Knowing about the cervix anatomy is key for women’s health and medical care. The cervix is a part of the uterus that links the vagina to it. It’s about 4 centimeters long and 3 centimeters wide. Where is the cervix located? Get the ultimate, simple answer. This essential guide explains its vital function and place in your anatomy.
It’s the lower part of the uterus, forming a narrow passage. This passage connects the vagina to the uterine cavity. At Liv Hospital, we focus on top-notch care for cervical health. We use the latest medical knowledge to help women get the best care.
Key Takeaways
- The cervix is a vital part of the female reproductive system.
- Knowing its anatomy is key for good diagnosis and treatment.
- The cervix acts as a bridge between the outside and inside reproductive areas.
- Liv Hospital offers detailed cervical health checks.
- We follow international and academic standards for the best results.
The Cervix: Definition and Basic Functions
The cervix is a key part of the female reproductive system. It plays a vital role in women’s health. It is different from the uterus and has many important functions.
What Is the Cervix?
The cervix is the lower, narrow part of the uterus. It opens into the vagina. It is a complex structure that is different from the rest of the uterus.
Key Functions in Reproductive Health
The cervix has two main roles in reproductive health. It lets sperm into the uterus and keeps infections out. When a woman ovulates, the cervical mucus becomes thinner. This makes it easier for sperm to enter.
The cervix has two parts: the endocervix and the ectocervix. The endocervix is the inner part that lines the cervical canal. The ectocervix is the outer part that sticks out into the vagina.
The cervix is very important for reproductive health. It controls the flow of sperm and keeps the upper genital tract clean. Its work is closely tied to the menstrual cycle and overall reproductive health.
It’s important to understand the cervix and its role in fertility and reproductive health. The cervix changes its mucus properties throughout the menstrual cycle. This helps or blocks sperm entry as needed.
Where Is the Cervix Located?
The cervix is at the bottom of the uterus, linking the uterine cavity to the vagina. Knowing where it is in the female body helps us see its importance in health.
Position Within the Female Reproductive System
The cervix is part of the female body, connecting the uterus to the vagina. It sticks out into the vagina from the uterus’s bottom. This spot makes it key for health, like in menstruation, fertility, and pregnancy.
Relationship to Surrounding Organs
The cervix is near other important organs in the pelvic area. It’s between the bladder and the bowel. The ureters, which carry urine, are on the sides of the cervix. Knowing this helps us understand its role and importance.
Organ/Structure | Relation to Cervix | Significance |
Bladder | Anterior to the cervix | Close proximity can be relevant in surgical procedures |
Bowel | Posterior to the cervix | Important for understanding possible health issues |
Ureters | Lateral to the cervix | Critical for avoiding damage during surgeries |
Understanding the cervix’s location and its ties to other organs helps us see its role in the female body. It’s vital for health and in medical situations.
Physical Characteristics and Dimensions
The cervix is a key part of the female body. It has unique features that help it do its job. Knowing about these features is important for understanding reproductive health.
Average Size and Measurements
The cervix has specific sizes that are considered normal. It is about 4 centimeters long and has a 3-centimeter diameter. This means it’s roughly 1.6 inches long and sticks out about 0.8 inches into the vagina. These sizes can vary a bit, but they usually stay the same.
Measurement | Average Value | Range |
Length | 4 cm | 3.5 – 4.5 cm |
Diameter | 3 cm | 2.5 – 3.5 cm |
Projection into Vagina | 2 cm | 1.5 – 2.5 cm |
Normal Appearance and Variations
The cervix looks different in everyone. It’s usually shaped like a cylinder or cone with a small opening. Its look can change because of hormones and health issues.
Its look can change for many reasons. Age, if you’ve had a baby, and hormones can all play a part. For example, a woman who has had a baby vaginally might see a different cervix than one who hasn’t.
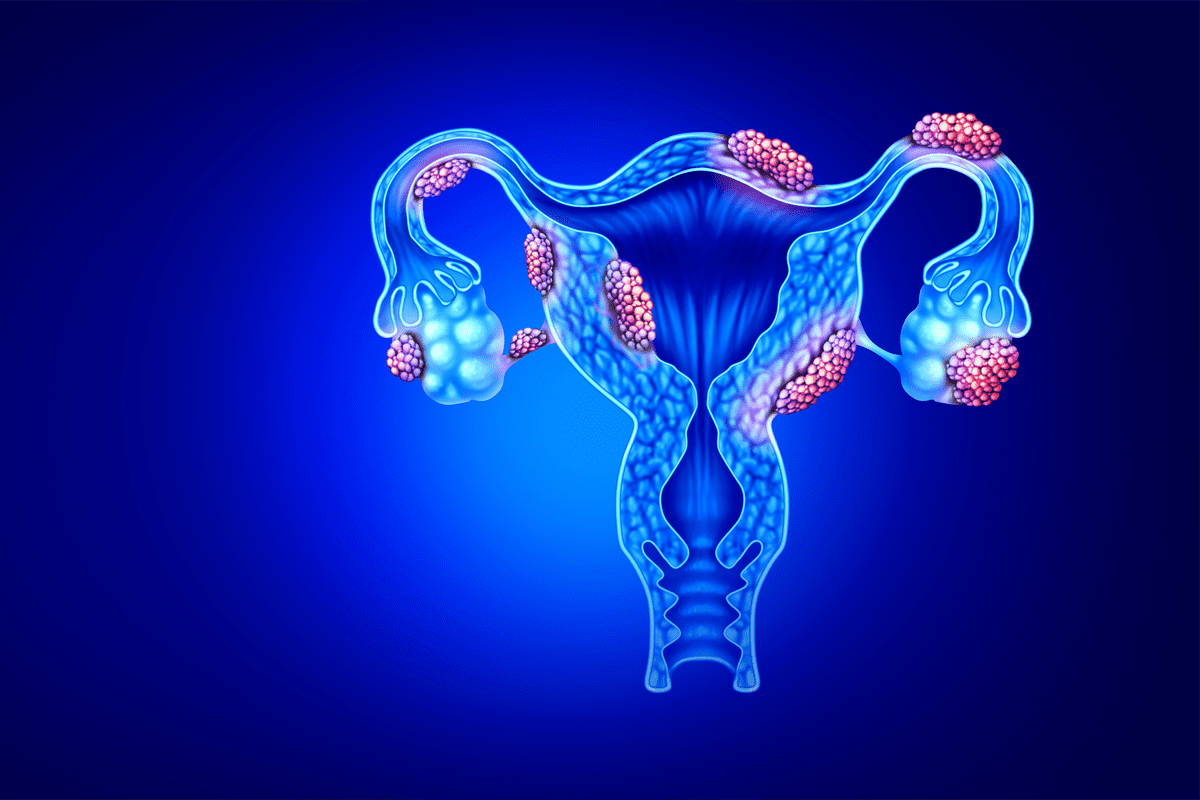
Anatomical Regions of the Cervix
It’s important to know the parts of the cervix to understand its role in health. The cervix has different areas, each with its own job. These parts are key to women’s health.
The Endocervix: Structure and Features
The endocervix is the inside of the cervix, lining the cervical canal. It has mucus-secreting simple columnar epithelium. This helps in reproductive processes by controlling sperm passage.
The Ectocervix: Structure and Features
The ectocervix is the outer part of the cervix, sticking into the vagina. It’s covered by non-keratinized stratified squamous epithelium. This protects it from the vagina. It’s seen during exams and is key for cancer checks.
The Internal Os
The internal os is the cervical canal’s opening into the uterus. It’s a key spot that separates the cervix from the uterus. It helps keep the pregnancy safe by staying closed until labor starts.
The cervix’s different parts work together for health. Knowing about them helps doctors and patients understand its complex role.
Microscopic Anatomy: Cervical Epithelium
The microscopic details of the cervical epithelium are key to its health. The cervix has two main types of epithelium. These are the endocervical glandular epithelium and the ectocervical squamous epithelium.
Endocervical Glandular Epithelium
The endocervical canal is covered by a single layer of simple columnar epithelium. This epithelium is vital for making mucus. The mucus helps sperm move during ovulation and protects against infections.
- The endocervical glandular epithelium is made up of tall, columnar cells.
- These cells have basal nuclei and are rich in mucin.
- The mucus changes in consistency throughout the menstrual cycle.
Ectocervical Squamous Epithelium
The ectocervix, on the other hand, is covered by non-keratinized stratified squamous epithelium. This multi-layered epithelium guards against mechanical and microbial threats.
- The ectocervical squamous epithelium is several layers thick.
- It lacks keratinization, unlike skin epithelium.
- This type of epithelium is more likely to undergo metaplastic changes.
It’s important to understand the differences between these epithelium types. Their roles in health and disease are significant. The squamocolumnar junction, where these types meet, is critical in cervical pathology.
The Squamocolumnar Junction (SCJ)
The SCJ is where two types of cells meet in the cervix. It’s important for health. Here, the squamous cells of the outer cervix meet the columnar cells of the inside.
Definition and Anatomical Location
The SCJ is where squamous and columnar cells come together. It’s found at the cervix’s opening. This spot changes with age and hormones.
Transformation Zone
The transformation zone (TZ) is around the SCJ. Here, columnar cells turn into squamous cells. This area is where most cervical cancers start.
The TZ has young cells that can easily change and become cancerous. Knowing about the TZ helps doctors understand cervical screening results and manage health issues.
Clinical Significance in Cervical Pathology
The SCJ and TZ are very important for cervical health. Most cervical cancers start in these areas.
Clinical Aspect | Significance |
Cervical Cancer Screening | The SCJ and TZ are key areas examined during cervical screening to detect pre-cancerous and cancerous changes. |
Cervical Pathology | Understanding the SCJ and TZ helps in diagnosing and managing cervical lesions and neoplasia. |
Colposcopy | A procedure used to closely examine the cervix, vagina, and vulva for signs of disease, particularl focusing on the SCJ and TZ. |
We know how important the squamocolumnar junction is in healthcare. It’s key for doctors to understand it for cervical cancer screening and care.
Cervical Stroma: Composition and Function
Cervical stroma is key to the cervix’s strength. It’s made of collagen and elastin fibers. These fibers help the cervix handle changes well.
Fibromuscular Tissue Structure
The cervical stroma is mostly fibromuscular tissue. It’s packed with collagen and elastic fibers. This makes the cervix firm and strong.
The collagen and elastin are vital. They keep the cervix strong. This is important for supporting the uterus and handling pregnancy and labor.
Medical experts say, “The cervix is densely fibrous and more rigid than other uterine tissue, with a thick layer of collagen and elastic fibers.” This makes it special and important.
Functional Role in Cervical Support
The cervical stroma supports the cervix. It keeps it in place and shape. This is key for a healthy pregnancy.
The stroma’s role is big. It helps the cervix stay strong and healthy. Its mix of fibers gives it the right amount of flexibility and strength.
Changes During Pregnancy and Labor
During pregnancy, the stroma changes a lot. The fibers in it soften and dilate the cervix. This is important for a vaginal delivery.
As pregnancy goes on, the cervix starts to open up. This is because of the stroma’s changes. It’s a big step for labor and the baby’s birth.
“The remodeling of the cervical stroma during pregnancy is a complex process involving significant changes in the composition and structure of the cervix, enabling it to accommodate the demands of labor.”
Vascular and Nervous Supply
It’s important to know how the cervix gets its blood and nerve supply. The cervix is a key part of the female body. It needs a network of blood vessels and nerve endings to work right.
Blood Supply to the Cervix
The uterine artery, a branch of the internal iliac artery, mainly feeds the cervix. This blood supply is key for the cervix’s health. It brings oxygen and nutrients. The uterine venous plexus helps take away blood that’s not full of oxygen.
The cervix’s blood vessels help it stay healthy. They support its role in reproductive health. This includes changes during the menstrual cycle and when a woman is pregnant.
Nerve Endings in the Cervix
The cervix has nerve endings that connect to the autonomic nervous system. These nerves are important for sending signals. They help control the cervix’s functions.
The nerve endings in the cervix are very sensitive. They help the cervix work well with the rest of the reproductive system. Knowing about these nerves is key to understanding the cervix’s health and how it reacts to different situations.
In summary, the blood and nerve supply to the cervix is complex. It’s vital for the cervix’s functions. By understanding this, we can see how important the cervix is for reproductive health and its responses to different situations.
Physiological Changes Throughout Life
The cervix changes a lot from puberty to postmenopause. These changes are key to understanding its role in women’s health. They show how the cervix adapts and changes over time.
Developmental Changes from Puberty
Puberty brings big changes to the cervix. Hormonal shifts in adolescence change its structure and function. The cervix starts making different kinds of mucus, which is vital for reproductive health.
Cyclical Changes During Menstruation
The cervix changes with the menstrual cycle. During ovulation, the mucus is alkaline, helping sperm. At other times, the mucus thickens, blocking sperm entry.
Cervical Adaptations During Pregnancy
In pregnancy, the cervix stays closed and the mucus thickens. This plug protects the fetus from infection. As pregnancy goes on, the cervix softens and gets ready for labor.
Postmenopausal Changes
After menopause, the cervix changes again. Estrogen levels drop, making the cervical canal narrower and mucus production less. These changes are part of aging and hormonal decline.
Knowing about these changes helps us understand the cervix’s role in women’s health. It shows how it adapts and changes over a woman’s life. This knowledge helps healthcare providers manage and treat cervix-related issues.
Clinical Significance of Cervical Anatomy
Knowing the cervix’s anatomy is key to understanding its role in women’s health. It’s important for reproductive functions and cancer screening.
Importance in Cervical Cancer Screening
The cervix is key for cancer screening because of the squamocolumnar junction (SCJ). This area is at high risk for cancer. Regular Pap smears and HPV tests help find cancer early.
The American Cancer Society says, “Cervical cancer is highly preventable with proper screening and vaccination against HPV.” Thanks to screening, cervical cancer deaths have dropped a lot.
Screening Method | Frequency | Benefits |
Pap Smear | Every 3 years | Detects precancerous cells |
HPV Testing | Every 5 years | Identifies high-risk HPV strains |
Co-testing (Pap + HPV) | Every 5 years | Combines benefits of both tests |
Role in Fertility and Conception
The cervix helps with fertility by changing its mucus to help or block sperm. Knowing how it changes can help plan for conception.
Cervical mucus is important for those trying to conceive. It shows when you’re most fertile. When you’re ovulating, the mucus is clear and helps sperm move.
Relevance to Common Gynecological Procedures
Cervical anatomy is important for many gynecological procedures. This includes colposcopy, cervical biopsy, and LEEP. Knowing the anatomy helps doctors do these procedures safely and well.
- Colposcopy: A procedure to closely examine the cervix, vagina, and vulva for signs of disease.
- Cervical Biopsy: Removing a sample of cervical tissue for pathological examination.
- LEEP: A procedure to remove abnormal cells from the cervix using a heated loop of wire.
In conclusion, the cervix’s anatomy is very important. It affects cancer screening, fertility, and many gynecological procedures. Doctors need to understand it well to give the best care to their patients.
Conclusion
Understanding the cervix and its anatomy is key to knowing its role in health. We’ve looked at what the cervix is, where it is, and its parts. We’ve also seen how it changes throughout life.
The cervix is very important for women’s health. Knowing about it helps doctors do their jobs better. It’s also important for checking for cervical cancer.
Knowing about the cervix helps doctors diagnose and treat problems. We’ve seen how it changes during pregnancy. Its anatomy is also important for medical treatments.
In short, the cervix is a complex and vital part of women’s health. Understanding it helps doctors give better care. This means patients get better medical decisions.
FAQ
What is the cervix and where is it located?
The cervix is the lower, narrow part of the uterus. It opens into the vagina. It’s found at the vagina’s top, near the bladder and rectum.
What are the main functions of the cervix in reproductive health?
The cervix lets sperm in but keeps the uterus sterile. It also changes its mucus to help or block sperm entry.
What is the anatomy of the cervix?
The cervix has three parts: the endocervix, ectocervix, and internal os. The endocervix connects the uterus to the vagina. The ectocervix projects into the vagina.
What is the squamocolumnar junction (SCJ) and why is it important?
The SCJ is where the ectocervix meets the endocervix. It’s key for understanding cervical health, like in cancer screening.
How does the cervix change during pregnancy?
During pregnancy, the cervix softens, dilates, and effaces. This prepares it for childbirth.
What is the role of the cervical stroma?
The cervical stroma is fibromuscular tissue. It supports the cervix and is vital for its structure and function.
How does the cervix change during the menstrual cycle?
The cervix’s mucus changes throughout the cycle. It becomes more sperm-friendly during ovulation.
What is the blood supply to the cervix?
The cervix gets its blood from the cervical branches of the uterine arteries.
What are the nerve endings in the cervix?
The cervix has nerve endings that feel stretch and pressure. This can cause pain during labor or procedures.
How does the cervix change after menopause?
After menopause, the cervix may shrink and become less noticeable. The cervical canal also narrows.
Why is understanding cervical anatomy important for healthcare providers?
Knowing cervical anatomy helps healthcare providers. It’s key for reproductive health, diagnosing issues, and performing gynecological procedures.
References
World Health Organization. Cervix Anatomy: Location and Dimensions. Retrieved from https://www.who.int/news-room/fact-sheets/detail/cervical-cancer