
Hematopoietic stem cells (HSCs) are key to our blood health. They are mainly found in the red bone marrow of adults. This includes areas like the pelvis, femur, and sternum. These cells are vital for making all types of blood cells, keeping us healthy.
Research on HSCs is moving forward fast. Places like Liv Hospital are using new treatments, like AVM Biotechnology Inc.’s AVM0703. This drug helps grow HSCs. It’s being tested in trials for blood cancers and solid tumors, showing how important HSCs are for health care.
Key Takeaways
- Hematopoietic stem cells are mainly found in the red bone marrow of adults.
- Locations such as the pelvis, femur, and sternum are key areas where HSCs reside.
- HSCs are vital for producing all types of blood cells throughout life.
- Research on HSCs is leading to innovative treatments for blood cancers and solid tumors.
- AVM Biotechnology Inc.’s drug AVM0703 is stimulating HSC production in clinical trials.
The Fundamental Nature of Hematopoietic Stem Cells
Hematopoietic stem cells (HSCs) are key to our blood system. They can grow themselves and turn into different blood cells. This keeps our blood cell count steady throughout our lives.
Definition and Basic Properties
Hematopoietic stem cells are special cells that make all blood cell types. They can self-renew and differentiate into many blood cell types. This is important for making new blood cells all the time.
A famous hematologist, says, “HSCs are the base of the hematopoietic system. They provide a lifelong supply of blood cells through their unique ability to balance self-renewal and differentiation.”
“The ability of HSCs to self-renew and differentiate is not only vital for normal blood cell production but also holds the key to understanding various blood disorders.”
Self-Renewal and Multipotency Characteristics
The self-renewal of HSCs keeps their numbers stable. This is key for long-term blood cell production. Also, HSCs are multipotent, which means they can turn into all blood cell types, including myeloid and lymphoid lineages.
- Self-renewal: The ability to maintain the HSC population.
- Multipotency: The capacity to give rise to all blood cell types.
- Differentiation: The process by which HSCs become specialized blood cells.
Research on AVM0703 has shown promising results. It reactivates the body’s Reserve Immune System and boosts HSC production. This shows the great promise of understanding and working with HSCs for treatments.
Where in the Body Are Hematopoietic Stem Cells Found
To understand HSCs, we need to know where they live in our bodies. They are not spread out randomly. Instead, they are in specific places that help them do their job well.
Primary Locations in Adult Bone Marrow
In adults, HSCs mainly live in the bone marrow, in the spongy parts of bones. The bone marrow has a special environment that helps HSCs grow and change into different blood cells. The main bones where this happens are:
- The pelvis
- The femur (thigh bone)
- The sternum (breastbone)
These bones have red marrow, which is full of blood vessels and cells. The bone marrow’s structure, with its network of blood vessels and cells, is key for keeping HSCs healthy.
Secondary Locations and Circulation
Besides the bone marrow, HSCs can also be found in smaller numbers in other places. These include:
- The spleen
- Lymph nodes
- Peripheral blood
HSCs can move through the blood, helping them spread out in the body. This movement is important for keeping a balance of HSCs and for responding to the body’s needs for blood cells.
Quantitative Distribution Across Anatomical Sites
Research shows that HSCs make up about 1 in 10,000 cells in the bone marrow. How many HSCs are in different bones and organs can change. This depends on things like age, health, and the body’s needs.
| Anatomical Site | HSC Concentration |
|---|---|
| Bone Marrow | 1 in 10,000 nucleated cells |
| Peripheral Blood | Much lower than bone marrow |
| Spleen | Variable, generally lower than bone marrow |
Knowing where HSCs are in the body is important for research and for treatments like stem cell transplants.
The Bone Marrow Microenvironment: HSC’s Primary Home
In the bone marrow, hematopoietic stem cells live in a special area. This area helps them grow and change into different blood cells. It’s key for keeping the balance between growing more HSCs and turning into blood cells.
Structure and Components of the Bone Marrow Niche
The bone marrow niche has many parts that work together. Key components include osteoblasts, endothelial cells, and growth factors. These parts help make a good place for HSCs to live and work.
Key Anatomical Locations: Pelvis, Femur, and Sternum
In adults, the main places for making blood are the pelvis, femur, and sternum. These bones have lots of bone marrow with HSCs. The pelvis is very important because it has a lot of marrow.
Cellular Interactions Supporting HSC Function
Inside the bone marrow, cells talk to each other to help HSCs. Osteoblasts make things that help HSCs grow. Endothelial cells help HSCs stay in the right place. This talking between cells keeps HSCs healthy.
Studies show that things like AVM0703 can help make more HSCs. This shows how important the bone marrow is for HSCs. Knowing how these cells talk to each other helps us find new ways to help HSCs.
Developmental Journey of Hematopoietic Stem Cells
The journey of hematopoietic stem cells from the start to their home in the bone marrow is complex. Their travel through different parts of the body is key to setting up a working blood system.
Embryonic Origins in the Aorta-Gonad-Mesonephros Region
In the third week of gestation, the first hematopoietic stem cells appear. They start in the aorta-gonad-mesonephros (AGM) region. This area is important for the first HSCs that will fill other blood-making spots.
“The AGM region is considered a critical site for the emergence of definitive hematopoietic stem cells capable of long-term reconstitution of the hematopoietic system.”
”
Yolk Sac and Fetal Liver as Temporary Residences
After starting in the AGM, HSCs move to the yolk sac and then the fetal liver. The yolk sac is the first place for blood cell making. The fetal liver is where HSCs grow and change into different blood cells during fetal growth.
- The yolk sac supports primitive hematopoiesis.
- The fetal liver is key for making definitive blood cells.
Migration to Bone Marrow During Late Development
As they grow, HSCs move to their final home: the bone marrow. This move is vital. The bone marrow has a special environment that helps HSCs stay healthy and work well for the rest of our lives.
The bone marrow environment is vital for HSCs to keep making more cells. This ensures we always have enough blood cells.
HSC Populations Across Different Age Groups
Hematopoietic stem cells (HSCs) change a lot from birth to old age. They affect our health and how we fight off diseases. Knowing how HSCs change is key to understanding their role in our bodies.
Neonatal and Pediatric HSC Distribution
In babies and kids, HSCs are more common and spread out in different places. Studies have shown they’re not just in the bone marrow but also in the liver and spleen early on. This helps support their fast growth and development.
As kids get older, HSCs move mostly to the bone marrow. The main places are the pelvis, femur, and sternum. The bone marrow microenvironment is key in helping HSCs work well during this time.
Changes in HSC Location and Function During Aging
As we age, HSCs change a lot. They start to have more of the same cells, which can weaken our immune system. This also raises the risk of blood cancers.
The bone marrow also changes with age. It gets more reactive oxygen species (ROS) and inflammation. This can hurt how well HSCs can renew themselves and develop into different blood cells.
Age-Related Decline in HSC Function
As we get older, HSCs don’t work as well. Studies have demonstrated they don’t move as well, can’t renew themselves as much, and tend to become more myeloid cells. This is a big problem for our health.
It’s important to understand why HSCs decline with age. This knowledge can help us find ways to improve blood cell production in older people. It can also help in creating new treatments for blood diseases.
The Remarkable Production Capacity of HSCs
Hematopoietic stem cells (HSCs) are key to making billions of blood cells every day. This is essential for our survival. The human body makes over 500 billion blood cells daily, thanks to these amazing cells.
Daily Blood Cell Production Statistics
The average adult makes more than 500 billion blood cells daily. This shows how hardworking HSCs are. Their work is vital for keeping our blood cell count up. This helps our body get oxygen and fight off infections.
Lifespan and Regenerative Capacity
HSCs can keep making blood cells for our whole lives. Studies on AVM0703 show it can help HSCs work better. This shows how good they are at regenerating.
Balancing Self-Renewal and Differentiation
HSCs are great at balancing two important things. They can keep themselves going (self-renewal) and make different types of blood cells (differentiation). This balance is key to keeping our blood healthy and our body working right.
In short, HSCs are very important for our health. They make billions of blood cells every day. Their ability to keep regenerating and balance their work is vital for our well-being.
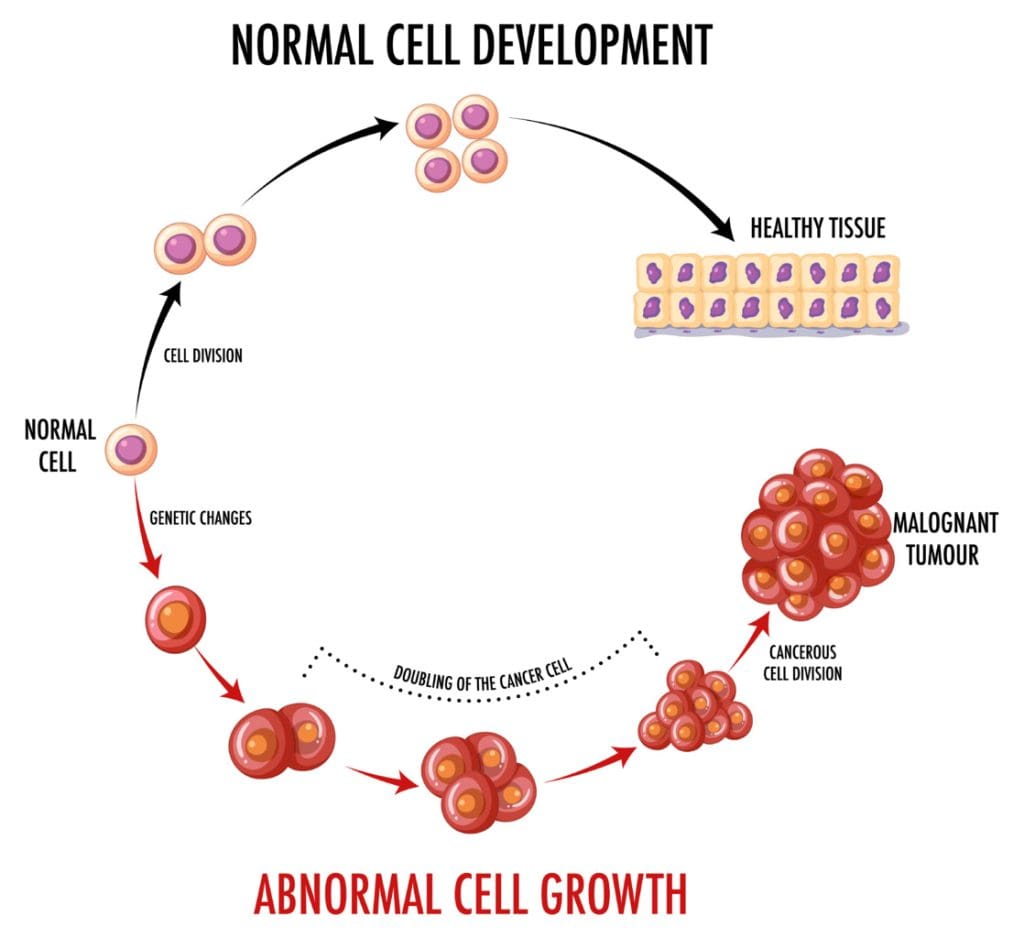
From Stem Cell to Specialized Blood Cell: The Differentiation Pathway
The journey of hematopoietic stem cells (HSCs) is complex and multi-step. It leads to the creation of different blood cells. These cells are mainly found in the bone marrow, which is inside bones like the hips and thighbones.
We will explore how HSCs turn into various blood cell types. This process is key for keeping our blood cell count right and our health good.
Myeloid Lineage Development
The myeloid lineage produces red blood cells, platelets, and some white blood cells. This process is controlled by growth factors and transcription factors.
For example, erythropoietin, made by the kidneys, helps make red blood cells. Granulocyte-colony stimulating factor (G-CSF) helps make neutrophils.
Lymphoid Lineage Development
The lymphoid lineage makes lymphocytes, like T cells, B cells, and natural killer cells. These cells are vital for fighting infections and diseases.
Many factors, including interleukins and specific transcription factors, influence lymphoid development. For instance, PAX5 is key for B cell development.
Regulation of Lineage Commitment
Choosing between the myeloid or lymphoid lineage is a precise process. Signaling pathways and transcription factors work together to keep the right balance of blood cells.
Understanding how HSCs decide their lineage is important for treating blood disorders. It helps in finding new treatments for imbalances in blood cell production.
In summary, the journey of hematopoietic stem cells is complex and vital for blood cell production. By understanding how HSCs become specialized blood cells, we can learn more about blood production. This knowledge helps in developing new treatments for blood-related issues.
Molecular Regulation of Hematopoietic Stem Cell Function
The way hematopoietic stem cells work is very complex. It involves many signaling pathways and transcription factors. These elements help keep HSCs in check, ensuring they function correctly. Hematopoietic stem cells (HSCs) are key to making all blood cell types. If they don’t work right, it can cause blood disorders.
Key Signaling Pathways Controlling HSC Behavior
Many signaling pathways are important for HSCs. The Wnt/β-catenin pathway helps with self-renewal and differentiation. The Notch signaling pathway keeps HSCs from differentiating too early. The PI3K/AKT pathway is vital for their survival and growth.
These pathways work together in a complex way. For example, research on AVM0703 shows tweaking these pathways can boost HSC activity. This could lead to new treatments.
Transcription Factors in HSC Maintenance
Transcription factors are key for controlling gene expression in HSCs. Important ones include RUNX1, GATA2, and HOXB4. They help keep HSCs in check and manage their self-renewal and differentiation.
Getting these transcription factors right is critical. If not, HSCs might exhaust themselves or turn cancerous. This shows how vital they are for blood cell production.
Environmental Factors Affecting HSC Activity
The bone marrow environment is vital for HSCs. Things like oxygen levels, cell interactions, and growth factors affect their behavior. The endosteal niche, in particular, is thought to support HSCs.
Learning about these environmental factors can help us find new ways to improve HSC function. This could lead to better treatments or transplant outcomes.
Clinical Applications: Hematopoietic Stem Cell Transplantation
Hematopoietic stem cells have opened new ways to treat serious diseases. Hematopoietic stem cell transplantation (HSCT) is a key treatment for many blood cancers, genetic disorders, and autoimmune diseases. We will look at the different types of HSCT, their uses, and the diseases they treat.
Autologous vs. Allogeneic Transplantation
There are two main types of HSCT: autologous and allogeneic. Autologous transplantation uses the patient’s own stem cells. These cells are collected, stored, and then given back after treatment. This method lowers the risk of graft-versus-host disease (GVHD) but might increase the chance of disease coming back.
Allogeneic transplantation uses stem cells from a donor. This method can help fight cancer cells better. But, it can cause GVHD and needs careful matching between donor and recipient to avoid problems.
Treatment of Blood Cancers
HSCT is a key treatment for blood cancers like leukemia, lymphoma, and multiple myeloma. The choice between autologous and allogeneic depends on the disease type, stage, and the patient’s health. It also depends on finding a suitable donor.
For example, allogeneic HSCT is often used for acute leukemias because it can fight leukemia well. Autologous HSCT is sometimes chosen for lymphoma and multiple myeloma.
Addressing Immune and Genetic Disorders
HSCT is also used for severe immune deficiencies and some genetic disorders. For instance, allogeneic HSCT can cure severe combined immunodeficiency (SCID) by giving a healthy immune system.
HSCT is also being studied for autoimmune diseases. The goal is to reset the immune system and stop disease progression. Research, like AVM0703 by AVM Biotechnology Inc., is ongoing to see if HSCT is safe and effective for these diseases.
We see the importance of HSCT in treating patients. As research grows, we expect more breakthroughs in hematopoietic stem cell transplantation.
Harvesting and Processing Hematopoietic Stem Cells
Getting hematopoietic stem cells (HSCs) right is key. New ways to get and prepare HSCs are helping more patients. This is a big step forward in saving lives.
Bone Marrow Aspiration Techniques
Bone marrow aspiration is a common way to get HSCs. It takes bone marrow from the pelvic bone or sometimes the sternum or femur. Special needles are used to get the marrow, which is then cleaned to find HSCs.
This method is good because it can get a lot of HSCs at once.
The steps are:
- Getting the patient ready with anesthesia
- Putting a needle into the bone marrow
- Getting the marrow into a syringe
- Cleaning the aspirate to find HSCs
Peripheral Blood Stem Cell Collection
Collecting HSCs from the blood is becoming more popular. It’s less invasive than bone marrow aspiration. Growth factors are used to move HSCs into the blood. Then, apheresis collects these cells.
This method is getting better, making it a top choice for many.
The steps are:
- Using G-CSF to move HSCs into the blood
- Apheresis to separate and collect HSCs
- Freezing the collected HSCs for later use
Umbilical Cord Blood as an HSC Source
Umbilical cord blood is a great source of HSCs. It’s perfect for patients who can’t find a donor. We collect cord blood right after birth, process it, and freeze it for later use.
Cryopreservation and Storage Methods
Cryopreservation is key for storing HSCs long-term. It freezes the cells to stop all activity, so they can be stored for a long time. We use the latest methods to keep HSCs alive when they’re thawed.
The steps for cryopreservation are:
- Adding cryoprotectants to protect cells from ice damage
- Freezing slowly to reduce damage
- Storing in liquid nitrogen at -196 °C
By using these advanced methods, we can give patients the best HSCs for their transplant. This improves their chances of recovery.
Current Research Frontiers in HSC Science
Research on hematopoietic stem cells (HSCs) is growing fast. It’s helping us understand these cells better and find new uses for them in healthcare. This research is opening up new ways to treat many diseases.
Expanding HSC Applications Beyond Blood Disorders
HSCs have long been used to treat blood-related problems. But now, scientists are looking into using them for other diseases too. For example, they might help with autoimmune diseases like multiple sclerosis and type 1 diabetes by fixing the immune system.
AVM0703, a new treatment, is showing great results in clinical trials. It helps move HSCs around the body, which could make them even more useful in treating diseases.
“The versatility of HSCs in regenerative medicine is becoming increasingly evident, opening new hopes for patients with many serious conditions.”
Gene Therapy and Genetic Engineering of HSCs
Gene therapy with HSCs is also making big strides. Scientists are changing HSCs’ genes to fix inherited diseases. This could lead to lasting cures for conditions like sickle cell anemia and beta-thalassemia.
CRISPR/Cas9 technology is making it easier to edit genes with precision. This is a big step forward in this field.
- Correcting genetic mutations in HSCs to treat inherited blood disorders
- Enhancing the immune system’s ability to fight cancer through genetically modified HSCs
- Developing novel gene therapies for previously untreatable conditions
Artificial HSC Production Efforts
Creating artificial HSCs is a new area of research. Scientists are working on making HSCs from induced pluripotent stem cells (iPSCs) or by changing other cells directly. This could give us more HSCs for transplants, solving problems like finding donors and avoiding immune rejection.
| Method | Advantages | Challenges |
|---|---|---|
| iPSC-derived HSCs | Potential for unlimited supply, reduced immune rejection | Risk of tumor formation, efficiency of differentiation |
| Direct Reprogramming | Bypasses need for pluripotency, potentially safer | Efficiency, stability of reprogrammed cells |
HSCs in Regenerative Medicine
HSCs are also being looked at for regrowing tissues, not just blood. They might help fix damaged hearts and livers. Their ability to help repair tissues through chemical signals is very interesting.
As we learn more about HSCs, we’ll see big improvements in treating many diseases. The future of HSC science is very promising for better patient care and quality of life.
Conclusion
Hematopoietic stem cells are vital for making all blood cell types. Knowing where they are in the body is key to understanding their role. They mainly live in the bone marrow, helping keep blood cell levels balanced.
The bone marrow environment helps HSCs work well. They can renew themselves and turn into different blood cells. Studies, like AVM0703, show how important HSCs are for health and future treatments.
To learn more about HSCs, check out the latest research and clinical uses. For example, Liv Hospital’s resource on short-term hematopoietic stem cells offers insights into HSCs.
In summary, HSCs are essential for blood cell production and have great promise for treating blood disorders and other diseases. Their main location in the bone marrow is vital for their function and use in medicine.
Where are hematopoietic stem cells (HSCs) mainly found in the body?
HSCs are mostly in the bone marrow. They are most concentrated in the pelvis, femur, and sternum.
What are the secondary locations of hematopoietic stem cells?
HSCs also live in smaller amounts in the peripheral blood and organs like the spleen and liver.
How do hematopoietic stem cells circulate in the body?
HSCs move through the blood. This lets them travel between different parts of the body, like from the bone marrow to other tissues.
What is the role of the bone marrow microenvironment in supporting HSCs?
The bone marrow microenvironment helps HSCs a lot. It does this through cell interactions and signals that keep HSCs working right and control their actions.
How do hematopoietic stem cells develop and migrate during embryonic development?
HSCs start in the aorta-gonad-mesonephros area during early development. Then, they move to the yolk sac, fetal liver, and end up in the bone marrow.
How do HSC populations change across different age groups?
HSCs change a lot with age. Their numbers and how they work change from babies to adults and the elderly.
What is the production capacity of hematopoietic stem cells?
HSCs can make billions of blood cells every day. They balance making new cells and keeping their own numbers to help make blood cells for life.
How do hematopoietic stem cells differentiate into specialized blood cells?
HSCs turn into different blood cells through specific paths. Certain genes and signals guide them to become different types of blood cells.
What are the clinical applications of hematopoietic stem cell transplantation?
HSC transplantation helps treat blood cancers, immune problems, and genetic diseases. It can be from the patient themselves or from someone else.
How are hematopoietic stem cells harvested and processed for transplantation?
HSCs are taken out through bone marrow aspiration or blood collection. They can also come from umbilical cord blood. Then, they are prepared and frozen for later use.
What are the current research frontiers in HSC science?
Researchers are working on new uses for HSCs, gene therapy, making HSCs in the lab, and their role in fixing damaged tissues. They aim to find better treatments for many diseases.
What is the significance of understanding hematopoietic stem cell biology?
Knowing about HSCs is key for making good treatments for blood diseases. It also helps in regenerative medicine. So, more research in this area is very important.
References
- Wikipedia contributors. (2025). Hematopoietic stem cell. Wikipedia. Retrieved October 11, 2025, from https://en.wikipedia.org/wiki/Hematopoietic_stem_cell Wikipedia
- (n.d.). PMC6526542. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6526542/




































