Learn what is coronary artery disease CAD, its causes, symptoms, and treatment options.
Coronary Artery Disease (CAD) happens when the heart’s blood vessels get narrowed or blocked. This is due to fatty plaque buildup, known as atherosclerosis.
Heart disease is the top killer in the U.S. for men, women, and most racial groups. CAD is the main culprit, causing 371,506 deaths in 2022.
At Liv Hospital, we help people manage their heart health. We offer detailed care and education on CAD. This includes its symptoms, diagnosis, and treatment options. We use international standards and new protocols.
Key Takeaways
- Understanding CAD is key for prevention and care.
- CAD is the most common heart disease.
- Knowing CAD symptoms can save lives.
- Liv Hospital offers detailed care and education on CAD.
- Teaching CAD patients is vital for managing the condition.
1. What Is Coronary Artery Disease (CAD)?
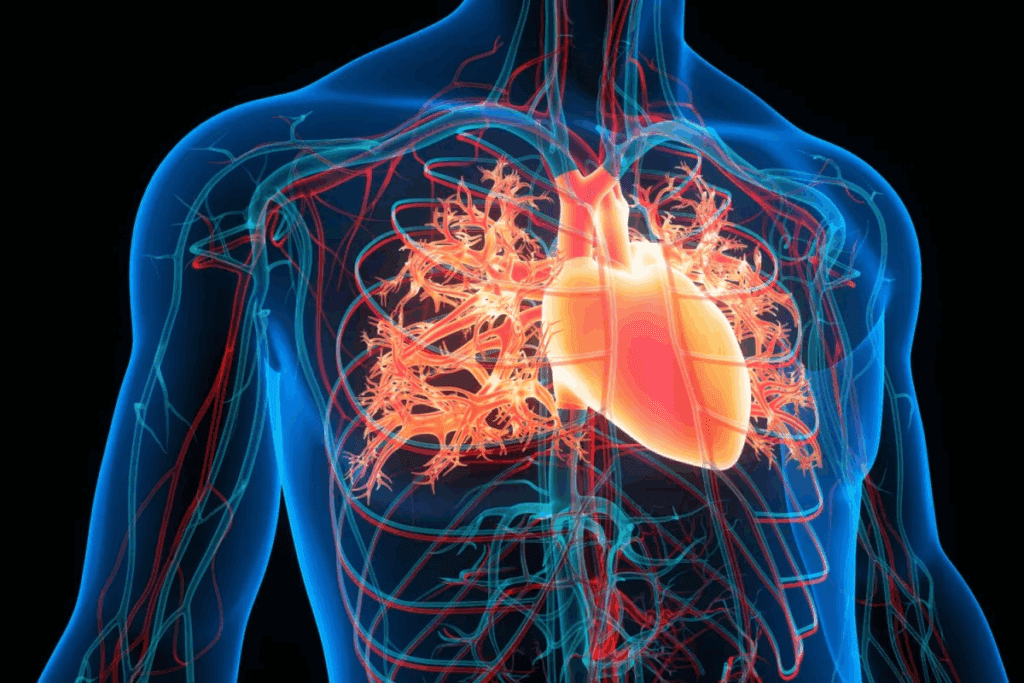
Coronary Artery Disease (CAD) is a heart condition that makes it hard for the heart to get the oxygen it needs. It happens when the arteries that bring blood to the heart muscle get blocked or narrowed. This is because of a buildup of plaque, known as atherosclerosis.
Definition and Pathophysiology
CAD is a heart disease that stops the heart’s arteries from bringing enough oxygen-rich blood. The arteries narrow because of plaque buildup, reducing blood flow to the heart.
Understanding CAD shows how it affects the heart. The heart needs a steady supply of oxygen-rich blood to work right. When CAD happens, this supply is cut off, leading to chest pain, heart attacks, or other serious issues.
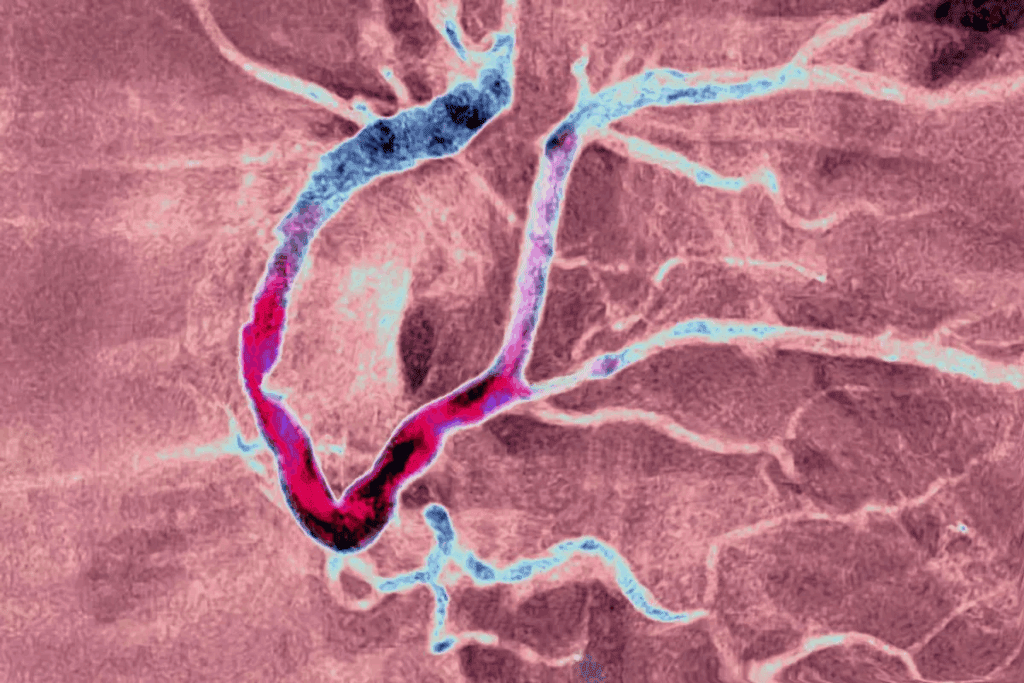
The Process of Atherosclerosis
Atherosclerosis is the main cause of CAD. It’s when fatty deposits, or plaque, build up inside the heart’s arteries. Over time, this plaque can harden or burst, narrowing or blocking the artery.
The atherosclerosis process is complex. It’s influenced by high cholesterol, smoking, and high blood pressure. As plaque grows, it reduces blood flow to the heart, causing symptoms like angina.
| Stage | Description | Impact on Heart |
| Initial Plaque Buildup | Fatty deposits start to accumulate on artery walls. | Minimal impact; often asymptomatic. |
| Plaque Progression | Plaque continues to build up, narrowing the artery. | Reduced blood flow; possible angina. |
| Artery Blockage | Plaque ruptures or significantly narrows the artery. | Significant reduction in blood flow; risk of heart attack. |
Visual Understanding: How CAD Affects Your Heart
To grasp CAD, it helps to see how it impacts the heart. The coronary arteries surround the heart, bringing it oxygen-rich blood. When plaque builds up, it’s like a kink in a hose, restricting blood flow.
By understanding CAD and its heart effects, people can see why managing risk factors and getting medical help when symptoms appear is so important.
2. CAD Is the Most Common Type of Heart Disease
Coronary Artery Disease (CAD) is the most common heart disease, affecting millions globally. It’s important to understand its impact, mainly in the United States.
CAD is a big public health issue, causing economic and health problems. About 1 in 20 adults over 20 have CAD, which is about 5% of this age group.
Prevalence Statistics in the United States
In the U.S., CAD is a major concern. It’s responsible for about 1 out of 6 deaths from heart disease in adults under 65. This shows how serious CAD is.
The cost of heart disease, including CAD, is huge. From 2020 to 2021, it cost around $417.9 billion. This shows the big financial hit CAD takes on healthcare and the economy.
Demographics Most Affected
CAD hits different groups in different ways. Age is a big risk factor, with older adults being more affected. Some ethnic groups and those with heart disease in their families are also at higher risk.
Knowing who is most at risk helps us target our efforts. We can use this info to focus on prevention and treatment for these groups.
Global vs. USA Coronary Artery Disease Rates
CAD is a worldwide problem, but its rate varies. The U.S. has one of the higher rates among developed countries. Looking at global and U.S. rates helps us understand risk factors and how to improve.
By studying these differences, we can learn from other countries. We might find ways to improve CAD management in the U.S. based on their success.
3. Understanding CAD Terminology and Related Conditions
It’s key to know the terms around Coronary Artery Disease (CAD). This is important for both patients and doctors. CAD is often mixed up with other heart issues, causing confusion.
Is Coronary Artery Disease the Same as Heart Disease?
Coronary Artery Disease (CAD) and heart disease are not the same. Heart disease is a wide term for many heart problems, like CAD, heart failure, and arrhythmias. CAD is about the narrowing or blockage of coronary arteries because of atherosclerosis.
This difference is vital. While all CAD is heart disease, not all heart disease is CAD. Knowing this helps in diagnosing and treating the right condition.
Coronary Artery Disease Is Also Referred to as Coronary Heart Disease
CAD is also known as Coronary Heart Disease (CHD). This shows how the disease affects the heart’s coronary arteries. Both terms are used in medical texts, showing the disease’s impact on the heart’s function.
Is CAD the Same as Ischemic Heart Disease?
Ischemic Heart Disease (IHD) is another name for CAD. IHD points out the reduced blood flow to the heart muscle because of narrowed or blocked arteries. So, CAD and IHD describe the same condition, with a focus on the disease process (CAD) or its effects (IHD).
CAD Medical Abbreviation and Common Misunderstandings
The medical term for Coronary Artery Disease is CAD. Many think CAD is rare, but it’s actually very common worldwide. Another mistake is thinking CAD only hits older people or those with clear risk factors. But, CAD can affect many, often without symptoms until a big event happens.
By clearing up these terms, we can talk better about CAD. This ensures patients get the right diagnosis and care.
4. Angina: The Most Common Symptom of Coronary Artery Disease
Angina is chest pain or discomfort. It’s the most common symptom of Coronary Artery Disease (CAD). It happens when the heart doesn’t get enough oxygen-rich blood. This usually happens during physical activity or when feeling stressed.
Types of Angina
There are different types of angina. Each type has its own characteristics. Knowing these can help doctors diagnose and treat CAD better.
- Stable Angina: This is chest pain that comes and goes. It happens when you’re active or stressed and goes away with rest or medicine.
- Unstable Angina: This pain is unpredictable. It can happen when you’re resting, is more severe, or is a new pain. It’s a sign of a possible heart attack.
- Variant Angina: This pain happens when you’re resting. It’s caused by a spasm in the coronary arteries, reducing blood flow.
- Microvascular Angina: This pain is from small blood vessels in the heart. It often doesn’t show blockages in the big arteries.
How Angina Feels and When It Occurs
Angina feels like a squeeze or pressure in the chest. It might spread to the arms, back, neck, jaw, or stomach. It’s uncomfortable but usually goes away. It often happens during:
- Physical exertion
- Emotional stress
- After a heavy meal
- In cold or hot weather
Not everyone with CAD gets angina. About 1 in 5 heart attacks are silent. This means the damage happens without the person knowing it.
CAD with Angina: What to Expect
For those with CAD and angina, managing it is key. This includes lifestyle changes, medicine, and sometimes surgery. Knowing what triggers angina and how to handle it is important.
| Management Strategy | Description |
| Lifestyle Changes | Diet, exercise, quitting smoking, and managing stress. |
| Medications | Nitrates, beta-blockers, and antiplatelet drugs to reduce angina and manage CAD. |
| Surgical Interventions | Angioplasty and stenting or CABG to improve blood flow to the heart. |
Understanding angina helps those with CAD manage their condition better. This improves their quality of life.
5. The Silent Danger: CAD Without Angina
CAD without angina is a big worry. It can cause sudden heart attacks or cardiac arrests.
Not all people with Coronary Artery Disease (CAD) get chest pain. Some have different symptoms or no symptoms at all until a serious heart event happens.
Atypical Symptoms to Watch For
While chest pain is common, some CAD patients have different symptoms. These include:
- Shortness of breath
- Fatigue
- Pain or discomfort in the arms, back, neck, jaw, or stomach
- Dizziness or lightheadedness
These symptoms can be hard to notice. They might be mistaken for other health issues. It’s important to pay attention to your heart health.
Why Some Patients Remain Asymptomatic
There are several reasons why some CAD patients don’t show symptoms:
| Factor | Description |
| Gradual Narrowing | The slow narrowing of arteries might not cause noticeable symptoms until it’s too late. |
| Collateral Circulation | Some people develop extra blood vessels. These help hide symptoms of reduced blood flow. |
| Individual Variability | How people feel pain and react to CAD can vary a lot. This affects whether symptoms are noticed. |
Knowing these reasons is key for both patients and doctors to manage CAD well.
CAD Without Angina: Detection Challenges
Finding CAD without chest pain is hard. Regular check-ups and tests are very important for early detection.
Doctors use risk checks, medical history, and tests to find CAD in people without symptoms.
By knowing the risks and looking out for different symptoms, people can help keep their heart healthy. This is true even if they don’t have typical chest pain symptoms.
6. Major Risk Factors for Developing CAD
Knowing the main risk factors for CAD is key to preventing it. Coronary Artery Disease (CAD) is shaped by many factors. Some can be controlled, while others can’t.
Modifiable Risk Factors
Modifiable risk factors are things we can change to lower CAD risk. These include:
- High Blood Pressure: High blood pressure can harm blood vessel linings, making them more likely to block.
- High Blood Cholesterol: Too much LDL cholesterol can cause artery plaque buildup.
- Smoking: Smoking harms the heart and blood vessels, raising CAD risk a lot.
- Diabetes: Diabetes can damage blood vessels and heart nerves.
- Obesity and Physical Inactivity: Being overweight and not moving much can lead to CAD.
- Unhealthy Diet: Eating too much saturated fats, trans fats, and cholesterol can increase CAD risk.
The American Heart Association says, “Changing these risk factors through lifestyle and medicine can prevent or slow CAD.”
“A healthy lifestyle is key to preventing heart disease. This includes a balanced diet, regular physical activity, not smoking, and maintaining a healthy weight.”
Non-Modifiable Risk Factors
Non-modifiable risk factors are things we can’t change. These include:
- Age: CAD risk goes up with age.
- Family History: A family history of CAD, even at a young age, raises risk.
- Gender: Men are generally at higher risk than women, but women’s risk goes up after menopause.
“Knowing these non-modifiable risk factors helps people take steps to lower their overall risk.”
High CAD Risk: Who Should Be Most Concerned
People with both modifiable and non-modifiable risk factors face the highest CAD risk. For example, a smoker with high blood pressure and a family history of CAD is at much higher risk than someone without these factors.
It’s vital for those at high risk to work with their healthcare providers. They can manage risk factors through lifestyle changes, medicine, or other tailored interventions.
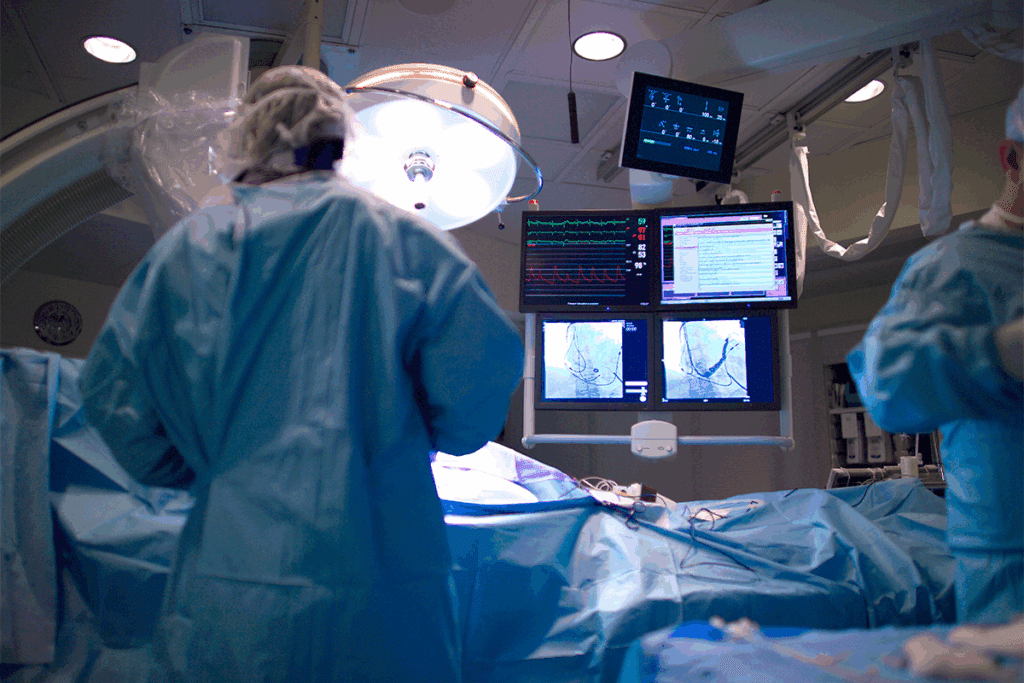
7. How CAD Is Diagnosed
Diagnosing coronary artery disease involves looking at symptoms, medical history, and test results. Your doctor will use your symptoms, medical and family history, risk factors, and heart test results to make a diagnosis.
Non-Invasive Diagnostic Tests
Non-invasive tests are key for diagnosing CAD safely. These include:
- Electrocardiogram (ECG or EKG): Records the heart’s electrical activity.
- Stress Test: Checks how the heart works under stress.
- Echocardiogram: Uses sound waves to show heart images.
| Test | Purpose | Benefits |
| Electrocardiogram (ECG) | Records heart’s electrical activity | Quick, painless, and gives immediate results |
| Stress Test | Evaluates heart function under stress | Helps identify CAD, assesses heart’s response to exertion |
| Echocardiogram | Creates images of the heart | Provides detailed information on heart structure and function |
Invasive Diagnostic Procedures
When non-invasive tests are unclear, invasive procedures might be needed. These include:
- Coronary Angiography: Uses dye and X-rays to see the coronary arteries.
- Cardiac Catheterization: Involves a catheter in the heart to diagnose and treat CAD.
Coronary Artery Disease Illustrations in Diagnosis
Visual aids like angiograms and echocardiograms are vital in diagnosing CAD. They help doctors see the extent and location of blockages. This guides treatment choices.
By combining test results, doctors can accurately diagnose CAD. They then create a treatment plan that meets the patient’s needs.
8. The Relationship Between CAD and Heart Failure
Coronary Artery Disease (CAD) and heart failure are closely linked. CAD often leads to heart failure if not managed well. CAD happens when the heart’s main blood vessels get damaged or diseased.
This damage is usually due to atherosclerosis. It’s a condition where plaque builds up in the arteries.
Progression to Heart Failure
CAD can cause heart failure in several ways. When the heart’s arteries are diseased, it doesn’t get enough oxygen-rich blood. This leads to ischemia.
Long-term ischemia can cause a heart attack. A heart attack damages the heart muscle and can lead to heart failure. Heart failure happens when the heart can’t pump enough blood for the body’s needs.
Key factors that contribute to the progression from CAD to heart failure include:
- Myocardial infarction (heart attack)
- Chronic ischemia
- Arrhythmias
- Cardiac remodeling
Prognosis for Patients with Both Conditions
Patients with both CAD and heart failure face a tougher prognosis than those with CAD alone. Heart failure means the disease is more advanced and the risk of complications is higher. But, with the right treatment, quality of life and prognosis can improve.
Effective management strategies include:
- Optimizing medical therapy for heart failure and CAD
- Implementing lifestyle changes such as diet, exercise, and smoking cessation
- Monitoring for and managing complications
- Considering device therapy or surgical interventions as needed
Managing CAD and Heart Failure Together
Managing CAD and heart failure together needs a detailed plan. This plan includes careful medication, lifestyle changes, and regular monitoring. By focusing on both conditions, healthcare providers can better help patients.
Every patient is different, so treatment plans are made just for them. Working with patients and their families helps create effective care plans. This improves their quality of life and prognosis.
9. Treatment Options and Patient Education for CAD
Managing CAD requires a wide range of treatments. This includes educating patients, making lifestyle changes, and using medical treatments. “Patient education is the cornerstone of CAD management,” as it helps people manage their condition better.
Lifestyle Modifications
Lifestyle changes are key in managing CAD. These include eating a healthy diet, staying active, and quitting smoking. A good diet for CAD patients should be low in fats and sodium but high in fruits and whole grains.
Regular exercise, like walking, can improve heart health. It helps lower blood pressure and improve cholesterol levels. Always talk to a doctor before starting any new exercise.
Medication Approaches
Medicines are also important in managing CAD. Statins lower cholesterol, beta-blockers control blood pressure, and antiplatelet agents prevent blood clots. Taking medicines as directed is key to managing CAD.
“Adherence to medication is a critical aspect of CAD management, as it can significantly reduce the risk of heart attacks and other cardiovascular events.”
Interventional Procedures and Surgery
For some, lifestyle changes and medicines may not be enough. In these cases, procedures or surgery might be needed. Angioplasty and stenting are used to open blocked arteries. For severe cases, coronary artery bypass grafting (CABG) might be recommended.
CAD Patient Education: Essential Knowledge for Self-Management
Teaching patients about CAD is vital for self-management. Educated patients can better understand their condition and follow treatment plans. Educational programs cover symptoms, medication, and lifestyle changes.
10. Conclusion: Living with CAD and Future Outlook
Coronary Artery Disease (CAD) is a serious health issue that needs quick action and care. To live with CAD, you must make lifestyle changes, take medicine, and sometimes undergo procedures.
Managing CAD well is key to avoiding heart attacks and improving life quality. Early detection and treatment are critical. They help people with CAD stay active and healthy.
For those with CAD, knowing the signs of a heart attack is vital. Acting fast when you feel symptoms can save your life. With the right care and sticking to treatment plans, CAD patients can look forward to a long, healthy life.
We stress the need for a proactive approach to managing CAD. Patients should work closely with their doctors. This way, they can keep their condition in check and adjust treatments as needed.
FAQ:
What is coronary artery disease (CAD)?
Coronary artery disease (CAD) is when the heart’s main blood vessels get damaged. This damage is often due to plaque buildup, which narrows or blocks the arteries.
Is coronary artery disease the same as heart disease?
No, CAD and heart disease are not the same. Heart disease is a wide term for many heart issues. CAD is a specific heart disease that affects the heart’s arteries.
What is the most common symptom of coronary artery disease?
The most common symptom is angina. It’s chest pain or discomfort when the heart doesn’t get enough oxygen. It can feel like pressure or squeezing in the chest and other areas.
Can you have CAD without angina?
Yes, you can have CAD without angina. Some people might not show symptoms or have different symptoms. This makes it hard to detect CAD without a medical check-up.
What are the major risk factors for developing CAD?
Major risk factors include high blood pressure, high cholesterol, smoking, diabetes, and obesity. Non-modifiable factors like age, family history, and genetics also play a role.
How is CAD diagnosed?
Doctors use medical history, physical exams, and tests to diagnose CAD. Tests include ECG, stress tests, and echocardiograms. They might also do coronary angiography.
What is the relationship between CAD and heart failure?
CAD can damage the heart muscle, making it hard to pump blood. If CAD is not treated, it can lead to heart failure. Heart failure means the heart can’t supply enough blood and oxygen.
What are the treatment options for CAD?
Treatments include lifestyle changes, like diet and exercise. Medications help manage symptoms and risk factors. Procedures like angioplasty and CABG are also options.
Is CAD patient education important for managing the condition?
Yes, educating patients about CAD is key. Knowing about the condition, treatments, and lifestyle changes helps patients make better choices. This improves their health outcomes.
Can CAD be managed to allow for a healthy life?
Yes, managing CAD is possible with the right approach. This includes lifestyle changes, medication, and medical treatments. Early treatment and management can prevent complications and improve quality of life.
References:
Brown, J. C. (2023). Risk factors for coronary artery disease. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK554410/