Panuveitis is a rare and serious eye condition. It causes inflammation in all layers of the uvea. At Liv Hospital, we recognize the importance of early diagnosis and treatment to prevent permanent vision loss. This condition demands urgent medical attention and specialized care to manage its complex symptoms effectively.
Understanding panuveitis is key for effective management. It involves widespread inflammation in the eye’s uvea. This can impact vision and overall eye function. We emphasize coordinated multidisciplinary care to preserve vision in patients affected by this condition. Asking what is panuveitis? Our essential guide explains the causes, serious symptoms, and critical treatment options you need to know.
Key Takeaways
- Panuveitis is a severe form of uveitis affecting all layers of the uvea.
- Early diagnosis and treatment are critical to prevent vision loss.
- Coordinated care is essential for managing panuveitis effectively.
- Understanding the causes and symptoms is vital for effective treatment.
- Liv Hospital provides specialized care for panuveitis patients.
Understanding the Eye’s Uveal Tract
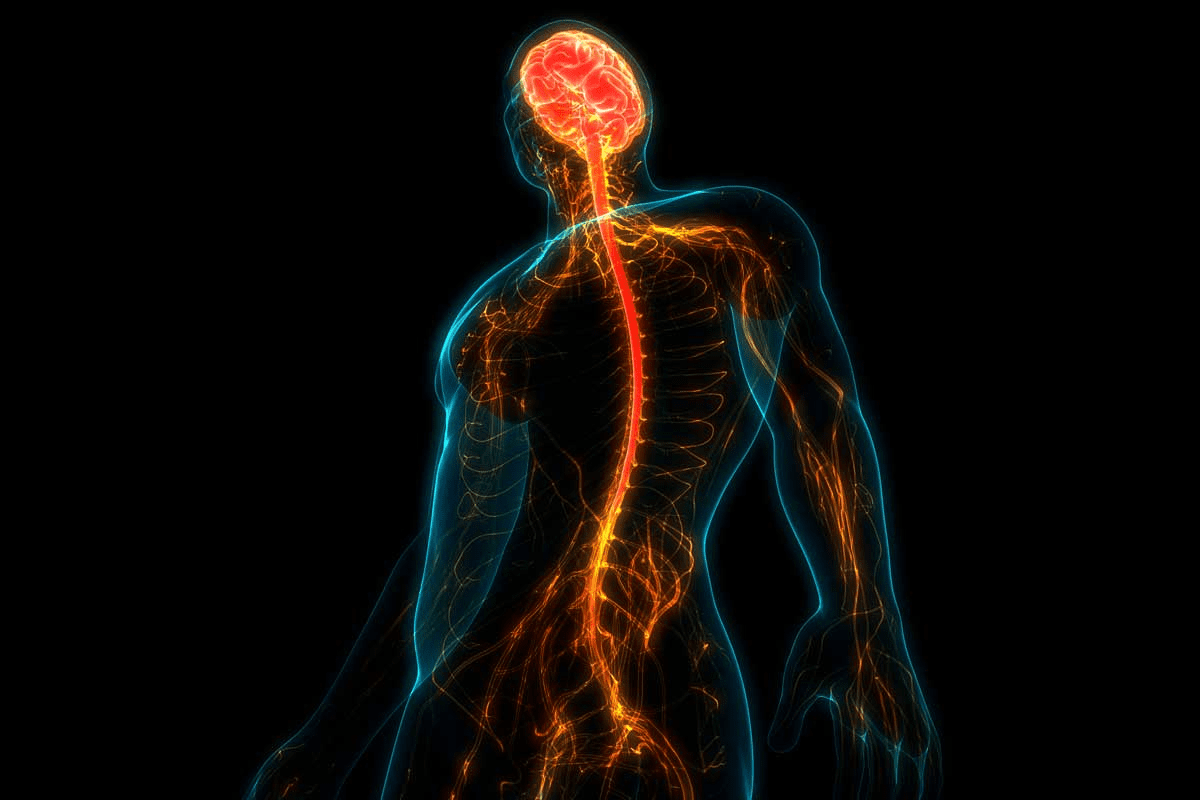
It’s key to know about the uveal tract to understand panuveitis. The uveal tract, or uvea, is the middle layer of the eye. It gives the eye the blood it needs to stay healthy.
Anatomy of the Uvea
The uvea has three main parts: the iris, ciliary body, and choroid. The iris controls how much light gets in by changing the pupil’s size. The ciliary body makes the fluid that feeds the lens and cornea, and it changes the lens for clear vision. The choroid is a big layer of blood vessels that gives the retina oxygen and nutrients.
Uveal Component | Function |
Iris | Controls light entry by adjusting pupil size |
Ciliary Body | Produces aqueous humor and changes lens shape for focusing |
Choroid | Supplies retina with oxygen and nutrients |
Function of the Uveal Tract in Vision
The uveal tract is vital for the eye’s health. It feeds the retina and other parts of the eye. When it gets inflamed, like in panuveitis, it can harm vision.
“The uvea is a vital structure for the eye’s overall health, and its inflammation can have serious implications for vision.”
Medical Expert
Knowing about the uveal tract helps us see how panuveitis affects the eye. It shows why treating eye inflammation is so important.
What Is Panuveitis?
Panuveitis is an inflammatory condition that affects the entire uvea. This middle layer of the eye includes the iris, ciliary body, and choroid. When it occurs, it can cause inflammation in all these structures, potentially leading to complications that affect vision.
Definition and Classification
Panuveitis is defined as inflammation that involves all layers of the uvea: the iris, ciliary body, and choroid. It can be classified based on its etiology, duration, and anatomical location. According to the Standardization of Uveitis Nomenclature (SUN) Working Group, panuveitis is characterized by inflammation in the anterior chamber, vitreous, and choroid or retina.
“Panuveitis represents a significant challenge in ophthalmology due to its high risk of causing severe visual impairment,” as noted by experts in the field of uveitis.
How Panuveitis Differs from Other Forms of Uveitis
Uveitis can be categorized into different types based on the part of the uvea affected. Anterior uveitis involves the iris and ciliary body, intermediate uveitis affects the vitreous, and posterior uveitis involves the choroid and retina. Panuveitis, on the other hand, is distinguished by its involvement of all these structures, making it a more complex and potentially severe form of uveitis.
Impact on the Entire Eye Structure
Panuveitis can have far-reaching consequences on the eye’s structure and function. Inflammation can lead to complications such as cataract formation, secondary glaucoma, retinal detachment, and optic nerve damage. The condition can also result in vision loss if not promptly and effectively treated.
As
“The management of panuveitis requires a complete approach to address the underlying cause, control inflammation, and prevent complications.”
This highlights the importance of a thorough treatment plan in managing panuveitis and preserving vision.
Epidemiology and Risk Factors
The study of panuveitis shows us how common it is and who it affects. Knowing this helps doctors and researchers find better ways to treat it. This can lead to better results for patients.
Prevalence and Incidence Rates
Panuveitis makes up about 10–15% of all uveitis cases globally. Its occurrence changes based on where you are and your genes. It’s not as common as other uveitis types, but it can cause serious vision loss.
Demographics Most Affected
Most people with panuveitis are adults between 20 and 50. It affects men and women almost equally. Some ethnic groups might be more likely to get it due to their genes.
Genetic Predispositions
Genes play a big part in getting panuveitis. If you have a family history of certain diseases or specific genes, you’re more at risk. Knowing this can help doctors diagnose and treat you better.
Panuveitis is a complex issue. It’s influenced by genes, environment, and who you are. By studying it, we can manage it better. This helps improve life for those with the condition.
Common Causes of Panuveitis
Panuveitis can be caused by infections, autoimmune disorders, and trauma. Knowing these causes helps in finding the right treatment.
Infectious Triggers
Infections are a big reason for panuveitis. They can come from bacteria, viruses, and parasites. Some common ones include:
- Toxoplasmosis, a parasitic infection that can reactivate in the eye
- Tuberculosis, a bacterial infection that can affect the uveal tract
- Viral infections such as herpes simplex and varicella-zoster
These infections can cause eye inflammation, leading to panuveitis. Finding out the exact cause is key for effective treatment.
Autoimmune Conditions
Autoimmune diseases also cause panuveitis. Conditions like sarcoidosis and Behcet’s disease can lead to eye inflammation. Sarcoidosis, for example, can cause inflammation in different parts of the body, including the eyes.
Behcet’s disease is known for oral, genital ulcers, and uveitis. It can cause severe panuveitis if not treated well.
Traumatic Eye Injury
Eye injuries can also lead to panuveitis. The injury can cause inflammation and may introduce infections. Traumatic uveitis is a serious complication of eye injuries and needs quick treatment to avoid lasting damage.
The ICD-10 coding for traumatic uveitis is important for insurance and medical records. It shows the need for accurate diagnosis and coding.
Vogt-Koyanagi-Harada Syndrome
Vogt-Koyanagi-Harada (VKH) syndrome is a rare autoimmune condition that can cause panuveitis. It has neurological, dermatological, and ocular symptoms. VKH syndrome is more common in certain groups, like people of Asian or Native American descent.
The exact cause of VKH syndrome is not known, but it’s thought to be an autoimmune response against melanin-containing cells. Treatment usually involves immunosuppressive therapy to control the autoimmune response.
In conclusion, panuveitis has many causes, including infections, autoimmune disorders, trauma, and rare syndromes. Understanding these causes is vital for managing and treating the condition effectively.
Recognizing Panuveitis Symptoms
It’s important to spot the early signs of panuveitis to avoid vision damage. We’ll cover the main symptoms and how panuveitis can show up differently.
Early Warning Signs
Panuveitis starts with signs like eye pain, redness, and sensitivity to light. You might see blurred vision or floaters in your sight.
An expert says, “Finding panuveitis early is key to treating it well and avoiding problems.”
“The key to managing panuveitis lies in recognizing its symptoms early and seeking medical attention promptly.”
Common Symptoms
People with panuveitis often feel eye discomfort and see vision changes. They might notice blurred or decreased vision, floaters, and feel more sensitive to light. If not treated quickly, it can lead to serious issues.
Symptom | Description | Impact on Vision |
Blurred Vision | Lack of clarity in visual perception | Significant |
Floaters | Spots or specks in the field of vision | Moderate |
Sensitivity to Light | Increased discomfort from light exposure | Variable |
Unilateral vs. Bilateral Presentation
Panuveitis can hit one eye (unilateral) or both (bilateral). The cause and individual factors decide this. Knowing if it’s one or both eyes helps in choosing the right treatment.
Acute vs. Chronic Symptom Patterns
Panuveitis symptoms can be acute or chronic. Acute means sudden, while chronic means ongoing or coming back. Knowing the symptom pattern is key to managing it well.
It’s vital to watch how symptoms change and adjust treatments to help patients with panuveitis the most.
Potential Complications of Untreated Panuveitis
If panuveitis is not treated, it can cause serious problems. These issues can harm your vision and eye health. The inflammation can damage many parts of the eye, leading to secondary conditions.
Vision Loss and Blindness Risks
Untreated panuveitis can lead to vision loss. The inflammation can damage important eye structures. This can result in blindness if not treated quickly. Research shows that delayed treatment increases the risk of severe vision problems.
Secondary Glaucoma Development
Panuveitis can cause secondary glaucoma. This is when the pressure inside the eye goes up. This high pressure can harm the optic nerve, making vision worse. Treating glaucoma often needs medication or surgery.
Cataract Formation
Panuveitis can make cataracts form faster. Cataracts cloud the lens in the eye, causing blurry vision. They might need surgery. With panuveitis, surgery for cataracts can be more complicated.
Retinal and Optic Nerve Damage
Panuveitis can harm the retina and optic nerve. Damage to the retina can cause macular edema or retinal detachment. These can severely affect vision. Damage to the optic nerve can cause permanent vision loss. This highlights the need for quick and effective treatment.
In summary, untreated panuveitis can cause severe and lasting problems. It’s important to get a diagnosis and treatment early to avoid these issues and protect your vision.
Diagnostic Approach for Panuveitis
Diagnosing panuveitis is complex. It involves a detailed eye exam, lab tests, and imaging. Accurate diagnosis is key for effective treatment and preventing complications.
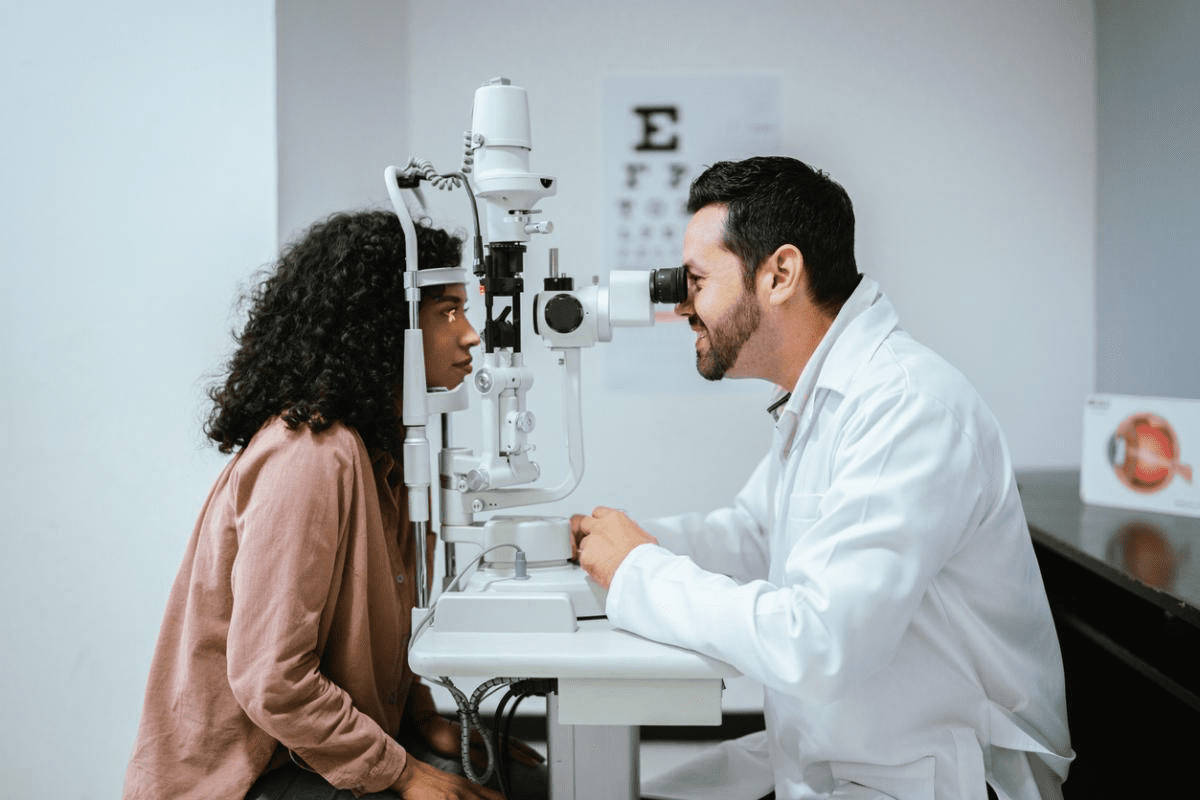
Comprehensive Eye Examination
A detailed eye exam is the first step. It includes:
- Visual acuity testing to check vision sharpness
- Slit-lamp exam to look at the eye’s front part
- Dilated fundus exam to check the eye’s back part
- Intraocular pressure test to check for glaucoma
These tests help spot inflammation and check the eye’s health.
Laboratory Testing
Labs are vital for finding panuveitis causes. We might do:
- Blood tests for infections or autoimmune issues
- Tests for specific antibodies or markers
- Chest X-rays or other studies to check for systemic diseases
These tests help us create a treatment plan that fits the patient’s needs.
Advanced Imaging Techniques
Advanced imaging is key for seeing inflammation and damage. Important imaging methods include:
Imaging Modality | Key Features | Clinical Utility |
Optical Coherence Tomography (OCT) | High-resolution imaging of retinal layers | Assesses retinal edema, detachment, and structural damage |
Fluorescein Angiography | Visualization of retinal vasculature | Identifies vascular leakage, ischemia, and neovascularization |
Ultrasonography | Evaluation of posterior segment when media opacity is present | Assesses for retinal detachment, vitreous hemorrhage, or posterior scleritis |
Differential Diagnosis Considerations
When diagnosing panuveitis, other conditions must be considered. These include:
- Other forms of uveitis (e.g., anterior, intermediate, or posterior uveitis)
- Retinal vasculitis
- Retinal detachment
- Vitreoretinal lymphoma
By considering these, we ensure an accurate diagnosis and proper treatment.
Treatment Options for Panuveitis
Managing panuveitis well means having a detailed treatment plan. It aims to cut down inflammation, ease symptoms, and stop vision loss. We’ll look at the different ways to treat it, like corticosteroids, immunosuppressants, biologic agents, and targeted therapies.
Corticosteroid Therapy Approaches
Corticosteroids are key in treating panuveitis because they fight inflammation well. They can be given in several ways, like eye drops, injections around the eye, injections into the eye, or taken by mouth.
- Topical Corticosteroids: Good for mild to moderate inflammation, applied directly to the eye.
- Periocular Injections: For more severe cases, injections around the eye provide focused treatment.
- Intravitreal Injections: Directly into the eye, for severe inflammation.
- Systemic Corticosteroids: Oral or IV, used for severe cases or when vision is at risk.
Immunosuppressive Medications
For those not helped by corticosteroids or needing ongoing treatment, immunosuppressants are used. These drugs calm down the immune system’s overactive response.
Medication Class | Examples | Use in Panuveitis |
Antimetabolites | Methotrexate, Azathioprine | Helps reduce inflammation |
Calcineurin Inhibitors | Cyclosporine, Tacrolimus | Reduces immune response |
Alkylating Agents | Cyclophosphamide | Used for severe, hard-to-treat cases |
Biologic Agents and Targeted Therapies
Biologic agents are a new type of treatment that targets specific parts of the immune system. They’re great for patients with tough or severe panuveitis.
“The advent of biologic therapies has revolutionized the treatment of uveitis, bringing new hope to patients with refractory disease.” –
A leading ophthalmologist
- TNF-alpha Inhibitors: Drugs like Adalimumab and Infliximab treat various uveitis types, including panuveitis.
- Interleukin Inhibitors: New therapies targeting interleukins, like IL-6 or IL-17, show promise.
Treating Underlying Systemic Conditions
Managing panuveitis often means finding and treating any underlying conditions that cause eye inflammation.
In conclusion, treating panuveitis involves many approaches, from corticosteroids to biologic agents. A treatment plan tailored to the patient’s specific needs is key to managing the condition effectively.
Managing Panuveitis Long-Term
Managing panuveitis long-term needs a detailed plan. This includes regular checks and changes to treatment plans. It’s key to control inflammation, avoid complications, and keep vision sharp.
Monitoring Disease Progression
Eye exams are vital to track panuveitis and see how treatment works. These exams check vision, look at the eye’s front part, and use imaging like OCT.
Key Components of Regular Eye Exams:
- Visual acuity tests to check vision sharpness
- Slit-lamp examination to look at the eye’s front part
- OCT imaging to see the retina and spot issues
Adjusting Treatment Protocols
Panuveitis changes, so treatment plans must too. This might mean changing medication doses, trying new treatments, or switching therapies.
Treatment Adjustment | Rationale |
Changing medication dosage | To get the best results and avoid side effects |
Switching to alternative therapies | When current treatments don’t work or cause problems |
Adding new treatments | To handle new issues or symptoms |
Managing Medication Side Effects
Long-term use of certain medications can cause side effects. It’s important to manage these to keep the patient’s quality of life good.
Common side effects include:
- Osteoporosis
- Weight gain
- Increased risk of infections
Preventing Recurrence
Stopping panuveitis from coming back is key. This means sticking to a treatment plan, going to follow-up visits, and watching for flare-ups early.
By being proactive and flexible, patients and doctors can work together. This helps achieve the best results and keeps vision intact.
Living with Panuveitis
Living with panuveitis means taking a few steps. You need medical treatment, lifestyle changes, and support from doctors and patient groups. It’s key to know how to handle this condition in your daily life.
Practical Lifestyle Adjustments
For those with panuveitis, making lifestyle changes is important. Wearing UV-protective sunglasses can help with light sensitivity. Using preservative-free artificial tears helps with dry eyes, a common issue.
Eating well and exercising regularly is good for your eyes. Stress management techniques like meditation or yoga can also help. They can lessen stress that makes symptoms worse.
Support Resources and Patient Communities
Support groups and online forums are key for coping with panuveitis. They offer a sense of community and advice. Online forums and social media groups for uveitis and panuveitis are great for connecting with others.
“Connecting with others who understand what you’re going through can be incredibly empowering. It helps you feel less isolated and more informed about your condition.”
Working with Your Healthcare Team
Managing panuveitis well needs teamwork with your healthcare team. Regular check-ups with your ophthalmologist are essential. Keeping a symptom journal helps track changes and find triggers.
Talking openly with your healthcare provider is also important. Share your experiences and challenges. This helps your team offer better support.
Emerging Research and Clinical Trials
Keeping up with new research and trials is vital. Medical research is always improving our understanding and treatments. Participating in clinical trials can give you access to new therapies.
Stay updated by following medical journals, attending conferences, or registering for trials. Knowing about new research helps you make better care choices.
Conclusion
Panuveitis is a serious eye condition that can harm your sight. It needs quick diagnosis and treatment. We’ve looked at what causes it, its symptoms, and how to treat it.
Starting treatment early can stop vision loss. Keeping up with care helps keep your eyes healthy. Knowing about panuveitis helps patients get help fast when they see symptoms.
Working with doctors, patients can find the best treatment for them. With the right care, people with panuveitis can avoid serious problems and keep their vision.
FAQ
What is panuveitis, and how does it differ from uveitis?
Panuveitis is a rare and serious eye condition. It affects all parts of the eye, unlike other uveitis types. This makes it harder to manage.
What are the common causes of panuveitis?
Panuveitis can be caused by many things. These include infections like toxoplasmosis and tuberculosis. Autoimmune conditions like sarcoidosis, eye injuries, and Vogt-Koyanagi-Harada syndrome are also causes.
What are the symptoms of panuveitis?
Symptoms include eye pain, redness, blurred vision, and floaters. It can affect one or both eyes. Symptoms can be sudden or last a long time.
What are the possible complications of untreated panuveitis?
Untreated panuveitis can cause serious problems. These include vision loss, blindness, and secondary glaucoma. It can also lead to cataracts and damage to the retina and optic nerve.
How is panuveitis diagnosed?
Diagnosing panuveitis involves a detailed eye exam. Lab tests and advanced imaging are used to find the cause and extent of inflammation.
What are the treatment options for panuveitis?
Treatment includes corticosteroids, immunosuppressants, and biologic agents. Managing any underlying conditions is also key to effective treatment.
How can panuveitis be managed long-term?
Long-term management involves regular check-ups and adjusting treatments as needed. Managing side effects and preventing recurrence are also important.
What lifestyle adjustments can help manage panuveitis symptoms?
Making lifestyle changes can help. This includes accessing support, working with healthcare teams, and staying updated on research. These steps can help manage symptoms.
What is the ICD-10 code for panuveitis?
The ICD-10 code is for billing and insurance. It’s important to talk to a healthcare professional to get the right code.
Is panuveitis associated with any genetic predispositions?
Research shows that genetics may play a role in panuveitis. Finding these genetic factors can help us understand the condition better.
References
National Center for Biotechnology Information. Panuveitis: Causes, Symptoms, and Treatment Options. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC2841373/