Last Updated on October 21, 2025 by mcelik
Blood cancer is a big health worry, mainly for older people. The chance of getting blood cancer goes up a lot after 60.
The American Cancer Society says over 192,000 new blood cancers cases are expected in the U.S. in 2025. Blood cancer happens when bad blood cells grow too much. They take over and mess with normal cells.
These cancers start in the bone marrow because of DNA changes in blood cells. Knowing who’s at risk, like older people and those with certain genes, helps find and treat it early.
Key Takeaways
- Older adults are more prone to developing blood cancer.
- The risk of blood cancer increases significantly after age 60.
- Nearly 192,000 new blood cancer cases are expected in the U.S. in 2025.
- Blood cancer is caused by mutations in the DNA of blood cells.
- Early detection and understanding risk factors are key for good treatment.
What is Blood Cancer: Understanding the Basics
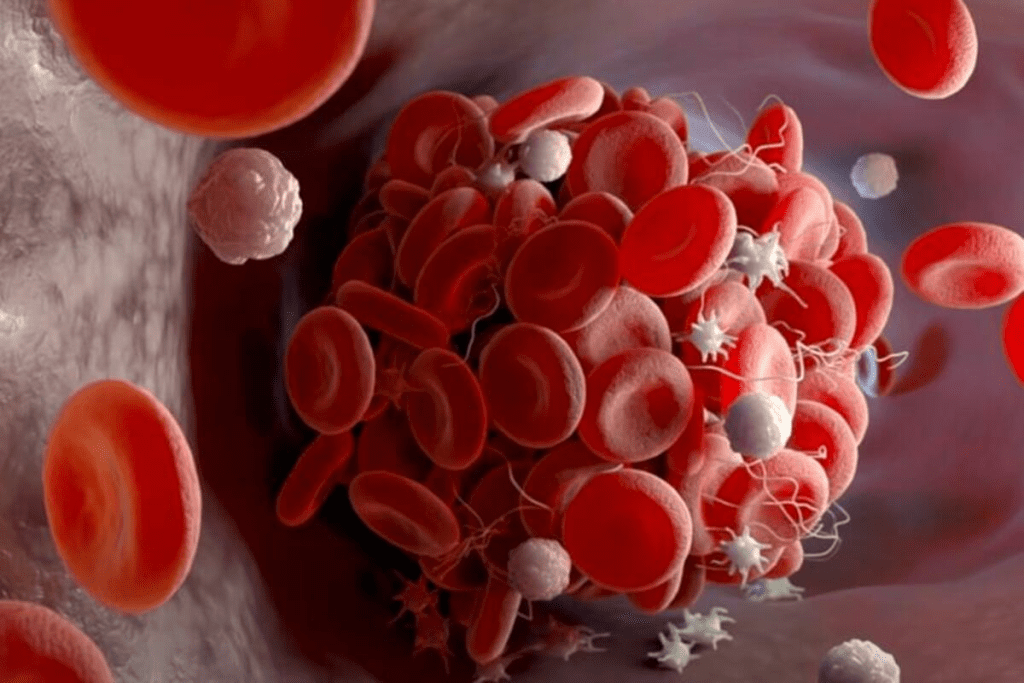
Blood cancer starts with abnormal growth in blood cells. It’s also known as cancer of the blood. This growth messes up blood function, causing health problems. It’s important to know the basics of this disease.

Common Types of Blood Cancers
There are three main types of blood cancers: leukemia, lymphoma, and myeloma. Leukemia happens in the bone marrow with too many abnormal white blood cells. Lymphoma starts in the lymphatic system’s cells. Myeloma begins in plasma cells.
Each blood cancer type is different. They affect the body in unique ways. Knowing these differences helps doctors diagnose and treat better.
How Blood Cancer Affects the Body
Blood cancer can weaken the body’s fight against infections and healing. Leukemia, for example, fills healthy cells with abnormal ones. This makes it hard to fight off infections.
Lymphoma causes swollen lymph nodes, leading to pain. Myeloma can cause anemia, bone pain, and more infections. The cause of blood cancer often comes from genetic mutations in blood cell production. Knowing how it affects the body helps find symptoms early and get the right medical care.
The Age Factor: Why Older Adults Face Higher Risk
As we get older, the risk of blood cancer grows. This is because our bodies accumulate genetic changes and environmental exposures over time. These factors increase the chance of blood cancers in older adults.
“The risk of developing leukemia, lymphoma, and myeloma increases with age, with most cases occurring in people over 60,” recent studies show. This rise in risk is due to genetics, lifestyle, and environmental exposures.
The Significant Increase in Risk After Age 60
After 60, the risk of blood cancer jumps up. This is because of genetic damage and immune system changes that come with aging. Older adults are also more affected by environmental factors like radiation and chemicals.

Older people often can’t repair DNA damage as well. This makes them more likely to get cancer. All these factors lead to more blood cancer in older adults.
Blood Cancer Incidence Across Different Age Groups
Blood cancer can happen at any age, but the risk changes a lot. It’s rare in kids and young adults but goes up after 40.
Most blood cancers are diagnosed between 65 and 70 years old. This shows why it’s key for older adults to get checked early and treated quickly.
Key statistics on blood cancer incidence across age groups include:
- Children and young adults (0-20 years): Mostly acute lymphoblastic leukemia (ALL)
- Adults (20-60 years): Increased incidence of lymphoma and other types
- Older adults (60+ years): Significant rise in leukemia, lymphoma, and myeloma
Knowing how age affects blood cancer is vital for prevention and treatment. Our healthcare network offers special care for older adults with blood cancer. We focus on support and advanced treatments.
Gender Differences: Why Men Are More Vulnerable
Men are more likely to get blood cancer than women. This is true for leukemia, lymphoma, and myeloma. The exact reasons are not fully known but involve genetics, hormones, and the environment.
Statistical Evidence of Male Predominance
Research shows men get blood cancer more often than women. For example, some types of leukemia and lymphoma hit men harder. This pattern is seen in all ages and ethnic groups, pointing to a gender-related factor.
Key statistics highlighting this disparity include:
- Higher incidence rates of leukemia among men.
- Increased prevalence of certain lymphoma subtypes in men.
- Greater risk of multiple myeloma in men compared to women.
Gender-Specific Variations in Blood Cancer Types
Different blood cancers affect men and women differently. For instance, CLL is more common in men, while women are more likely to get certain lymphoma subtypes. Knowing these differences helps doctors create better treatment plans.
The survival rate of blood cancer also varies by gender. Some studies suggest women might live longer than men with blood cancer. Survival depends on the cancer type, treatment response, and overall health.
We understand blood cancer impacts people in unique ways, regardless of gender. Our medical team focuses on personalized care for blood cancer patients. We tailor treatments to meet each patient’s specific needs and situation.
Racial and Ethnic Risk Patterns in the United States
In the U.S., the risk of blood cancer varies among different ethnic and racial groups. Some groups face a higher risk of certain blood cancers.
Caucasians tend to have more cases of lymphoma and myeloma than others. This shows we need to find out why these differences exist.
Higher Prevalence Among Caucasian Americans
Caucasian Americans are more likely to get lymphoma and myeloma. The reasons for this are complex. They might include genetics, environment, and lifestyle.
- Genetics could be a factor in why Caucasians are at higher risk.
- Exposure to harmful radiation might also play a part.
- How we live, including our diet and exercise, could affect our risk too.
Comparative Rates Between Different Ethnic Groups
Studies show African Americans face a higher risk of some leukemias than Caucasians. This highlights the need for specific prevention and treatment plans.
It’s important to take these differences into account when creating health programs and guidelines for blood cancer.
By understanding these patterns, we can make our prevention and treatment efforts more effective. This will help improve outcomes for everyone.
Genetic Predisposition and Family History
A family history of blood cancer can greatly raise your risk. We understand the role of genetics in identifying those at higher risk. This helps us provide the right care.
Genetics are key in blood cancer development. Some genetic disorders raise the risk of leukemia, lymphoma, and myeloma. For example, people with Down syndrome are more likely to get leukemia.
Hereditary Factors That Increase Vulnerability
Hereditary factors greatly affect blood cancer risk. Research has found genetic mutations linked to blood cancer. For instance, TP53 gene mutations increase cancer risk, including blood cancers.
Some key hereditary factors include:
- Family history of blood cancer
- Genetic syndromes like Li-Fraumeni syndrome
- Chromosomal instability syndromes
Congenital Conditions Linked to Blood Cancer Risk
Certain conditions present at birth can raise blood cancer risk. Some congenital conditions are linked to leukemia and other blood cancers.
For example, people with:
- Down syndrome
- Fanconi anemia
- Bloom syndrome
face a higher risk of blood cancer due to their genetics.
We stress the need for genetic counseling and screening. This is for those with a family history of blood cancer or congenital conditions that raise risk.
Environmental Exposures That Trigger Blood Cancer
Environmental factors like radiation and chemicals can lead to blood cancer. We know that some environmental elements raise the risk of this disease.
The Impact of Ionizing Radiation
Ionizing radiation is a known risk factor for blood cancer. High levels of ionizing radiation, from nuclear accidents or medical procedures, can harm the bone marrow. This can cause leukemia. We stress the need to limit exposure to ionizing radiation to lower blood cancer risk.
Chemical Exposures Including Benzene
Chemical exposures, like benzene, increase blood cancer risk. Benzene is used in many industrial processes. Long-term exposure to it can cause leukemia. We urge for strict safety measures in workplaces where benzene is used to prevent exposure.
Previous Cancer Treatments as Risk Factors
Previous cancer treatments, like chemotherapy and radiation therapy, can also raise blood cancer risk. These treatments are often needed to fight primary cancers. Yet, we emphasize the importance of watching for signs of blood cancer in those who have had these treatments.
Knowing about these environmental risk factors is key to preventing and catching blood cancer early. By reducing exposure to ionizing radiation, certain chemicals, and being mindful of cancer treatment risks, people can lower their chance of getting blood cancer.
Lifestyle Factors Contributing to Blood Cancer Risk
Many lifestyle choices can increase the risk of blood cancer. Making smart choices can greatly improve our health and lower cancer risk.
Obesity and Physical Inactivity Connection
Studies show that obesity and not being active raise the risk of blood cancer. Staying at a healthy weight and exercising regularly can help. We suggest doing at least 150 minutes of moderate exercise or 75 minutes of intense exercise weekly.
Important points to remember:
- Being overweight causes chronic inflammation, which can lead to cancer.
- Regular exercise boosts the immune system and lowers cancer risk.
- Eating a diet full of fruits, veggies, and whole grains is good for health.
Smoking and Tobacco Use Effects
Smoking and tobacco use are major risks for many cancers, including blood cancer. Tobacco smoke’s chemicals harm cell DNA, causing cancer. Quitting smoking is key to lowering cancer risk. We urge smokers to get help to quit.
The dangers of smoking include:
- Higher risk of acute myeloid leukemia (AML).
- Exposure to carcinogens that cause genetic mutations.
- Damage to the bone marrow, where blood cells are made.
The Role of Hypercholesterolemia
Hypercholesterolemia, or high cholesterol, is linked to many health problems, including cancer risk. While the exact link to blood cancer is being studied, managing cholesterol is vital for health. This can be done through diet, exercise, and medication if needed.
- Eat a heart-healthy diet low in saturated fats and high in soluble fiber.
- Regular physical activity improves lipid profiles.
- Keep an eye on cholesterol levels and work with a healthcare provider to manage them.
By tackling these lifestyle factors, we can lower our risk of blood cancer and improve our health.
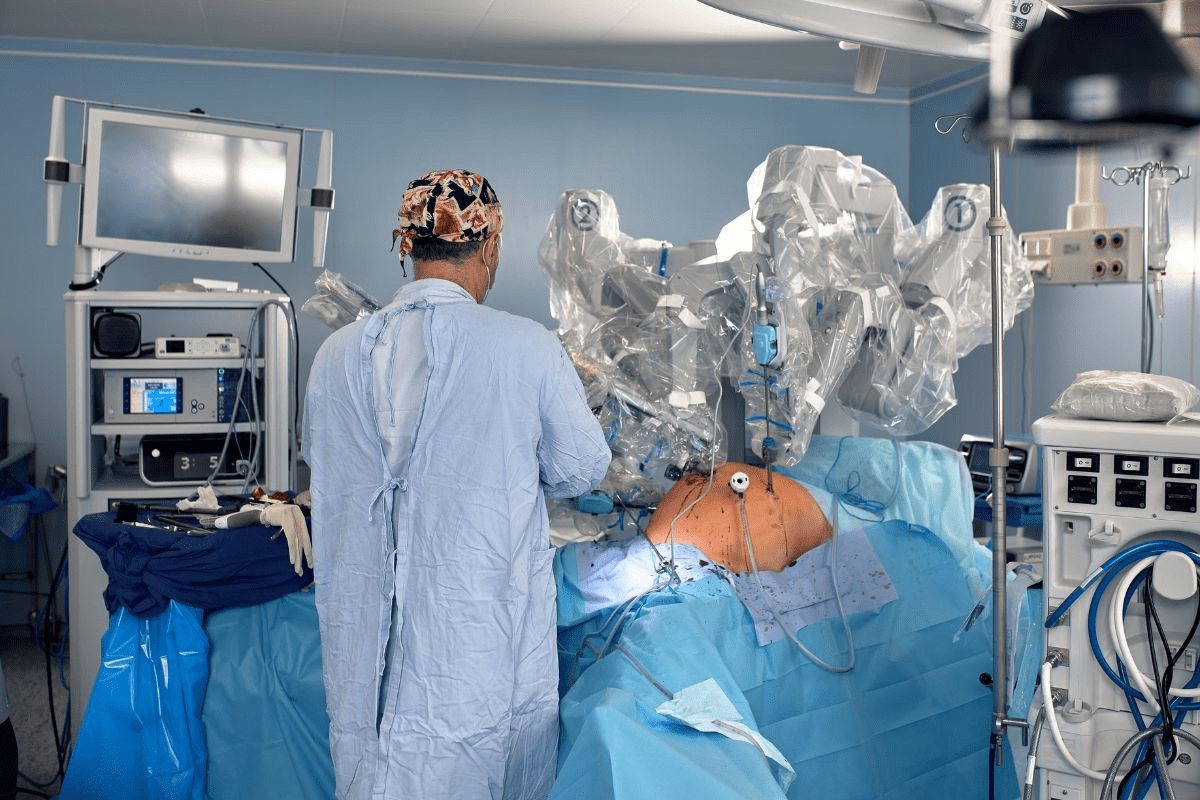
Conclusion: Advances in Prevention, Detection, and Treatment
Therapies and detection methods have greatly changed how we deal with blood cancer. People with a family history or who have had chemotherapy before are at higher risk. It’s key to know the leukemia risk factors early on.
Thanks to new treatments, survival rates for blood cancer have gone up. Catching it early and treating it fast is vital for better results. We aim to give top-notch healthcare to international patients, helping them live longer with blood cancer.
Our network is dedicated to ongoing research and education to help blood cancer patients. By leading in medical advancements, we offer the best care for this challenging condition.
FAQ
What is blood cancer, and how does it affect the body?
Blood cancer, also known as leukemia, is a cancer of the blood cells. It happens when the bone marrow makes bad white blood cells. This can cause anemia, infections, and bleeding problems. We offer full care for blood cancer patients, including diagnosis, treatment, and support.
What are the different types of blood cancer, and how are they treated?
Blood cancer types include leukemia, lymphoma, and multiple myeloma. Treatment depends on the type, stage, and patient’s health. Our team gives personalized care, using chemotherapy, radiation, and targeted therapy.
How does age affect the risk of developing blood cancer?
Blood cancer risk grows with age, mostly in people over 60. We focus on older adults, considering their unique needs and health.
Are men more likely to develop blood cancer than women?
Yes, men face a higher risk of blood cancer than women. But the exact reasons are unclear. Our team cares for all patients, focusing on their individual needs.
What are the risk factors for blood cancer?
Risk factors include genetic predisposition, radiation, chemical exposure, and past cancer treatments. We help patients avoid these risks and offer genetic counseling.
Can lifestyle factors contribute to the risk of developing blood cancer?
Yes, lifestyle factors like obesity, lack of exercise, and smoking increase blood cancer risk. We advise on healthy living, including diet, exercise, and avoiding tobacco.
What is the survival rate for blood cancer, and how does it vary by age and type of cancer?
Survival rates for blood cancer depend on the type, stage, age, and health. We offer personalized care and support to help patients achieve the best outcomes.
How can I reduce my risk of developing blood cancer?
While some risks can’t be avoided, healthy living can help. Avoid radiation and chemicals, and get regular check-ups. We provide prevention advice and screenings.
What causes blood cancer, and can it be prevented?
Blood cancer is caused by genetics and environment. While prevention is not always possible, reducing risk is. We offer full care for blood cancer patients.
How do you get blood cancer?
Blood cancer starts when the bone marrow makes bad white blood cells. It can be triggered by genetics, radiation, and chemicals. We guide on avoiding these risks and offer screenings.
References
- Mohammadian-Hafshejani, A., et al. (2024). Global incidence and mortality of childhood leukemia and lymphoma: A systematic review. International Journal of Cancer. https://pmc.ncbi.nlm.nih.gov/articles/PMC11218982/
- National Cancer Institute. (2025). Cancer Stat Facts: Childhood Leukemia (Ages 0“19) – SEER. https://seer.cancer.gov/statfacts/html/childleuk.html
- American Cancer Society. (2025). Prognostic Factors and Survival Rates for Childhood Leukemia. https://www.cancer.org/cancer/types/leukemia-in-children/detection-diagnosis-staging/survival-rates.html