Azoospermia means a man has no sperm in his ejaculate. This significant condition affects about 1% of men. It’s also a big reason for male infertility, making up 8 to 15% of cases. Knowing about azoospermia is key for men looking into fertility treatments.
We understand how azoospermia affects families. At Liv Hospital, we aim to help with top-notch care and treatments. We want to give hope and help through sperm retrieval and other fertility technologies.
Key Takeaways
- Azoospermia is defined as the absence of sperm in a man’s ejaculate.
- It affects about 1% of all men and 15% of infertile men.
- Understanding azoospermia is key for fertility treatment.
- Liv Hospital offers advanced treatments for azoospermia.
- Effective sperm retrieval and assisted reproductive technologies are available.
Understanding Azoospermia: Which Medical Term Means Condition of No Sperm
Azoospermia is a term for when a man’s semen has no sperm. It’s a common issue that affects many men worldwide. This condition is a big factor in male infertility.
Definition and Medical Terminology
Azoospermia means a man’s semen has no sperm. Doctors use a semen analysis to check for this. They look at the semen under a microscope after spinning it down.
To be sure, doctors do two semen tests at different times. This makes sure the results are correct.
There are two main types of azoospermia. Obstructive azoospermia happens when there’s a blockage in the sperm delivery system. Non-obstructive azoospermia is when there’s a problem with sperm production.
Prevalence and Demographics
About 1% of all men have azoospermia. But, up to 15% of men with infertility issues have it. The exact number depends on the cause.
- Prevalence in the general male population: around 1%
- Prevalence among infertile men: up to 15%
- Types: Obstructive and Non-Obstructive Azoospermia
Impact on Male Fertility
Azoospermia greatly affects a man’s ability to have children. It can also cause emotional stress for couples trying to conceive.
Doctors start by doing a physical exam and blood tests. They check if the problem is with sperm production or transport. Knowing the cause helps find the right treatment.
Key diagnostic steps include:
- Comprehensive semen analysis
- Hormonal testing and blood work
- Genetic testing and chromosomal analysis
Types of Azoospermia
It’s important to know the different types of azoospermia to find the right treatment. Azoospermia is mainly split into two types: obstructive and non-obstructive.
Obstructive Azoospermia Overview
Obstructive azoospermia happens when something blocks the way sperm can move. This block can be anywhere from the testicles to the vas deferens. Even though there’s a blockage, sperm production might not be affected; it just can’t get out. Reasons include being born with it, infections, or past surgeries.
Non-Obstructive Azoospermia Overview
Non-obstructive azoospermia means there’s little to no sperm being made in the testes. It can be caused by genetic problems, hormonal issues, or environmental factors. Unlike obstructive azoospermia, the problem is with making sperm, not moving them.
Knowing if you have obstructive or non-obstructive azoospermia is key to choosing the right treatment. Tests like semen analysis, hormone checks, and genetic tests help figure out which one you have.
Causes of Obstructive Azoospermia
Blockages in the male reproductive system can cause obstructive azoospermia. This is when there’s no sperm in the semen. Knowing what causes these blockages is key to finding the right treatment.
Congenital Blockages and Abnormalities
Congenital issues are a big reason for obstructive azoospermia. Conditions like cystic fibrosis can block the vas deferens. This is a major part of the male reproductive system. Other birth defects, like epididymal obstruction, can also cause this problem.
Infections and Inflammatory Conditions
Infections and inflammation can lead to scarring and blockages. Epididymitis, an inflammation of the epididymis, is one such condition. It can cause obstructive azoospermia if not treated right.
Surgical Complications and Vasectomy
Surgical problems, including those from vasectomy, can also cause obstructive azoospermia. Vasectomy is a way to prevent pregnancy by cutting or blocking the vas deferens. But, some men might want to have kids later, making it important to understand these complications.
The following table summarizes the causes of obstructive azoospermia:
| Cause | Description |
|---|---|
| Congenital Abnormalities | Conditions such as cystic fibrosis or epididymal obstruction present at birth. |
| Infections and Inflammation | Conditions like epididymitis that cause scarring and blockages. |
| Surgical Complications | Complications arising from surgeries such as vasectomy. |
Causes of Non-Obstructive Azoospermia
Non-obstructive azoospermia is caused by many factors. These include genetics, hormones, and the environment. Knowing these causes helps in finding the right treatments.
Genetic Disorders Including Klinefelter Syndrome
Genetics play a big role in non-obstructive azoospermia. Klinefelter syndrome is a common cause. It happens when males have an extra X chromosome (XXY). This affects how their testicles work and how they make sperm.
Other genetic issues can also cause non-obstructive azoospermia. These include:
- Y chromosome microdeletions, which can affect sperm production genes
- Mutations in genes important for making sperm
- Chromosomal problems like translocations or deletions
Hormonal Imbalances and Endocrine Factors
Hormones are key to making sperm. Problems like hypogonadotropic hypogonadism can stop sperm production. Other issues, like thyroid problems and too much prolactin, can also hurt fertility.
Important hormonal factors include:
- Low testosterone, which is vital for making sperm
- Not enough FSH and LH, important for testicles
- Too much prolactin, which messes with hormone balance
Environmental, Medication, and Lifestyle Factors
Many things in our environment and lifestyle can harm sperm production. Toxins like pesticides and heavy metals are harmful. Some medicines, like anabolic steroids and chemotherapy, can also hurt fertility.
- Too much heat, like from saunas or hot tubs
- Smoking and drinking too much alcohol
- Being overweight and related health issues
Knowing what causes non-obstructive azoospermia helps in creating better treatment plans for men with this issue.
Diagnosing Azoospermia
To find out if someone has azoospermia, doctors use many tools and methods. They look for the main cause of the problem. This is key to picking the right treatment.
Comprehensive Semen Analysis Protocol
The first step is a detailed semen analysis. A semen sample is taken and checked for sperm. The test looks at:
- Sperm count: To see if there are any sperm.
- Semen volume: To check if there’s a problem with the fluid.
- Sperm motility: This is checked, even though it’s not needed for azoospermia.
This test helps doctors tell if azoospermia is caused by a blockage or not.
Hormonal Testing and Blood Work
Hormones play a big role in azoospermia. Blood tests check hormone levels, like:
- Testosterone: Needed for making sperm.
- FSH (Follicle-Stimulating Hormone): Shows how well the testes work.
- LH (Luteinizing Hormone): Helps make testosterone.
These tests help find out why someone might have azoospermia, like hormonal issues or testicle problems.
Genetic Testing and Chromosomal Analysis
Genetic tests are used to find any genetic problems that might cause azoospermia. This includes:
- Karyotyping: Looks for chromosomal issues.
- Y chromosome microdeletion analysis: Finds Y chromosome problems that can lead to azoospermia.
These tests help understand the genetic reasons for azoospermia. They also help doctors talk to patients about their condition and risks.
Doctors use semen analysis, hormone tests, and genetic tests together. This way, they can accurately diagnose azoospermia. Then, they can choose the best treatment for each patient.
Advanced Diagnostic Procedures
Advanced diagnostic procedures are key to understanding azoospermia. When azoospermia is diagnosed, more tests are needed. These tests help figure out if it’s due to a blockage or not.
Testicular Biopsy Techniques
A testicular biopsy is a major tool in diagnosing azoospermia. It involves taking a small piece of testicular tissue for examination. This helps find out if sperm are being made.
There are several ways to do a testicular biopsy:
- Conventional Open Biopsy: This traditional method involves making a small incision in the scrotum to access the testicle.
- Needle Biopsy: A less invasive technique that uses a needle to aspirate testicular tissue.
- Microdissection Testicular Sperm Extraction (microTESE): An advanced technique that involves using an operating microscope to identify and extract seminiferous tubules likely to contain sperm.
Imaging Studies: Ultrasound and MRI
Imaging studies are essential for checking the male reproductive tract’s anatomy. They help find the cause of azoospermia.
Ultrasound: This non-invasive method is great for looking at the testes, epididymis, and vas deferens. It can spot blockages or other issues.
MRI: Magnetic Resonance Imaging gives detailed images of the reproductive tract. It’s good for finding complex blockages.
Differentiating Between Obstructive and Non-Obstructive Types
Telling obstructive from non-obstructive azoospermia is key for choosing the right treatment.
- Hormonal Testing: Hormone tests can show how well the testicles are working. They help tell if it’s a blockage or not.
- Genetic Testing: Genetic tests can find the cause, mainly in non-obstructive cases.
- Imaging and Biopsy Findings: Using imaging and biopsy results together helps make a correct diagnosis.
Treatment Options for Obstructive Azoospermia
The main goal of treating obstructive azoospermia is to fix the blockage or get sperm for IVF. Men with this condition have many treatment options. The right choice depends on the blockage’s cause and location.
Microsurgical Reconstruction Techniques
Microsurgical reconstruction is a top choice for treating obstructive azoospermia. It works well for blockages caused by vasectomy or other issues. Microsurgical vasectomy reversal fixes the vas deferens, helping men get fertile again.
Vasoepididymostomy is another microsurgical method. It connects the vas deferens to the epididymis to get around epididymal blockages.
Sperm Retrieval Methods
For those who can’t or don’t want microsurgery, sperm retrieval is an option. PESA (Percutaneous Epididymal Sperm Aspiration) and MESA (Microsurgical Epididymal Sperm Aspiration) get sperm from the epididymis. These are less invasive than surgery and work for some men with blockages.
TESE (Testicular Sperm Extraction) takes sperm directly from the testicles. It’s good for blockages that stop sperm from reaching the ejaculatory ducts.
Success Rates and Prognosis
Success in treating obstructive azoospermia varies by method and individual. Microsurgery can have high success rates, with up to 50% of men conceiving naturally after the procedure.
IVF or ICSI after sperm retrieval can also lead to high pregnancy rates. These rates range from 30% to 60% per cycle, depending on the woman’s age and sperm quality.
Men with obstructive azoospermia should talk to a fertility specialist. They can help choose the best treatment based on the man’s condition and medical history.
Treatment Approaches for Non-Obstructive Azoospermia
Treating non-obstructive azoospermia is very personal. It depends on what’s causing the condition. This condition is a big challenge for men wanting to have kids.
Hormonal Therapy and Medication Options
Hormonal therapy is often used when hormone imbalances are a problem. Medications like human chorionic gonadotropin (hCG) and follicle-stimulating hormone (FSH) help make sperm. But, how well it works can vary a lot.
A study found that about 20% of men got better with this treatment. Some even got pregnant naturally. But, it’s important to know that results can differ a lot.
| Hormone | Function | Treatment Role |
|---|---|---|
| hCG | Stimulates testosterone production | Enhances sperm production |
| FSH | Essential for sperm production | Supports spermatogenesis |
Surgical Sperm Retrieval Techniques (microTESE)
For those who don’t get better with hormones, surgery is an option. Microdissection testicular sperm extraction (microTESE) looks for sperm in the testicles under a microscope.
MicroTESE is a key treatment for non-obstructive azoospermia. It gives men a chance to be biological fathers even when sperm production is low. Success rates are good when done by experts.
Experimental and Emerging Treatments
New research is looking into treatments for non-obstructive azoospermia. Stem cell therapy and genetic treatments are being explored to fix sperm production problems.
These treatments are not common yet. But, they could be big steps forward. Men thinking about these options should know about the research and possible risks and benefits.
Fertility Options and Family Building
Even with azoospermia, new ways to build a family exist thanks to reproductive medicine. Men with this condition need to know their options.
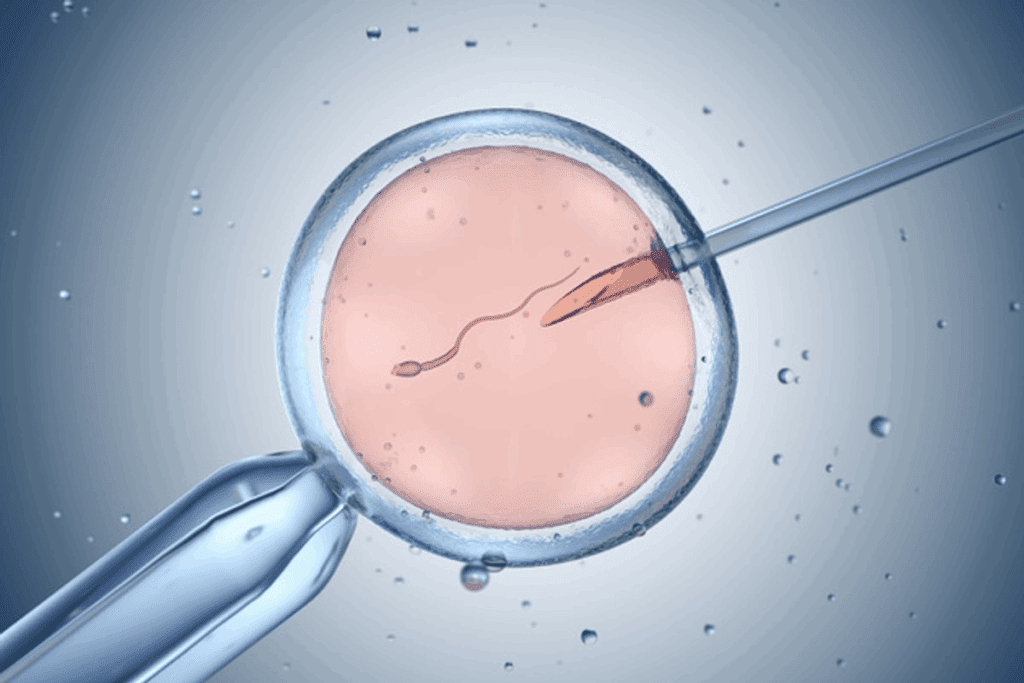
Assisted Reproductive Technologies with Retrieved Sperm
Men with azoospermia can use sperm from micro-TESE for IVF with ICSI. This method injects a sperm into an egg for fertilization. It has brought hope to many.
First, we figure out the best way to get sperm. Then, we use them in IVF-ICSI. This method works well, even with few sperm.
Donor Sperm Considerations
Using donor sperm is an option for building a family. It’s a personal choice that comes with emotional and legal considerations.
We help our patients weigh their options. We also offer counseling for those choosing donor sperm.
Adoption and Other Family-Building Alternatives
Adoption is a way to create a family. It gives a child a loving home. It’s a rewarding choice for many.
We guide those thinking about adoption. We share info on adoption types, legal needs, and emotional readiness.
Building a family with azoospermia might mean trying different paths. We support our patients at every step. We ensure they have the info and care to make informed choices.
Conclusion: Living with Azoospermia
Understanding azoospermia and its treatments can change lives. We’ve looked at the types, causes, and how to diagnose it. Treatments like surgery and assisted reproductive technologies offer hope for families.
Dealing with azoospermia needs a full approach. This includes medical checks, emotional support, and looking at treatment choices. The outlook for azoospermia varies based on the cause and personal situation. Getting professional help is key to facing its challenges.
There are resources for azoospermia support. We suggest looking into these and getting help from doctors. This way, people can make smart choices about their reproductive health and family plans.
FAQ
What is azoospermia?
Azoospermia is when a man’s semen has no sperm. It’s a big problem for many men trying to have kids.
What are the main types of azoospermia?
There are two main types: obstructive and non-obstructive azoospermia. Each has different reasons and treatments.
What causes obstructive azoospermia?
Obstructive azoospermia happens when something blocks the way sperm can get out. This can be due to birth defects, infections, or surgery problems.
What are the causes of non-obstructive azoospermia?
Non-obstructive azoospermia is often due to genetic issues like Klinefelter syndrome. Hormonal imbalances and lifestyle choices also play a part.
How is azoospermia diagnosed?
Doctors use semen analysis, hormone tests, and genetic tests to find out if you have azoospermia. They might also do a testicular biopsy or imaging studies.
What are the treatment options for obstructive azoospermia?
Doctors can try to fix the blockage with surgery. They might also use sperm retrieval methods like PESA, MESA, or TESE.
How is non-obstructive azoospermia treated?
For non-obstructive azoospermia, doctors might use hormone therapy. They might also try microTESE surgery or new treatments.
Can men with azoospermia have children?
Yes, men with azoospermia can have kids. They might use sperm from assisted reproductive technologies, donor sperm, or adoption.
What is the difference between obstructive and non-obstructive azoospermia?
Obstructive azoospermia means there’s a blockage. Non-obstructive azoospermia means there’s a problem with sperm making, not a blockage.
Are there any emerging treatments for azoospermia?
Yes, new treatments for non-obstructive azoospermia are being researched. This includes new surgeries and therapies.
How does azoospermia affect male fertility?
Azoospermia makes it hard for men to have kids naturally. It’s because there are no sperm in the semen.
Can azoospermia be treated with medication?
Sometimes, taking medicine can help if hormonal imbalances cause non-obstructive azoospermia. This might help make more sperm.
What is the role of genetic testing in diagnosing azoospermia?
Genetic testing finds the causes of azoospermia, like Klinefelter syndrome. It helps doctors decide on treatment and tells if there’s a risk of passing on genetic problems.
References
National Center for Biotechnology Information. Azoospermia: Diagnosis and Understanding Male Infertility. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3583160/[4