Last Updated on November 25, 2025 by Ugurkan Demir
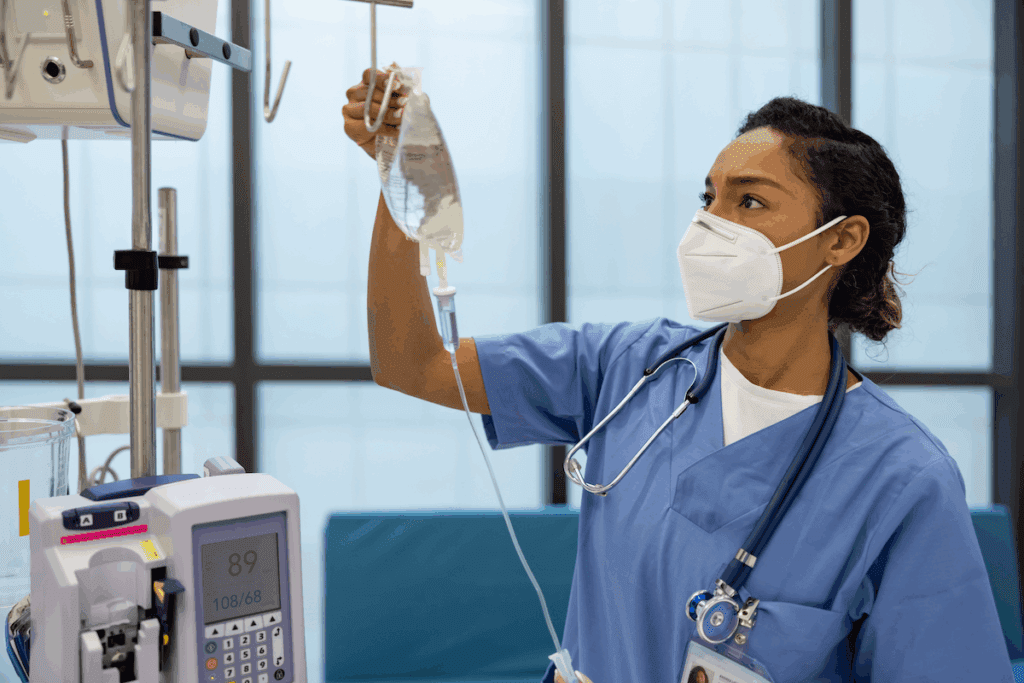
Arterial calcification is a serious health issue that can point to bigger problems. At Liv Hospital, we take it seriously and treat it with care. Arterial calcification is linked to atherosclerosis, chronic kidney disease, and diabetes mellitus.Learn which disorder would cause calcification of the arteries and how this condition affects your cardiovascular health.
Conditions like chronic kidney disease and diabetes mellitus play a big role in vascular calcification. We aim to give full care, tackling the root causes. We support patients with complex vascular diseases too.
Key Takeaways
- Arterial calcification is linked to serious underlying health conditions.
- Chronic kidney disease and diabetes mellitus are significant contributors to vascular calcification.
- A patient-centered approach is key in managing arterial calcification.
- LivHospital offers expert care for complex vascular diseases.
- Comprehensive support is available for international patients seeking advanced medical treatments.
Understanding Arterial Calcification
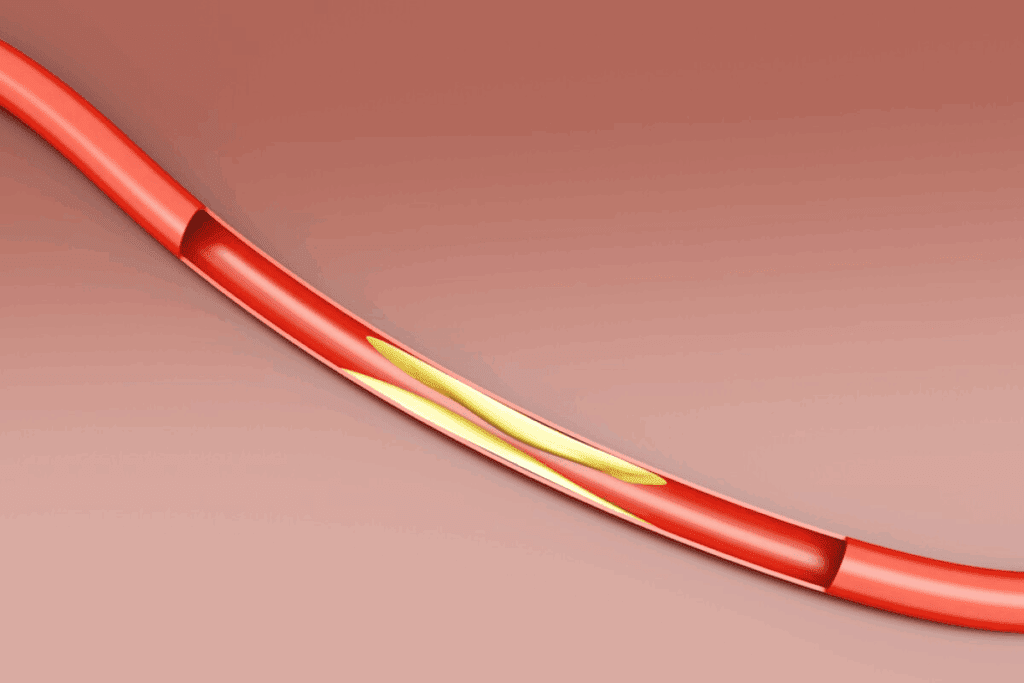
Arterial calcification is when calcium builds up in artery walls. It’s linked to heart diseases and can cause serious health issues. We’ll look into what it is, how it happens, and its types.
Definition and Pathophysiology
Calcification in arteries means calcium and phosphate minerals build up. It’s not just a simple buildup. It involves many cell and molecular actions. Active calcification processes are controlled by things like inflammation and growth factors.
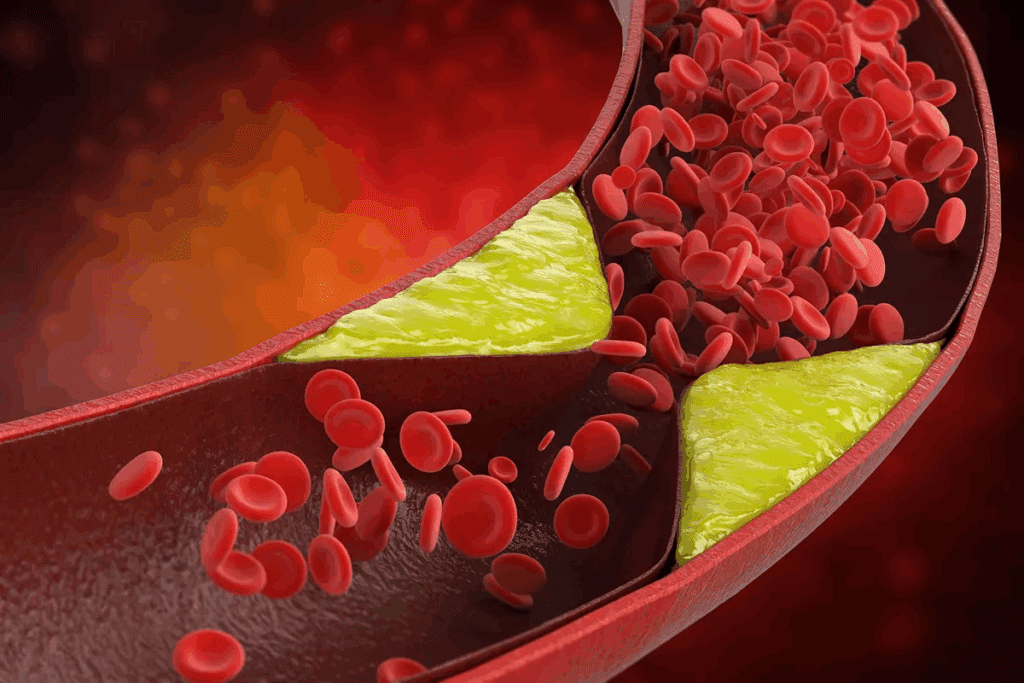
The process changes smooth muscle cells into cells that help calcium build up. This change is caused by high phosphate levels, stress, and inflammation. Knowing how it works helps us find ways to treat it.
Types of Vascular Calcification
Vascular calcification can be split into two main types. These are based on where and how the calcification happens. The types are intimal and medial calcification.
| Type of Calcification | Characteristics | Clinical Implications |
| Intimal Calcification | Occurs in the intimal layer of arteries, often associated with atherosclerosis. | Linked to plaque instability and increased risk of cardiovascular events. |
| Medial Calcification | Affects the medial layer, common in patients with diabetes and chronic kidney disease. | Results in arterial stiffness, contributing to systolic hypertension and cardiac workload. |
Knowing the type of calcification is key to understanding its effects and treating it. We’ll keep exploring why and how often arterial calcification happens next.
The Prevalence of Arterial Calcification
It’s important to know how common arterial calcification is. This condition affects many people around the world. We’ll look at how age and gender play a role.
Age-Related Statistics
Arterial calcification gets more common as people get older. It’s found in about 30% of younger people and over 80% of older adults. This depends on who is studied and how they are tested.
A study in a well-known medical journal showed:
- Arterial calcification is rare in people under 40, affecting 10-20%.
- Between 40-60 years, it affects about 40-50% of people.
- Over 60, it affects 70-90% of people.
Gender Differences in Calcification Rates
There are also differences in who gets arterial calcification. Men tend to get it more than women, mostly at younger ages.
A study combining several research papers found:
- Men under 60 get arterial calcification more often than women of the same age.
- As people get older, the difference between men and women narrows. Some studies suggest women may catch up with men after menopause.
“The gender difference in arterial calcification prevalence may be attributed to various factors, including hormonal influences and lifestyle factors.”
Knowing these differences helps us create better prevention and treatment plans.
Which Disorder Would Cause Calcification of the Arteries?
It’s important to know which disorders cause arteries to harden. Arterial calcification happens when calcium and phosphate build up in artery walls. This makes the arteries stiff and hard.
We’ll look at the different disorders that cause this problem. We’ll talk about primary and secondary causes. Primary causes are genetic or inherited. Secondary causes are things we get or do that increase the risk.
Primary vs. Secondary Causes
Primary causes include rare genetic disorders like Generalized Arterial Calcification of Infancy (GACI). These conditions affect how our body handles calcium and phosphate. They can cause severe and early calcification.
Secondary causes are more common. They include chronic kidney disease (CKD) and diabetes mellitus. CKD messes with mineral balance, raising the risk of calcification. Diabetes can also cause calcification through high blood sugar and changes in calcium levels.
Risk Assessment and Predisposition
Figuring out who’s at risk for calcification involves looking at several factors. Age, gender, and health conditions like high blood pressure and diabetes are important. Smoking also increases the risk.
Tools and biomarkers help spot people at high risk. For example, CT scans can show calcification. Biomarkers related to minerals can also signal a higher risk.
Knowing the causes and risks helps doctors create better prevention and treatment plans. This way, they can help people avoid or manage calcification.
Chronic Kidney Disease and Arterial Calcification
Arterial calcification is a big problem for people with chronic kidney disease. It makes their health worse and can even be deadly. We will look at how CKD causes this problem and the role of mineral and bone disorders.
Mechanisms of CKD-Induced Calcification
CKD messes with how the body handles minerals. This leads to too much phosphate and not enough calcium. It also affects parathyroid hormone and vitamin D levels. These changes cause calcium and phosphate to build up in arteries, making them stiff and raising heart disease risk.
As CKD gets worse, the kidneys can’t keep minerals in balance. This makes the problem of calcification even worse. People with CKD often have high levels of FGF23, which also increases the risk of hardening in arteries.
“The pathogenesis of vascular calcification in CKD is multifactorial, involving factors such as inflammation, oxidative stress, and the aforementioned mineral metabolism disturbances.”
Mineral and Bone Disorder in CKD
Mineral and bone disorder is common in CKD. It’s caused by problems with calcium, phosphate, PTH, and vitamin D. This disorder can lead to different bone problems, like osteitis fibrosa cystica, adynamic bone disease, and osteomalacia.
| CKD-MBD Component | Description | Impact on Arterial Calcification |
| Hyperphosphatemia | Elevated phosphate levels | Increases risk of calcification |
| Secondary Hyperparathyroidism | Overproduction of PTH | Contributes to bone turnover and calcification |
| Osteitis Fibrosa Cystica | Bone disease characterized by high bone turnover | Associated with increased risk of vascular calcification |
It’s important to understand how CKD, mineral metabolism, and bone health are connected. This helps manage the risk of arterial calcification in these patients.
Diabetes Mellitus as a Cause of Vascular Calcification
Diabetes mellitus causes vascular calcification through hyperglycemia, oxidative stress, and changes in calcium metabolism. It speeds up vascular calcification, increasing the risk of heart problems.
Hyperglycemia and Calcium Metabolism
High blood sugar in diabetes messes with calcium levels, leading to vascular calcification. High glucose levels start pathways that add calcium to artery walls. We’ll look at how high blood sugar affects calcium and causes calcification.
Research shows high blood sugar increases AGEs in arteries, causing calcification. It also changes vascular smooth muscle cells into osteoblasts, depositing calcium.
Diabetic Macrovascular Complications
Diabetes raises the risk of big blood vessel problems like atherosclerosis and calcification. These issues come from insulin resistance, bad cholesterol, high blood pressure, and high blood sugar.
To see how diabetes affects calcification, let’s compare diabetic and non-diabetic groups:
| Condition | Diabetic Population | Non-Diabetic Population |
| Vascular Calcification Prevalence | High | Low to Moderate |
| Cardiovascular Risk | Significantly Increased | Baseline |
| Impact of Hyperglycemia Control | Reduced Progression with Tight Control | N/A |
Managing diabetes well is key to stopping or slowing vascular calcification. It’s not just about controlling blood sugar. It also means dealing with high blood pressure and bad cholesterol.
Genetic Disorders Leading to Arterial Calcification
We look into how genetics affect arterial calcification. We focus on rare disorders that start in infancy and other hereditary conditions. These genetic factors can change how arteries calcify, unlike other causes.
Generalized Arterial Calcification of Infancy (GACI)
Generalized Arterial Calcification of Infancy is a rare genetic disorder. It causes widespread arterial calcification in babies. This is often due to ENPP1 gene mutations, which control mineralization in the body.
GACI can cause serious heart problems. These include heart attacks and heart failure, leading to early death.
To diagnose GACI, doctors use imaging and genetic tests. They look for ENPP1 gene mutations. Managing GACI is hard, focusing on symptom relief and heart risk management.
Other Hereditary Conditions
Other hereditary conditions also lead to arterial calcification. These include disorders that affect mineral and vascular health. Examples are pseudoxanthoma elasticum and idiopathic basal ganglia calcification.
Pseudoxanthoma elasticum causes tissue and artery calcification. It increases heart disease risk.
Knowing the genetic causes of these conditions is key. It helps in finding better treatments and improving life for those affected. Genetic testing and counseling are also important for identifying risk in families.
Cardiovascular Risk Factors and Arterial Calcification
Arterial calcification is a sign of heart disease. It’s linked to things we can change, like high blood pressure, bad cholesterol, and smoking. Knowing about these factors helps us find ways to prevent and treat heart disease.
Hypertension and Vessel Wall Changes
Hypertension, or high blood pressure, is a big risk for arterial calcification. The high pressure damages the blood vessel walls, leading to calcification. Studies show that controlling blood pressure can lower the risk of calcification.
Hypertension affects the blood vessels in many ways. It damages the inner lining of the blood vessels and promotes calcification. This damage is due to the high pressure and the body’s response to it.
Dyslipidemia and Calcification Processes
Dyslipidemia, or abnormal blood lipids, also increases the risk of arterial calcification. The link between bad lipids and calcification is complex. High levels of LDL cholesterol and low levels of HDL cholesterol are linked to more calcification.
- LDL cholesterol helps form foam cells, which are part of atherosclerotic plaques that can calcify.
- HDL cholesterol, on the other hand, may protect against calcification, but we don’t fully understand how.
Smoking and Oxidative Stress
Smoking is a major risk for heart disease and arterial calcification. It causes oxidative stress and inflammation in the blood vessels, making them more likely to calcify. The chemicals in cigarette smoke harm the blood vessel lining and encourage calcification.
Quitting smoking is key to reducing the risk of heart disease. Doctors should push for smoking cessation programs to help lower heart disease risk.
In summary, risk factors like high blood pressure, bad cholesterol, and smoking are key in arterial calcification. Understanding and managing these risks is vital for preventing heart disease.
Clinical Implications of Arterial Calcification
Arterial calcification has big effects on our health, raising the chance of heart problems and affecting many parts of our body. It’s key to manage it well to avoid serious heart damage.
Cardiovascular Complications
Calcification in arteries ups the risk of heart attacks, strokes, and death from heart disease. It makes arteries stiff, raising blood pressure and heart work. “The stiffening of arteries due to calcification is a major predictor of cardiovascular morbidity and mortality.” This also speeds up atherosclerosis, making heart health worse.
Calcification’s effect on the heart is big. It can cause the heart to work harder, leading to thickening, poor function, and even heart failure. The complex interplay between arterial calcification and cardiac function highlights the need for early action.
Impact on Organ Systems
Calcification in arteries doesn’t just harm the heart. It also affects other parts of the body. For example, it can cause high blood pressure and kidney problems. The impact on kidney function can worsen mineral and bone disorders, creating a cycle.
It also raises the risk of stroke and brain decline. Calcification in other arteries can lead to leg pain and reduced mobility. This is known as peripheral artery disease.
The effects of arterial calcification are wide-ranging, needing a detailed management plan. Understanding these effects helps doctors create better strategies to reduce risks.
“The management of arterial calcification requires a multidisciplinary approach, incorporating lifestyle modifications, pharmacological interventions, and potentially novel therapeutic strategies to mitigate its clinical implications.”
Diagnostic Approaches for Arterial Calcification
Diagnosing arterial calcification involves several steps. These include imaging and checking biomarkers. Accurate diagnosis is key to managing heart risks and avoiding serious problems.
We use different methods to find and measure arterial calcification. These steps help us see how much calcification there is and guide treatment plans.
Imaging Techniques
Imaging is a big part of diagnosing arterial calcification. Computed Tomography (CT) scans are very good at finding calcification. They can also measure how much calcium is there.
CT scans show us how much calcification is in the arteries. This helps us understand how serious the problem is. Other tools like X-rays and ultrasound can also help, but CT scans are more accurate.
Biomarkers for Calcification
Besides imaging, we use biomarkers to check for arterial calcification. Biochemical markers like osteocalcin and alkaline phosphatase show how much calcification is happening.
We also look at other biomarkers. These include ones related to mineral balance and inflammation. They help us understand why calcification is happening.
By using imaging and biomarkers together, we get a full picture of arterial calcification. This helps us create better treatment plans.
Treatment Strategies for Disorders Causing Arterial Calcification
Dealing with disorders that lead to arterial calcification needs a detailed plan. It’s about reducing risks and slowing down the disease. Understanding the root cause is key to creating the right treatment plan.
Disease-Specific Interventions
Each disease needs its own treatment for arterial calcification. For those with chronic kidney disease (CKD), managing mineral and bone disorder is essential. This means keeping phosphate levels in check, using vitamin D analogs, and calcimimetics to control parathyroid hormone.
| Disease | Intervention | Goal |
| CKD | Phosphate control, Vitamin D analogs, Calcimimetics | Regulate mineral and bone disorder |
| Diabetes Mellitus | Glycemic control, Lifestyle modifications | Reduce macrovascular complications |
For diabetes patients, keeping blood sugar levels in check and making lifestyle changes are critical. These steps help lower the risk of heart problems and arterial calcification.
“The management of vascular calcification in patients with CKD requires a complete approach. This includes controlling serum phosphate, calcium, and parathyroid hormone levels.” –
KDOQI Guidelines
Novel Therapeutic Approaches
New treatments aim to directly tackle arterial calcification. One promising method is using inhibitors of calcification, like sodium thiosulfate. It has shown to reduce vascular calcification in CKD patients.
Another strategy is to target the calcification process itself. This includes using anti-inflammatory agents to lessen oxidative stress and inflammation. These factors play a big role in calcification.
- Sodium thiosulfate for vascular calcification
- Anti-inflammatory agents to reduce oxidative stress
- Targeting pathways leading to calcification
At Liv Hospital, we’re dedicated to giving full care to those with arterial calcification disorders. Our team creates custom treatment plans. They use the latest in therapy to help our patients.
Conclusion
Managing arterial calcification well needs a full plan that tackles the root causes and risks. At Liv Hospital, we focus on a team effort to handle this condition. Our team of experts from different fields works together to offer top-notch care.
We’ve talked about how diseases like chronic kidney disease and diabetes can lead to arterial calcification. Knowing this helps doctors create better prevention and treatment plans.
Managing arterial calcification means fixing the underlying problems and reducing risk factors. We aim to give our patients the best care using the newest medical tech and methods. This ensures they get the best results.
We use the latest technology and put our patients first to better their lives. Our goal is to give each patient care that fits their needs. This way, we help them live healthier lives.
FAQ
Which disorder would cause calcification of the arteries?
Chronic kidney disease, diabetes mellitus, and genetic conditions like Generalized Arterial Calcification of Infancy (GACI) can cause artery calcification.
What is arterial calcification?
Arterial calcification is when calcium and phosphate build up in artery walls. This makes the arteries hard and stiff.
How does chronic kidney disease contribute to arterial calcification?
Chronic kidney disease (CKD) leads to artery calcification. It does this through issues with mineral and bone disorder, like calcium and phosphate problems.
What is the relationship between diabetes mellitus and vascular calcification?
Diabetes mellitus increases the risk of vascular calcification. This is due to high blood sugar, oxidative stress, and inflammation. These factors affect calcium metabolism and lead to big vessel problems.
What are the cardiovascular risk factors that contribute to arterial calcification?
Risk factors for artery calcification include high blood pressure, bad cholesterol, and smoking. These factors change the vessel walls and cause calcification in different ways.
How is arterial calcification diagnosed?
Doctors use imaging like CT scans and biomarkers to find artery calcification. These tools show calcification and damage to the blood vessels.
What are the treatment strategies for disorders causing arterial calcification?
Treatments for artery calcification include managing diseases like CKD and diabetes. There are also new treatments to reduce calcification and lower heart disease risk.
Can genetic disorders lead to arterial calcification?
Yes, genetic disorders like Generalized Arterial Calcification of Infancy (GACI) can cause artery calcification. They affect how the body regulates calcium and phosphate.
What are the clinical implications of arterial calcification?
Arterial calcification raises the risk of heart attacks and strokes. It also affects other organs because of reduced blood flow and high blood pressure.
References:
In CKD, the body’s regulation of calcium (Ca) and phosphate (P) becomes disturbed, which directly promotes vascular smooth muscle cells (VSMCs) in the arterial wall to transform into bone-type (osteogenic) cells, thereby depositing calcium–phosphate crystals in the arteries





