Last Updated on November 27, 2025 by Bilal Hasdemir
Knowing the difference between aortic stenosis and aortic regurgitation is key. At Liv Hospital, we focus on patient care. We use international standards to treat aortic valve disease.
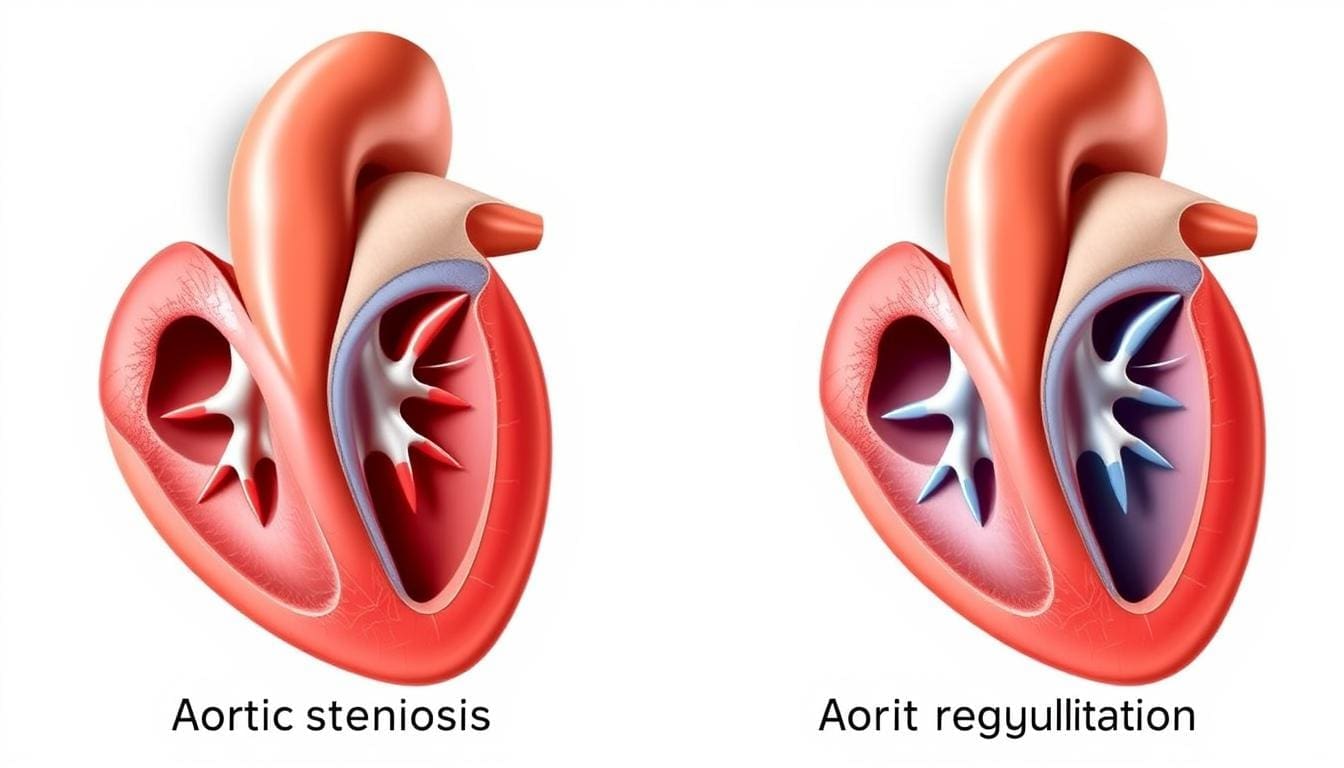
Aortic stenosis happens when the aortic valve gets too narrow. This blocks blood flow from the heart. On the other hand, aortic regurgitation occurs when the valve leaks. This lets blood flow back into the heart’s left ventricle.
We will look at the unique symptoms, how doctors diagnose them, and treatment choices for these issues.
Key Takeaways
- Understanding the differences between aortic stenosis and regurgitation is vital for proper diagnosis and treatment.
- Aortic stenosis involves the narrowing of the aortic valve, while regurgitation involves a leaky valve.
- Both conditions are types of heart valve disease requiring timely medical intervention.
- Symptoms and diagnostic approaches differ between the two conditions.
- Treatment options include surgical and minimally invasive procedures.
Overview of Aortic Valve Disease

Aortic valve disease includes many conditions that affect the valve’s function and heart health. We will look at the aortic valve’s anatomy and function. We will also discuss the different types of valvulopathies and their prevalence and demographics.
Anatomy and Function of the Aortic Valve
The aortic valve is key for blood flow from the heart to the aorta. It is made of three cusps that open and close with each heartbeat. This ensures blood flows right and prevents backflow.
Types of Aortic Valvulopathies
Aortic valvulopathies include aortic stenosis and aortic regurgitation. These happen due to age, congenital defects, or rheumatic heart disease. These conditions can cause the valve to narrow or leak.
Prevalence and Demographics
Aortic stenosis affects up to 4 percent of people over 75. This shows how common age-related calcification is. Knowing the demographics and prevalence helps in early diagnosis and treatment.
Aortic Stenosis: Pathophysiology and Causes

Aortic stenosis is a condition where the aortic valve narrows. This narrowing affects the heart’s function. It’s often caused by age-related calcification.
Definition and Mechanism of Valve Narrowing
Aortic stenosis happens when the aortic valve opening gets smaller. The valve leaflets thicken and calcify, making it hard for blood to flow. This blocks blood from moving from the left ventricle to the aorta.
Studies show that aortic stenosis is caused by genetics, environment, and lifestyle. Knowing these factors helps manage the condition better.
Age-Related Calcification
Calcification with age is a big reason for aortic stenosis, mainly in older people. Calcium builds up on the valve leaflets, making them stiff and narrow. This is common in those with high blood pressure and high cholesterol.
Congenital Bicuspid Valve Defects
Born with a bicuspid aortic valve? You’re at higher risk for aortic stenosis. The bicuspid valve is more likely to get calcified and narrow. This might need early treatment.
Rheumatic Heart Disease and Other Causes
Rheumatic heart disease used to cause a lot of aortic stenosis. But now, it’s less common in developed countries. Other causes include radiation and certain metabolic disorders. Knowing these causes helps doctors diagnose and treat aortic stenosis.
Aortic Regurgitation: Pathophysiology and Causes
When the aortic valve doesn’t close right, it causes aortic regurgitation. This is when blood flows back into the left ventricle. This backflow can lead to big changes in blood flow and can cause serious heart problems.
Definition and Mechanism of Valve Leakage
Aortic regurgitation happens when the aortic valve doesn’t close fully. This lets blood flow back into the left ventricle during diastole. This backflow can make the left ventricle bigger and put more pressure on it. Over time, this can cause the ventricle to change shape and not work right.
Primary valvular abnormalities are a big reason for aortic regurgitation. These can be things like a bicuspid aortic valve or damage from rheumatic heart disease.
Primary Valvular Abnormalities
Many things can cause primary valvular abnormalities leading to aortic regurgitation. For example, a bicuspid aortic valve is a birth defect that can cause regurgitation. Other causes include rheumatic fever and endocarditis, an infection of the valve.
Aortic Root Dilation and Aneurysms
Aortic regurgitation can also be caused by aortic root dilation or aneurysms. When the aortic root gets bigger, it can stop the valve from closing right. Marfan syndrome, a condition that affects connective tissue, can cause this dilation.
Infective Endocarditis and Other Causes
Infective endocarditis, an infection of the heart valves, is another reason for aortic regurgitation. The infection can damage the valve leaflets, causing leakage. Other causes include chest trauma and certain connective tissue disorders.
Knowing why aortic regurgitation happens is key to treating it. By figuring out the cause, doctors can make treatment plans that fit each patient’s needs.
Key Differences in Aortic Valve Disease Presentations
Aortic stenosis and regurgitation are two types of aortic valve disease. They have different symptoms and how they affect the heart. Both share some symptoms, but their causes and effects on the heart are unique.
Hemodynamic Effects and Blood Flow Patterns
Aortic stenosis narrows the aortic valve opening. This blocks blood flow from the left ventricle to the aorta. It makes the left ventricle work harder, leading to left ventricular hypertrophy.
Aortic regurgitation, on the other hand, lets blood flow back into the left ventricle. This increases the ventricle’s volume, potentially causing left ventricular dilation.
The blood flow in these conditions is different. Aortic stenosis has a high-velocity jet of blood through the narrowed valve. Aortic regurgitation has a regurgitant jet of blood flowing back into the left ventricle.
Cardiac Remodeling and Compensation Mechanisms
The heart changes in response to aortic stenosis and regurgitation. In aortic stenosis, the left ventricle gets thicker to handle the increased pressure. Over time, this can lead to diastolic dysfunction and heart failure.
In aortic regurgitation, the left ventricle gets bigger to hold more blood. This is a temporary fix but can lead to systolic dysfunction if not treated.
Natural History and Disease Progression
Aortic stenosis starts with no symptoms and gradually gets worse. The rate of worsening depends on factors like calcification and overall heart health.
Aortic regurgitation also gets worse over time. It can stay silent for years but becomes serious once symptoms appear or the heart starts to fail.
Knowing the differences in aortic stenosis and regurgitation is key for early diagnosis and treatment. Understanding their effects on the heart helps doctors provide better care for patients with aortic valve disease.
Clinical Presentation and Symptoms
The symptoms of aortic valve disease can be complex and overlapping. This makes diagnosis challenging. Both aortic stenosis and aortic regurgitation have symptoms that need careful evaluation.
Overlapping Symptoms: Breathlessness, Fatigue, and Chest Pain
Patients with either aortic stenosis or aortic regurgitation often report breathlessness, fatigue, and chest pain. These symptoms happen because the heart can’t meet the body’s needs due to the valvular dysfunction.
Breathlessness, or dyspnea, is a common symptom. It can happen during exertion or even at rest in severe cases. Fatigue is another frequent complaint, as the heart works harder to compensate for the valve issue. Chest pain, or angina, can occur due to increased demand for oxygen by the hypertrophied myocardium or reduced coronary flow.
Distinctive Features of Aortic Stenosis
Aortic stenosis has some distinctive features. Syncope, or sudden loss of consciousness, is a concerning symptom. It indicates a severe obstruction to outflow.
The classic symptoms of severe aortic stenosis are often remembered by the triad of dyspnea, angina, and syncope. The presence of these symptoms signifies a poor prognosis without valve replacement.
| Symptom | Description | Clinical Significance |
|---|---|---|
| Dyspnea | Breathlessness during exertion or at rest | Indicates heart failure or severe valve obstruction |
| Angina | Chest pain due to increased myocardial oxygen demand | Signifies ischemia; may indicate severe stenosis |
| Syncope | Sudden loss of consciousness | Indicates severe obstruction to outflow; poor prognosis without treatment |
Distinctive Features of Aortic Regurgitation
Aortic regurgitation presents with symptoms related to volume overload. Symptoms include palpitations and exertional dyspnea. Patients may also experience orthopnea and paroxysmal nocturnal dyspnea as the condition progresses.
The wide pulse pressure in aortic regurgitation can lead to various physical findings. These include a “water-hammer” pulse and pulsatile head or neck vessels. These signs are indicative of the severity of the regurgitation.
Diagnostic Approaches and Evaluation
To diagnose aortic valve disease, we use physical exams, imaging, and lab tests. These methods help us understand how severe the disease is. This information guides our treatment plans.
Physical Examination Findings and Heart Murmurs
A detailed physical exam is key in diagnosing aortic valve disease. We listen for specific heart murmurs. These sounds can show if and how badly the valve is affected.
The sound of the murmur can tell us a lot. A louder murmur often means the disease is more serious.
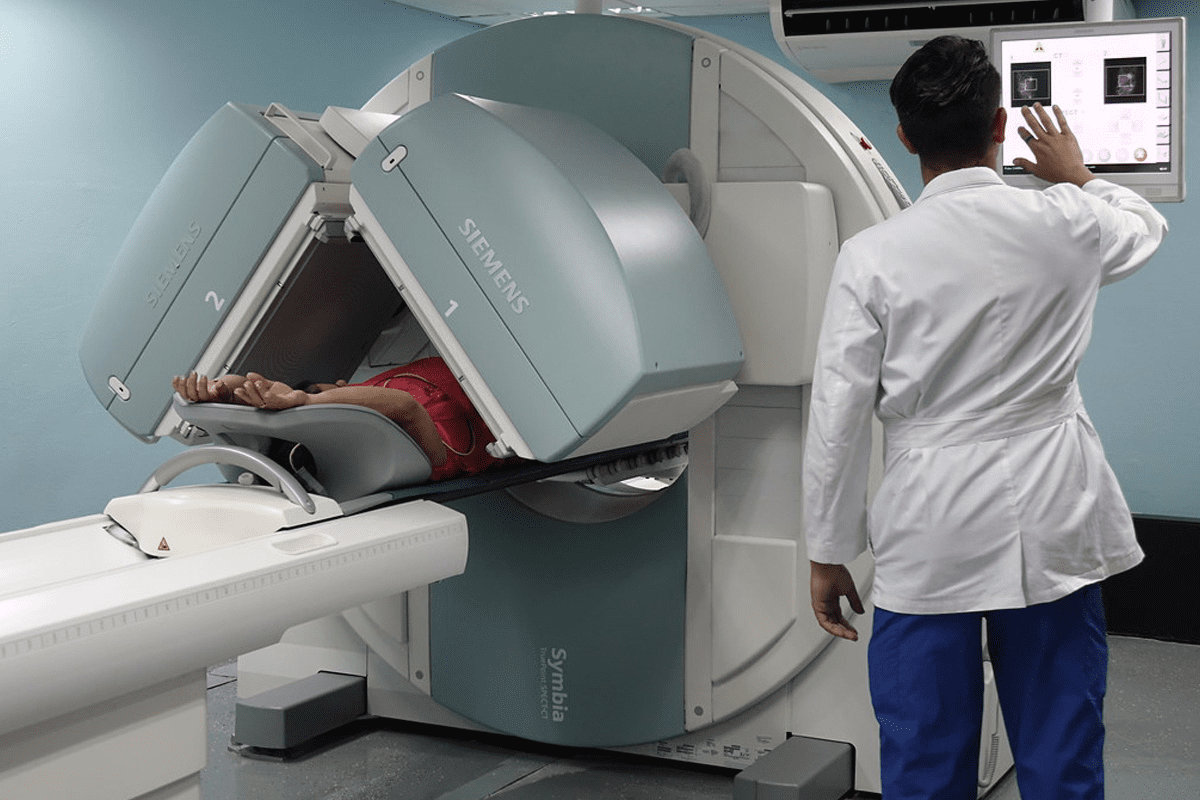
Echocardiography and Advanced Imaging
Echocardiography is a main tool for checking aortic valve disease. It lets us see the valve and how it works. We can also measure its size and check the heart’s function. Other imaging like MRI and CT scans give more details about the valve and the aorta.
These tests help us figure out how bad the disease is. They help us decide if surgery is needed.
Cardiac Catheterization and Hemodynamic Assessment
Cardiac catheterization is a detailed test that looks at the aortic valve’s function. It measures the pressure and flow across the valve. This helps us understand how severe the disease is.
This info is key for deciding if treatment is needed. It also helps us choose the right treatment, like minimally invasive procedures like TAVR.
Biomarkers and Laboratory Testing
Biomarkers and lab tests help us manage aortic valve disease. They help us track the disease’s progress and check the heart’s health. They also help spot any complications early.
| Diagnostic Tool | Information Provided | Clinical Utility |
|---|---|---|
| Echocardiography | Valve structure and function, left ventricular function | Assesses severity of valve disease, guides treatment decisions |
| Cardiac Catheterization | Hemodynamic data, pressures, and gradients across the valve | Evaluates need for intervention, plans treatment |
| Biomarkers (e.g., BNP) | Cardiac stress and function | Monitors disease progression, identifies possible complications |
By using these methods together, we can accurately diagnose and manage aortic valve disease. This approach improves patient care. The right tool depends on the patient’s specific situation and disease.
Treatment Options and Management Strategies
Managing aortic valve disease needs a detailed plan. We look at the disease type, symptoms, and health to choose the best treatment. This ensures the treatment fits the patient’s needs.
Medical Management and Monitoring
For mild or no symptoms, we start with monitoring. Regular check-ups and echocardiograms help track the disease. We also manage related health issues to ease heart strain.
Key aspects of medical management include:
- Regular monitoring of disease progression
- Management of related health conditions
- Lifestyle modifications to reduce cardiac risk factors
Surgical Valve Replacement and Repair
For severe disease or symptoms, surgery is needed. We choose between replacement or repair based on the valve condition. The patient’s health and age guide our decision.
The table below shows the differences between valve replacement and repair:
| Procedure | Description | Indications |
|---|---|---|
| Valve Replacement | Involves replacing the diseased valve with a prosthetic one | Severe valve disease, significant symptoms |
| Valve Repair | Involves repairing the native valve to restore function | Less severe valve disease, specific valve pathologies |
Transcatheter Aortic Valve Replacement (TAVR)
TAVR is a key option for severe aortic stenosis, mainly for those at high surgical risk. It’s a minimally invasive method that replaces the valve through a catheter. We consider TAVR for those not suited for traditional surgery.
- Minimally invasive approach, reducing recovery time
- Less risk of complications compared to open-heart surgery
- Effective for patients with severe aortic stenosis
Individualized Treatment Decision-Making
Treatment choices for aortic valve disease are tailored to each patient. We consider their specific factors, disease, and health. This ensures the treatment meets their unique needs.
Personalized treatment improves outcomes and quality of life for those with aortic valve disease.
Living with Aortic Valve Disorders: Prognosis and Quality of Life
It’s important to know how aortic valve disease affects people’s lives. This includes stenosis and regurgitation. These conditions can change daily life a lot. So, finding ways to improve their quality of life is key.
Risk Stratification and Monitoring
Managing aortic valve disease starts with risk stratification. We use different tools to figure out the risk of bad outcomes. This helps us decide the best treatment. Regular checks are also important to adjust treatment plans as needed.
When we assess risk, we look at several things:
- Symptom severity: We check how bad symptoms like breathlessness, chest pain, and fatigue are.
- Valve disease severity: We use echocardiography and other tests to see how bad the valve problem is.
- Comorbid conditions: We also consider other health issues that might affect the patient’s overall health.
Lifestyle Modifications and Activity Recommendations
Changing lifestyle is important for managing aortic valve disease. We suggest a heart-healthy diet, regular exercise, and quitting smoking. These steps help improve heart health and lower the risk of problems.
For those with aortic valve disease, it’s important to:
- Stay physically active: Do moderate exercise like walking, cycling, or swimming after talking to a doctor.
- Maintain a healthy weight: Eat right and exercise to keep a healthy weight.
- Manage stress: Use stress-reducing activities like meditation or deep breathing.
Long-term Outcomes and Survival Rates
The long-term outlook for aortic valve disease patients depends on several things. This includes how severe the disease is, any other health issues, and how well treatment works. With good care, many patients can live active and happy lives.
We stress the importance of:
- Regular follow-up: Keep up with doctor visits to monitor the condition and adjust treatment if needed.
- Adherence to treatment: Stick to the treatment plan, including medication and lifestyle changes.
- Patient education: Teach patients about their condition, treatment options, and the importance of self-care.
Understanding the prognosis and quality of life for aortic valve disease patients helps us give better care. We focus on their unique needs to improve their well-being.
Conclusion
It’s important to know the difference between aortic stenosis and aortic regurgitation. We’ve looked at how they affect the heart and how to treat them.
Aortic stenosis and regurgitation are two different heart valve diseases. Each needs its own treatment plan. Finding and treating these conditions early is key to managing them well.
The main difference is in how they affect the heart. Stenosis narrows the valve, while regurgitation lets blood leak back. Knowing this helps doctors create better treatment plans for patients.
We’ve covered the main points about aortic valve disease. Our goal is to help you understand these conditions better. This knowledge can lead to better care for those with heart valve disease.
FAQ
What is aortic valve disease?
Aortic valve disease refers to conditions affecting the aortic valve. This includes aortic stenosis and regurgitation. These conditions impact the valve’s ability to regulate blood flow from the heart.
What are the main differences between aortic stenosis and aortic regurgitation?
Aortic stenosis is when the aortic valve narrows, blocking blood flow. Aortic regurgitation is when the valve leaks, causing blood to flow back into the heart’s left ventricle.
What causes aortic stenosis?
Aortic stenosis can be caused by age-related calcification, congenital bicuspid valve defects, and rheumatic heart disease. These factors contribute to the narrowing of the aortic valve.
What are the symptoms of aortic stenosis and regurgitation?
Symptoms include breathlessness, fatigue, and chest pain. The specific characteristics and severity of these symptoms vary between the two conditions.
How is aortic valve disease diagnosed?
Diagnosis involves a thorough approach. This includes physical examination, imaging studies like echocardiography, cardiac catheterization, and laboratory tests. These help evaluate the condition and severity of the aortic valve disease.
What are the treatment options for aortic valve disease?
Treatment options include medical management and monitoring. Surgical interventions like valve replacement and repair are also available. Transcatheter aortic valve replacement (TAVR) is an option for eligible patients.
How is the severity of aortic valve disease determined?
Diagnostic tests like echocardiography and cardiac catheterization assess the valve’s function. They determine the impact on the heart, helping to determine severity.
Can lifestyle modifications help manage aortic valve disease?
Yes, lifestyle modifications and activity recommendations are key. They can improve quality of life and potentially influence long-term outcomes.
What is the prognosis for patients with aortic stenosis and regurgitation?
The prognosis varies based on the condition’s severity, treatment effectiveness, and individual factors. Ongoing monitoring and management are critical for optimizing outcomes.
What is transcatheter aortic valve replacement (TAVR)?
TAVR is a minimally invasive procedure for treating aortic stenosis. It’s used for patients at high risk for surgical complications. The procedure involves replacing the aortic valve with a prosthetic one.
References
NCBI Bookshelf (National Library of Medicine): Valvular Heart Disease (Specific NCBI ID)
Cardioflow Medtech: Aortic Stenosis (Patient Information)