Last Updated on December 3, 2025 by
We are seeing a big change in how children die from cancer. Brain cancer is now the deadliest form of childhood cancer, beating out leukemia. According to the U.S. CDC, almost one in three kids who die from cancer have brain cancer. This shift highlights the answer to the question, what is the most deadly form of cancer in children today, with brain cancer surpassing leukemia due to advances in leukemia treatment and the ongoing challenges in effectively treating brain tumors.

This change comes from better treatments for leukemia, which have greatly increased survival chances. But, brain cancer is hard to treat because of its complex nature and the blood-brain barrier. This barrier makes it hard for treatments to reach the brain.
Key Takeaways
- Brain cancer is now the deadliest form of childhood cancer.
- Nearly one in three childhood cancer deaths are due to brain cancer.
- Advances in leukemia treatment have improved survival rates.
- Brain cancer treatment is challenging due to its complex nature.
- The blood-brain barrier hinders effective treatment delivery for brain cancer.
The Current State of Childhood Cancer
Childhood cancer has seen progress in treatment and survival rates. It’s a big worry because it affects young lives. We’ll look at the latest numbers and how it’s different from adult cancers.

erroneous image
Annual Incidence and Mortality Statistics
In the U.S., about 14,910 kids and teens get cancer each year. The top cancers are leukemia, brain tumors, and others. From 1999 to 2014, cancer deaths in kids fell by 20 percent.
This shows how far medicine has come. The numbers show we need more research and better treatments. Leukemia is the most common, followed by brain tumors and lymphomas. Knowing this helps us find better ways to treat it.
How Childhood Cancers Differ from Adult Cancers
Childhood cancers are different from adult ones in many ways. Kids get more leukemias, brain tumors, and sarcomas. The causes and how they respond to treatment are also unique.
It’s important to understand these differences. Treating childhood cancer needs a team effort. We must keep learning and improving to help kids live better lives.
Brain Cancer: Now the Deadliest Form of Childhood Cancer
Brain cancer has become the deadliest form of childhood cancer, surpassing leukemia. This change is alarming and needs our attention. We must understand the reasons behind this shift.
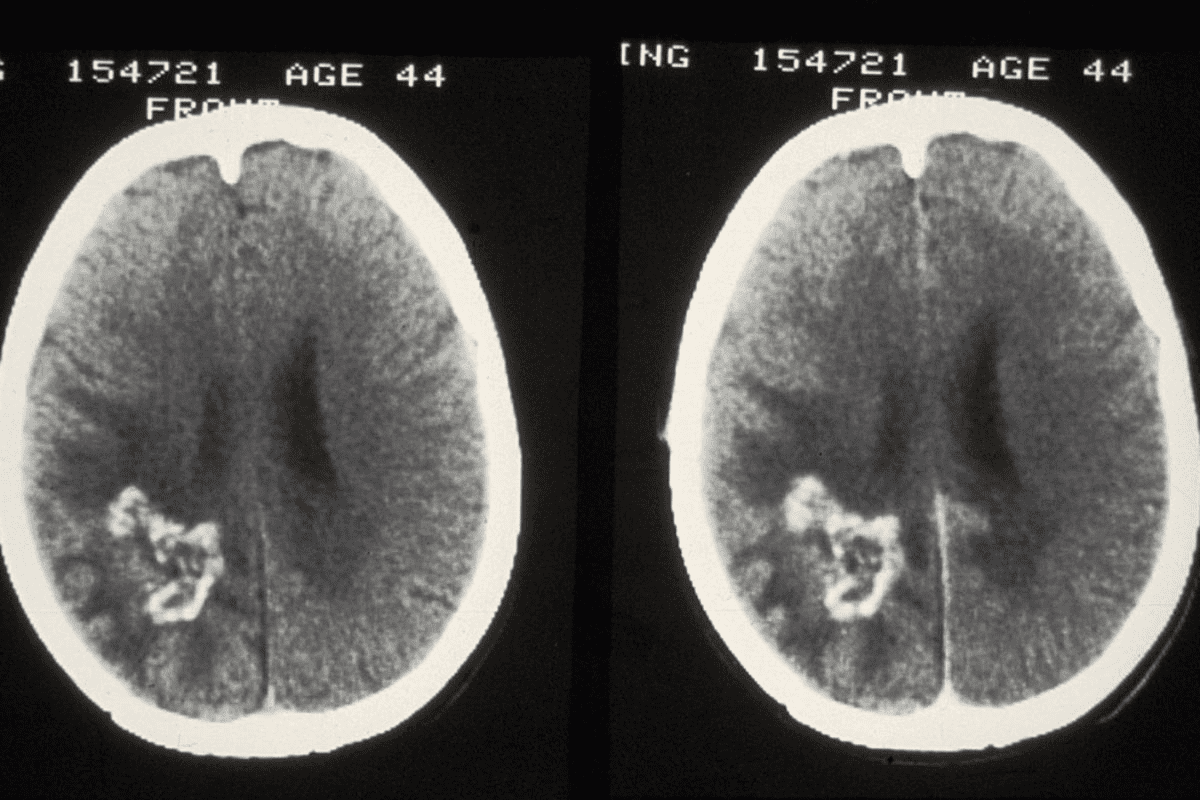
Statistical Evidence of Brain Cancer Mortality
The Centers for Disease Control and Prevention (CDC) reports a rise in brain cancer deaths among children. From 516 in 1999 to 534 in 2014, the numbers show an increase. Now, nearly one in three childhood cancer deaths are due to brain cancer.
This data is clear. Brain cancer is a major cause of childhood cancer deaths. We need more awareness and better treatments.
Key statistics include:
- Nearly one in three childhood cancer deaths are due to brain cancer.
- Brain cancer deaths among children rose from 516 in 1999 to 534 in 2014.
- Brain cancer is now the leading cause of cancer-related deaths in children.
Why Brain Cancer Has Surpassed Leukemia
Several factors have led to brain cancer becoming the deadliest form of childhood cancer. The complexity of brain cancer and the challenges in treating it are key. Brain cancer is often diagnosed late, making treatment harder.
The blood-brain barrier also plays a role. It’s a barrier that keeps toxins out but also blocks many treatments. This barrier makes it hard to reach brain tumors with effective treatments.
The reasons behind this shift are multifaceted and involve:
- The complexity of brain cancer.
- Challenges in treating brain cancer due to its location and the blood-brain barrier.
- Advances in treatment for other forms of childhood cancer, such as leukemia.
What is the most deadly form of cancer in children: Types of Brain Tumors
Brain tumors are a wide range of cancers, but some are more deadly in kids. Knowing about these types is key to finding better treatments and helping young patients.
High-Grade Gliomas and Their Mortality Rates
High-grade gliomas are very aggressive brain tumors in children. They grow fast and are hard to treat because of their location and how they spread. Mortality rates for high-grade gliomas remain high, even with new treatments.
Studies on high-grade gliomas show they have complex molecular profiles. This affects how they grow and respond to treatment. Targeted therapies are being looked into to help patients with these tough tumors.
Diffuse Intrinsic Pontine Glioma (DIPG)
DIPG is a very tough brain cancer that mainly hits kids. It’s responsible for almost a quarter of all cancer deaths in young people. This makes it one of the deadliest types of cancer in this age group.
Professor Matt Dun’s research on DIPG has been a big step in understanding and possibly treating it. His work shows the need for more research and new treatments for DIPG.
Medulloblastoma and Other Aggressive Brain Tumors
Medulloblastoma is a very aggressive brain tumor that mostly affects kids. It starts in the cerebellum and can spread to other brain parts and the spinal cord. Treatment usually includes surgery, chemotherapy, and radiation therapy.
Other aggressive brain tumors in kids include:
- Ependymomas, which start in the ependymal cells lining the ventricles and central canal of the spinal cord.
- Primitive neuroectodermal tumors (PNETs), which are very malignant tumors that can occur in different brain parts.
- Atypical teratoid/rhabdoid tumors (ATRTs), which are rare but very aggressive tumors that usually affect young kids.
It’s important to know about these tumors’ characteristics and mortality rates. This helps in creating effective treatment plans and improving survival rates for kids with these deadliest forms of cancer.
Leukemia: Historical Context and Current Status
Leukemia has been the top childhood cancer for a long time. But, its status as the deadliest has changed. It’s now the most common childhood cancer, making up about 25% of new cases. We’ll look at its history, how treatments have improved, and today’s death rates to understand its current role in childhood cancers.
Historical Dominance of Leukemia
Leukemia was once the main killer among childhood cancers. Several reasons made it the top killer:
- The high number of acute lymphoblastic leukemia (ALL) cases in kids.
- Little was known about the disease and treatments were not effective.
- Old diagnostic tools meant late diagnosis and treatment.
Advances in Treatment
Big steps forward in treatment have greatly boosted survival chances for kids with leukemia. These include:
- New combination chemotherapy regimens.
- Better ways to figure out who needs what treatment.
- Improvements in care that help kids survive treatment better.
The CDC reports a drop in leukemia deaths in kids. From 445 in 1999 to 316 in 2014, showing the effect of these changes.
Current Mortality Statistics
Even with these improvements, leukemia is a big killer in kids. Survival rates have gone up, but there’s more to do. We keep watching death rates and aim to lower them even more.
erroneous image
Knowing about leukemia’s history, treatment progress, and today’s death rates helps us tackle this common childhood cancer. We must keep improving to help kids with leukemia live better lives.
The Blood-Brain Barrier: Why Brain Cancers Are Harder to Treat
The blood-brain barrier is a complex structure that makes treating brain cancers tough. It protects the brain from harmful substances but blocks treatments from reaching tumors.
Understanding the Blood-Brain Barrier
The blood-brain barrier is a membrane that keeps the brain safe from the bloodstream. It’s made of cells that tightly control what can enter the brain. This barrier is vital for brain health but makes treating brain tumors hard.
Studies have found that the blood-brain barrier is a big problem for brain cancer treatment. It’s a major hurdle for high-grade gliomas and other aggressive tumors. This barrier makes it hard for chemotherapy to reach the tumor effectively.
Treatment Delivery Challenges
Getting treatments to brain tumors is tough because of the blood-brain barrier. Chemotherapy, which works well for other cancers, doesn’t work as well for brain cancers. This limits treatment options and makes outcomes poor.
The barrier also makes it hard to use other treatments like targeted therapy and immunotherapy. These treatments might not work as well or be harder to deliver because of the barrier.
Current Approaches to Overcome the Blood-Brain Barrier
Scientists are working on ways to get past the blood-brain barrier to help brain cancer patients. They’re looking at novel delivery systems like nanoparticles to carry treatments into the brain.
Another method is using focused ultrasound to open the barrier temporarily. This lets treatments reach the tumor. Early trials show promise, giving hope to brain cancer patients.
By understanding the blood-brain barrier, we can find better ways to treat brain cancer. This could lead to better outcomes for patients.
Warning Signs and Early Detection of Deadly Childhood Cancers
Spotting cancer symptoms early can greatly improve treatment chances. We’re looking at the deadliest childhood cancers and their warning signs. It’s key to know these signs to catch these diseases early.
Brain Cancer Symptoms in Children
Brain cancer in kids shows in many ways, some subtle, others clear. Common signs include:
- persistent headaches
- nausea and vomiting, often in the morning
- seizures
- weakness or numbness in arms or legs
- changes in personality or behavior
- trouble with balance or coordination
Parents and caregivers must watch for these symptoms. Early spotting can greatly help treatment success.
Leukemia Warning Signs
Leukemia, a common childhood cancer, has its own signs. These include:
- persistent fatigue or weakness
- frequent infections
- easy bruising or bleeding
- pale skin
- swollen lymph nodes or spleen
Spotting these signs early is key to timely medical help. This is vital for better survival chances.
When to Seek Medical Attention
If a child shows any of these symptoms, get medical help fast. These signs can mean different things, not just cancer. A full medical check is needed to find out what’s wrong.
We stress the need to be active in your child’s health. If worried about symptoms, talk to a doctor. Early action and treatment are vital for kids with cancer.
Other Significant Childhood Cancers and Their Mortality Rates
Leukemia and brain cancer are the deadliest in kids. But, cancers like neuroblastoma, lymphomas, and bone and soft tissue sarcomas also kill many children. These cancers are less common but very dangerous and need careful treatment.
Neuroblastoma
Neuroblastoma starts in the adrenal glands, neck, chest, or spinal cord. It’s most found in kids under five. High-risk neuroblastoma has a low survival rate, depending on the tumor’s stage and type.
It’s key to find it early and treat it hard. Doctors use surgery, chemo, radiation, and immunotherapy to fight it.
Lymphomas
Lymphomas are cancers of the lymphatic system. They’re common in kids. Hodgkin lymphoma is more common in teens and young adults, while non-Hodgkin lymphoma can happen at any age.
Doctors treat lymphomas with chemo and sometimes radiation. The outcome depends on the type and stage of the disease.
Bone and Soft Tissue Sarcomas
Bone and soft tissue sarcomas are rare but deadly in kids. Osteosarcoma and Ewing’s sarcoma are common bone sarcomas. Rhabdomyosarcoma is a common soft tissue sarcoma.
Treatment includes surgery, chemo, and radiation. The chance of survival depends on the type, stage, and how well it responds to treatment.
Global Disparities in Childhood Cancer Outcomes
Childhood cancer outcomes differ greatly around the world. Each year, about 400,000 new cases are reported globally. Survival rates range from over 80% in rich countries to less than 30% in poorer ones.
80% vs. 30%: The Survival Gap Between High and Low-Income Countries
The survival rate gap between rich and poor countries is alarming. Rich countries have better medical tech, early detection, and care. Poor countries face limited healthcare, delayed diagnosis, and poor treatment options.
Key factors contributing to the survival gap include:
- Limited access to healthcare facilities and specialists in low-income countries
- Delayed diagnosis due to lack of awareness and limited screening programs
- Inadequate treatment protocols and lack of access to essential medicines
- Socioeconomic factors affecting families’ ability to seek and continue treatment
Access to Diagnosis and Treatment Barriers
Several barriers block access to timely diagnosis and treatment in poor countries. These include:
- Economic constraints: Cancer treatment is too expensive for many families.
- Lack of infrastructure: Poor healthcare setup, lacking in equipment and staff.
- Cultural beliefs and misinformation: Misunderstandings about cancer can cause delays in seeking help.
International Initiatives to Improve Global Outcomes
Many global efforts aim to bridge these gaps. These include:
- Collaborations between rich and poor countries to share knowledge and resources
- Programs to enhance healthcare infrastructure and train staff
- Efforts to make medicines and treatments more affordable
- Efforts to raise awareness about childhood cancer symptoms
By tackling these disparities, we can help more children with cancer worldwide.
Conclusion: Future Directions in Fighting Deadly Childhood Cancers
We’ve looked into the deadliest childhood cancers and seen big strides in treatment. The five-year survival rate is now 80 percent. But, we have a lot more to do, mainly with brain cancer and other tough cancers.
Brain tumors and some leukemias are the toughest to treat. Research and new treatments have helped a lot. But, we need more research and teamwork to keep improving.
By understanding these cancers better and working together, we can help more kids beat cancer. We aim for a future where every child can survive and live a full life.
FAQ
What is the deadliest form of childhood cancer?
Why has brain cancer become the leading cause of death among childhood cancers?
What are the most common types of childhood cancer?
What makes brain cancer so challenging to treat?
What are the most aggressive forms of brain tumors in children?
How have advances in leukemia treatment impacted its mortality rates?
What are the warning signs of brain cancer and leukemia in children?
Are there global disparities in childhood cancer outcomes?
What international initiatives are aimed at improving global outcomes for childhood cancer?
What is the current focus for future research and treatment in childhood cancer?
References
- Kim, H.-J., et al. (2022). Suggestions for escaping the dark ages for pediatric diffuse intrinsic pontine glioma research. PMC, 13, 470.