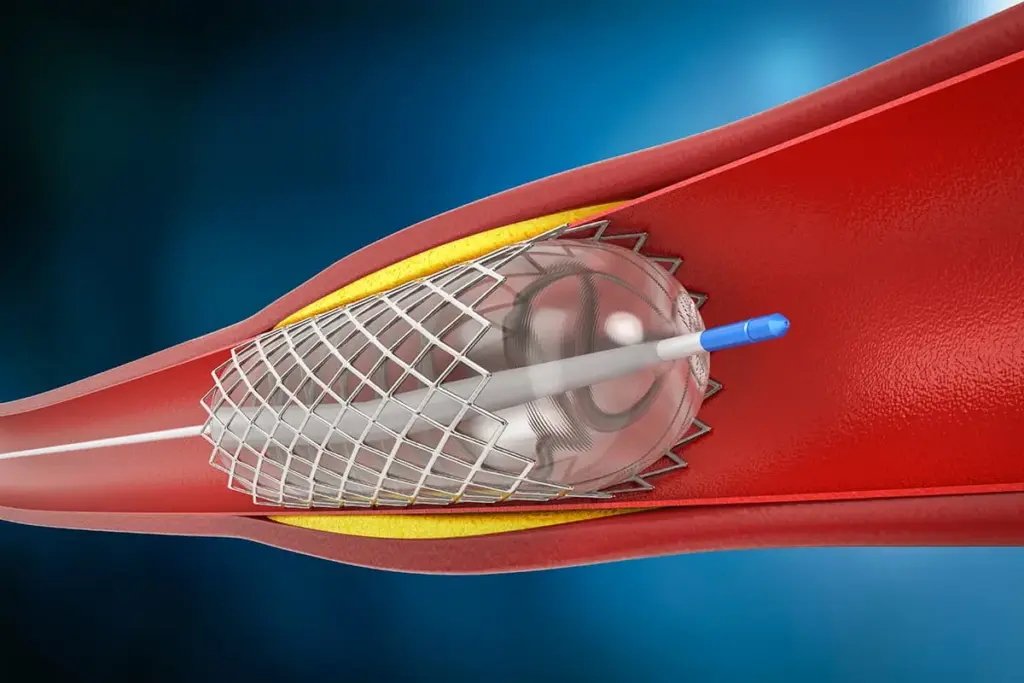
A stent is a medical device that keeps arteries open. This improves blood flow. It’s a small, mesh-like tube used to treat narrowed or blocked arteries.
“Stents have changed how we treat heart disease,” says a leading cardiologist. “They offer a less invasive way to keep arteries open, greatly improving patient results.”
The Structure and Components of Modern Stents
Modern stents are made from materials like stainless steel and cobalt-chromium. These materials are strong and flexible. They can be compressed into a small catheter and then expanded to fit the artery.
Key components of modern stents include:
- Mesh structure for flexibility and strength
- Drug-eluting coatings to prevent restenosis
- Radio-opaque markers for visibility during imaging
How Stents Keep Arteries Open

A stent is placed in an artery through a small catheter. Once in place, it expands, pushing against the plaque. This keeps the artery open.
The stent stays in the artery forever. It supports the artery walls and prevents them from collapsing or becoming blocked again.
Historical Development of Stent Technology
The idea of stenting started in the 1960s. But the first coronary stent was developed in the 1980s. Stent technology has improved a lot, with better materials and coatings.
Stent technology has grown a lot. There’s always research to make stents safer and more effective.
Types of Stents Used in Modern Medicine
Modern medicine uses many types of stents, each with its own features. The right stent depends on the patient’s health, where the blockage is, and the doctor’s advice.
Bare Metal Stents
Bare metal stents are made from metals like stainless steel. They are simple and have been around for a while. But, they can cause tissue growth inside the artery, leading to re-narrowing.
Drug-Eluting Stents
Drug-eluting stents have a special coating that prevents the artery from narrowing again. They slowly release medicine, making them a good choice for those at high risk of re-narrowing.
Bioresorbable Vascular Scaffolds
Bioresorbable vascular scaffolds are a new kind of stent. They gradually dissolve over time. This technology supports the artery while it heals and then disappears, aiming to reduce long-term problems.
Specialized Stents for Different Arteries
Each artery needs a specific stent. For example, coronary artery stents are made to be flexible and strong. There are also stents for other parts of the body, like the legs and arms.
As stent technology improves, we can offer more personalized care. This leads to better health outcomes and a better quality of life for patients.
“The development of new stent technologies is key to better patient care and fewer complications.”
A Cardiologist
Visual Guide: Pictures of Stents for Heart Procedures
Seeing is believing when it comes to stents for heart procedures. Visual aids help us understand how stents work and their role in heart health.
Understanding Stent Appearance and Design
Stents are small, mesh-like tubes used to keep arteries open. They are made from metal or a mix of metal and fabric. Over time, stent design has improved to be more effective and safe.
Modern stents are flexible and strong. They can handle the blood flow and pressure in arteries.
Key Features of Stents:
- Mesh structure for flexibility and support
- Drug-eluting coatings to prevent restenosis
- Biocompatible materials to reduce the risk of adverse reactions
Before and After Images of Stent Placement
Looking at before and after images helps us see the impact of stent placement. These images are taken during angiogram procedures.
An image before stent placement might show a narrowed artery. After the procedure, the artery is fully open, with the stent in place.
How to Interpret Angiogram Images with Stents
Angiogram images are key for seeing inside arteries and checking stent placement. To understand these images, look for the stent as a mesh-like structure in the artery.
Key points to look for in angiogram images:
- The stent’s position within the artery
- The openness of the artery post-stent placement
- Any possible complications, like blood clots or restenosis
Healthcare professionals use these images to check if the stent placement was successful. They also monitor the patient’s progress over time.
The Stent Placement Procedure Explained
The stent placement procedure is a new way to treat heart problems. It’s less invasive than old methods. Knowing about it can make you feel better and more prepared.
Preparation for Stent Surgery
Before the procedure, our team will help you get ready. Here’s what you can expect:
- Detailed medical history and physical examination
- Review of current medications and possible changes
- Diagnostic tests like angiograms or stress tests
- Talk about the procedure’s risks and benefits
- Signing consent forms
Following our instructions is key. This might mean fasting before the procedure and having someone drive you home.
Step-by-Step Stent Insertion Process
The stent placement procedure involves several steps:
- Local anesthesia to numb the area.
- Inserting a catheter through an artery.
- Using imaging to guide the catheter to the blocked artery.
- Angioplasty to open the artery with a balloon.
- Placing the stent to keep the artery open.
- Removing the catheter and closing the site.
Immediate Post-Procedure Care
After the procedure, we watch you closely for any issues. Important post-procedure care includes:
- Resting for several hours to prevent bleeding.
- Monitoring vital signs and the catheter site.
- Medications to prevent clots.
- Slowly returning to normal activities as advised.
Learning about the stent placement procedure can reduce anxiety. Our team is here to support you every step of the way.
Restenosis: When Arteries with Stents Become Blocked Again
After a stent is placed, a big worry is restenosis. This is when the artery gets narrow again. It can bring back symptoms or even worse heart problems. Knowing about restenosis helps set the right expectations after a stent is put in.
The Restenosis Process
Restenosis happens because of the body’s reaction to the stent. The stent can irritate the artery’s lining, causing inflammation. This can lead to new tissue growth inside the stent, blocking it again. It involves complex cell actions, like smooth muscle cell growth.
There are two main types of restenosis: early restenosis and late restenosis. Early restenosis happens soon after the stent is placed. Late restenosis can occur years later. Each type has different causes and risks.
Risk Factors for Stent Blockage
Several things can make restenosis more likely. These include:
- Patient-related factors: Diabetes, high blood pressure, and high cholesterol increase the risk.
- Lesion-related factors: The location, length, and complexity of the treated area matter.
- Stent-related factors: The type of stent used, like bare-metal or drug-eluting, affects the risk.
- Procedural factors: How the stent is placed, like the stent size and inflation pressure, also plays a role.
Statistics on Stent Failure Rates
Stent failure rates depend on many things, like the stent type and patient health. Drug-eluting stents usually have lower restenosis rates than bare-metal stents. But, restenosis is always a possible problem.
Studies show drug-eluting stents have a 5-10% restenosis rate. This can change based on the study and how restenosis is defined. Researchers keep working to make stents better and lower these rates.
In-Stent Thrombosis: Another Form of Stent Blockage
In-stent thrombosis is a serious problem where a blood clot forms inside a stent. This can lead to the stent becoming blocked and cause severe health issues.
Mechanisms of Blood Clot Formation in Stents
The formation of blood clots in stents is complex. It involves the stent material, the patient’s blood, and the artery’s condition. Damage to the artery lining during stent placement can start the clotting process.
The risk of clotting depends on the stent type and how the patient reacts to it. Drug-eluting stents, for example, can slow healing and increase the risk of clotting later on.
Acute vs. Late Stent Thrombosis
Stent thrombosis can happen early or late. Acute stent thrombosis happens within 24 hours due to procedural issues or platelet activation. Late stent thrombosis occurs months or years later, often when antiplatelet therapy is stopped.
|
Characteristics |
Acute Stent Thrombosis |
Late Stent Thrombosis |
|---|---|---|
|
Timing |
Within 24 hours |
Months or years after stent placement |
|
Causes |
Procedural complications, acute platelet activation |
Discontinuation of antiplatelet therapy, delayed healing |
|
Risk Factors |
Incomplete stent apposition, residual dissection |
Resistance to antiplatelet therapy, complex lesions |
Prevention Strategies
To prevent in-stent thrombosis, we need a multi-faceted approach. This includes choosing the right stent, using precise techniques, and following antiplatelet therapy guidelines. Dual antiplatelet therapy (DAPT) is key, mainly in the early stages after stent placement.
Patients must take their medications as prescribed and keep up with follow-up appointments. Knowing the signs and symptoms of stent thrombosis is also important. This way, they can seek medical help quickly if problems arise.
Stent Recovery: What to Expect After Placement
After getting a stent, patients go through a healing process. This process helps them recover well and avoid problems. Knowing what to expect can make things easier.
Hospital Recovery Timeline
The time spent in the hospital after a stent varies. It can be a few hours or a couple of days. This depends on how the patient is doing and how complex the procedure was.
While in the hospital, doctors keep a close eye on the patient. They watch the heart rate, blood pressure, and other important signs. They also look for any signs of trouble.
Important parts of hospital recovery include:
- Watching the heart rate, blood pressure, and other vital signs
- Giving medicines to stop clots and manage pain
- Resting and doing little to let the stent settle
Activity Restrictions and Gradual Return to Normal Life
When patients go home, they need to follow certain rules. They should avoid hard work, heavy lifting, and intense exercise. Slowly, they can start doing more things, based on what their doctor says.
Here are some tips for getting back to normal:
- Start with short walks and then walk more
- Don’t lift heavy or bend a lot
- Wait for the doctor’s okay to start having sex again
Managing Discomfort and Side Effects
After getting a stent, some people feel pain or have side effects. These can include bruising, chest pain, and feeling very tired. It’s important to handle these feelings well to recover comfortably.
Ways to deal with discomfort include:
- Take the medicines as told
- Use cold packs to reduce swelling
- Rest enough to let your body heal
By knowing the recovery process and following the doctor’s advice, patients can get through the time after a stent placement. This helps avoid problems and makes sure the stent works right.
Medications After Stent Placement to Prevent Blockage
Medications are key in managing patients after stent placement. They focus on stopping clots and preventing restenosis. After a stent is put in, there’s a risk of clotting or blockage. Medications help lower this risk.
Dual Antiplatelet Therapy (DAPT)
Dual Antiplatelet Therapy (DAPT) is vital in stopping stent thrombosis. It uses two drugs: aspirin and a P2Y12 inhibitor (like clopidogrel or ticagrelor). DAPT stops platelets from sticking together, which lowers clot risk on the stent.
Using both drugs together is better than one alone in preventing stent thrombosis. The choice of P2Y12 inhibitor and how long to use DAPT depends on the stent type, patient risk, and other factors.
Key Components of DAPT:
- Aspirin: Stops platelet activation by blocking COX-1.
- P2Y12 Inhibitors: Block the P2Y12 receptor on platelets, stopping platelet aggregation.
Statins and Other Medications
Statins are also given to patients after stent placement. They lower cholesterol and reduce inflammation. Both can help prevent restenosis or stent blockage.
Other drugs like beta-blockers, ACE inhibitors, or ARBs might be used. They help manage conditions like high blood pressure or diabetes. These conditions can affect stent success.
|
Medication Class |
Purpose |
Examples |
|---|---|---|
|
Antiplatelet Agents |
Prevent platelet aggregation and clot formation |
Aspirin, Clopidogrel, Prasugrel |
|
Statins |
Lower cholesterol and reduce inflammation |
Atorvastatin, Rosuvastatin, Simvastatin |
|
Beta-blockers |
Reduce heart rate and blood pressure |
Metoprolol, Atenolol, Propranolol |
Duration of Medication Therapy
The length of medication after stent placement varies. It depends on the stent type, patient risk, and guidelines. Usually, DAPT is needed for 6 to 12 months. But it can last longer in some cases.
“The optimal duration of DAPT should be individualized based on the patient’s ischemic and bleeding risks.” –
American Heart Association Guidelines
Statins and other heart medications might be taken for a long time. This depends on the patient’s health and risk factors.
Lifestyle Changes to Maintain Stent Patency
Keeping a healthy lifestyle is key to the success of your stent. After getting a stent, making some lifestyle changes can greatly help. These changes can also improve your heart health.
Dietary Recommendations
Eating a heart-healthy diet is important for keeping your stent open. Eat lots of fruits, vegetables, whole grains, and lean proteins. Try to eat less of foods high in saturated fats, trans fats, and cholesterol.
Nutritional Tips:
- Eat more omega-3 fatty acids from fish like salmon and sardines.
- Choose healthy fats like avocado, nuts, and olive oil.
- Drink less from processed and packaged foods.
Exercise Guidelines After Stent Placement
Regular exercise is key for heart health and keeping your stent open. Start with easy activities like walking. Then, slowly add more intense exercises as your doctor suggests.
Exercise Benefits:
- Boosts heart function.
- Helps manage weight and stress.
- Improves overall health.
Smoking Cessation and Alcohol Moderation
Stopping smoking is a big step for heart health and stent patency. Look into smoking cessation programs and support groups. Also, drink alcohol in moderation, as too much can harm your heart.
Tips for Smoking Cessation:
- Talk to your doctor about quitting aids.
- Join a support group for motivation.
- Avoid things that make you want to smoke.
By making these lifestyle changes, you can greatly improve your stent’s effectiveness. This will also enhance your overall quality of life.
Signs and Symptoms of a Blocked Stent
It’s important for patients with stents to know the warning signs. A blocked stent can cause serious health issues if not treated quickly.
Warning Signs to Watch For
The symptoms of a blocked stent can differ. Here are some key signs to look out for:
- Chest pain or discomfort, feeling like pressure or tightness
- Shortness of breath, even when resting
- Fatigue or feeling unusually tired
- Dizziness or lightheadedness
- Pain or discomfort in the arms, back, neck, jaw, or stomach
Not everyone will show all these symptoms. Some might not show any at all. But if you notice any, it’s important to get medical help.
When to Seek Emergency Care
If you have severe or sudden symptoms, like intense chest pain or trouble breathing, get emergency care right away. These could be signs of a heart attack or other serious issues.
Don’t wait to call emergency services or get someone to drive you to the emergency room if symptoms are severe.
Diagnostic Tests for Stent Evaluation
If you’re showing symptoms of a blocked stent, your doctor might suggest some tests. These include:
- Angiogram: Uses dye and X-rays to see inside the arteries
- Stress test: Checks the heart’s function under stress, often with exercise or medicine
- Cardiac catheterization: Inserts a catheter into an artery to look at the heart and blood vessels
These tests help figure out if the stent is blocked and what treatment is best.
Stent Cards: Why You Need to Carry One
A stent card is more than just a piece of paper. It’s a vital document with important information about your stent. After getting a stent, it’s key to know why this card is so important and why you should always carry it.
Information on a Stent Card
A stent card has vital details about your stent placement. It might list the stent type, the procedure date, and the healthcare provider or institution. Having this info ready can be very helpful in medical emergencies.
Importance in Emergency Situations
In emergencies, a stent card gives doctors quick access to your stent info. This is very important if you can’t talk or if doctors don’t know your full medical history. Your stent card info can guide treatment and ensure you get the right care.
Digital Alternatives to Physical Stent Cards
Now, there are digital stent cards too. Some healthcare providers offer these digital cards for your phone or patient portal. These digital options make it easier to keep your stent info with you.
It doesn’t matter if you have a physical or digital stent card. The important thing is to always have it with you. Talk to your healthcare provider to see what options you have and make sure your card is current.
Complications and Risks Associated with Stents
Stents are usually safe and work well, but problems can happen. It’s key to know these risks. They’ve changed how we treat heart diseases, but patients need to understand the possible issues to make smart choices.
Short-term Complications
Right after a stent is put in, some issues might pop up. These include bleeding where the doctor made the access point, allergic reactions to the dye used, and acute stent thrombosis. This last one is rare but serious and can cause a heart attack or death if not treated fast.
- Bleeding or hematoma at the access site
- Allergic reactions to contrast dye
- Acute stent thrombosis
- Infection at the access site
A study in the Journal of the American College of Cardiology found that acute stent thrombosis is less than 1% with modern stents and the right treatment.
Long-term Risks
Stents can also have long-term issues. These include restenosis, or the artery getting narrow again, and late stent thrombosis. Restenosis is more likely with bare-metal stents than drug-eluting stents, which release medicine to stop cell growth.
|
Type of Stent |
Risk of Restenosis |
Risk of Late Stent Thrombosis |
|---|---|---|
|
Bare-metal Stents |
Higher |
Lower |
|
Drug-eluting Stents |
Lower |
Higher if DAPT is discontinued prematurely |
A well-known cardiologist says, “The main thing is to educate patients and make sure they take their medicine, like DAPT.”
The main thing is to educate patients and make sure they take their medicine, like DAPT.
Balancing Benefits Against Possible Complications
Even with risks, stents often help more than they harm for many people. Deciding to get a stent should be a careful choice, considering your own risks and talking it over with your doctor.
We stress the need for lifestyle changes, sticking to your medication, and keeping up with doctor visits. This helps lower risks and get the most from stent use.
Innovations in Stent Technology to Reduce Reblockage
Stent technology has made big strides, giving hope to those at risk of reblockage. Research and development are pushing the limits of stent design and function. This is aimed at bettering patient results.
Next-Generation Drug-Eluting Stents
New drug-eluting stents (DES) aim to fix old stent problems. They release medicine to stop cell growth, cutting down restenosis risk. Studies show newer DES designs, with better polymers and drug release, lead to better results.
Key Features of Next-Generation DES:
- Enhanced biocompatibility
- Improved drug release mechanisms
- Thinner struts for better deliverability
Biodegradable Stents
Biodegradable stents, or bioresorbable vascular scaffolds (BVS), are a big leap in stent tech. They act as temporary support, then dissolve, leaving a natural artery.
|
Feature |
Biodegradable Stents |
Traditional Metal Stents |
|---|---|---|
|
Material |
Biodegradable polymers or metals |
Permanent metal alloys |
|
Functionality |
Temporary scaffolding, then dissolves |
Permanent scaffolding |
|
Benefits |
Restores natural vessel function, reduces long-term complications |
Well-established efficacy, but with possible long-term issues |
A top cardiologist says, “Biodegradable stents are a big step in treating coronary artery disease. They could lead to better long-term results.”
“The future of stent technology is about meeting patient needs with personalized treatments. This aims to lower risks and increase benefits.”
A Interventional Cardiologist
Nanotechnology Applications in Stent Design
Nanotechnology is being used to make stents better and safer. Nanocoatings can make stents more biocompatible, reduce clotting, and improve drug delivery. These advances are key to creating stents that are both effective and safe for long use.
As we keep pushing stent technology forward, our goal is to improve patient outcomes and quality of life. With advancements in drug-eluting stents, biodegradable stents, and nanotechnology, the future of heart treatments looks bright.
Conclusion: Living Successfully with a Stent
We’ve looked into stents, their kinds, and how they’re put in. Living with a stent means taking care to keep it working well and your heart healthy.
Good stent care means following your meds, changing your lifestyle, and knowing about possible problems. This way, you can lower the chance of the stent getting blocked again or blood clots forming.
New stent tech and staying healthy can help you manage your condition well. It’s key to listen to your doctor and get regular check-ups to keep an eye on your stent.
Being proactive about your stent care and health can make your life full and active. Taking good care of your stent is essential for long-term success.
FAQ
What is a stent and how does it work?
A stent is a small, mesh-like device. It’s put into a narrowed or blocked artery. This keeps the artery open, improving blood flow to the heart.
It expands to fit the artery’s diameter. This holds it open, allowing blood to flow freely.
Can an artery with a stent get blocked again?
Yes, an artery with a stent can get blocked again. This is called restenosis or in-stent thrombosis. The risk depends on the stent type, patient health, and medication adherence.
What are the different types of stents used in modern medicine?
Modern medicine uses several stent types. These include bare metal stents, drug-eluting stents, and bioresorbable vascular scaffolds. Each is chosen based on the patient’s condition and the blockage’s location.
What is the stent placement procedure like?
The procedure starts with preparing the patient. Then, the stent is inserted through a catheter and expanded at the blockage site. It’s done under local anesthesia and takes about 30 minutes to an hour.
What medications are prescribed after stent placement?
Patients are given dual antiplatelet therapy (DAPT) to prevent blood clots. They also get statins to lower cholesterol. Other medications may be prescribed to manage health conditions. The medication duration varies based on the stent type and patient health.
What lifestyle changes are necessary after stent placement?
Adopting a healthy lifestyle is key. This includes a balanced diet, regular exercise, quitting smoking, and moderate alcohol use. These habits help keep the stent open and improve heart health.
What are the signs and symptoms of a blocked stent?
Signs of a blocked stent include chest pain and shortness of breath. These symptoms are similar to those before the stent was placed. If you experience them, seek emergency care right away.
Why is it important to carry a stent card?
A stent card is vital. It provides important information about the stent, like its type and when it was placed. This info helps healthcare providers make the right decisions in emergencies.
What are the complications and risks associated with stents?
Stents carry risks like bleeding, infection, restenosis, and stent thrombosis. Understanding these risks is important for making informed decisions about stent placement.
Are there any new developments in stent technology?
Yes, stent technology is evolving. New developments include next-generation drug-eluting stents and biodegradable stents. These aim to reduce reblockage risks and improve patient outcomes.
How can I maintain the health of my stent?
Keeping your stent healthy involves following medication, adopting a healthy lifestyle, and attending follow-up appointments. Being aware of complications signs is also key. Regular check-ups with your healthcare provider are essential.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/20828600/





