Last Updated on December 5, 2025 by Bilal Hasdemir
Imagine being awake during a delicate procedure where skilled surgeons work on your mind’s most complex parts. At Liv Hospital, we focus on you, making sure you’re safe, comfortable, and get the best care.
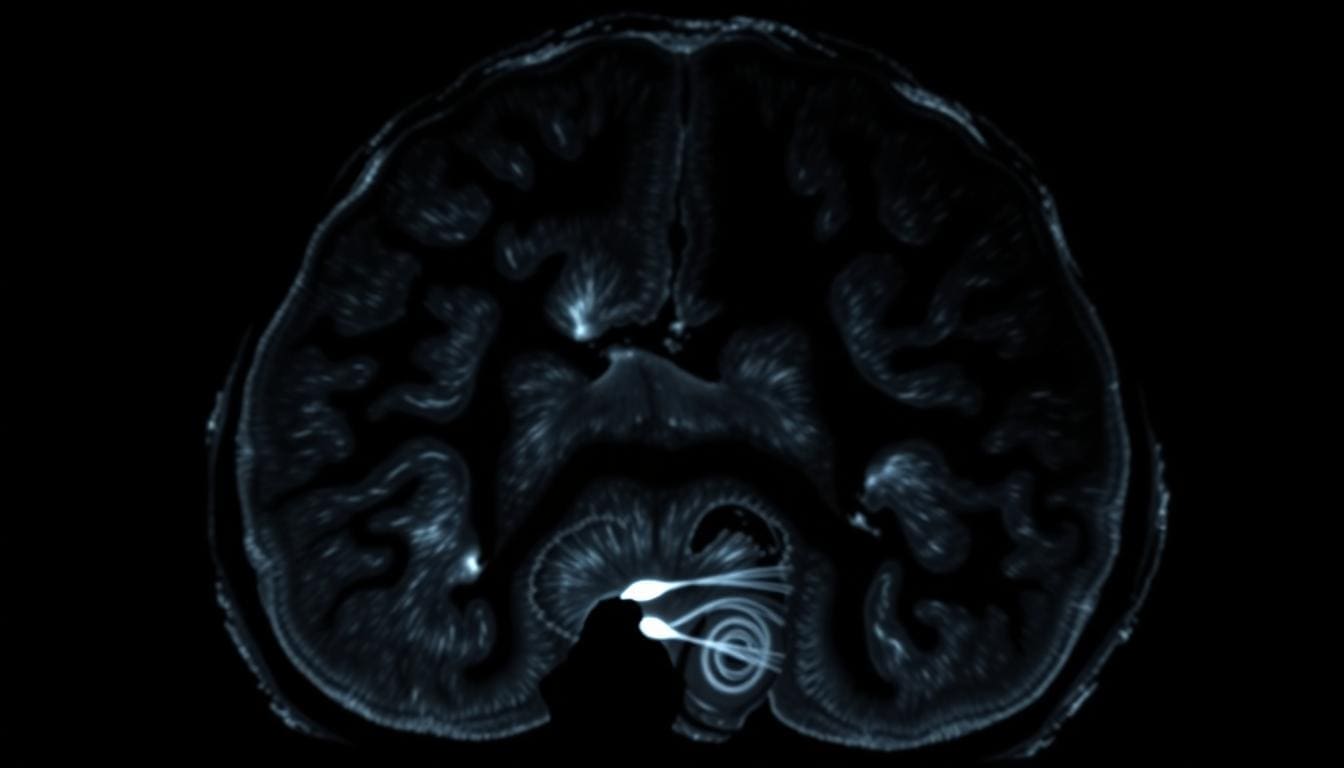
Awake craniotomy procedures let our neurosurgeons watch your brain functions as they happen. This way, they can avoid harming areas that control language, movement, or feeling. It helps us get more accurate results.
Being awake lets patients react to what’s happening. This helps our surgeons understand your brain better. Working together is key to a good outcome.
Key Takeaways
- Awake craniotomy allows for real-time monitoring of brain functions.
- Patients remain awake to respond to stimuli during the procedure.
- This technique reduces the risk of damage to critical brain areas.
- Liv Hospital prioritizes a patient-centered approach for optimal care.
- Collaboration between patient and surgeon is key to a successful outcome.
The Purpose of Consciousness During Neurosurgery
Surgeons often choose to keep patients awake during neurosurgery. This is to get more precise and protect important brain functions. This method, known as awake brain surgery, lets them watch brain activity in real-time. This way, they can make sure they don’t harm critical areas.
The main reason for keeping patients awake is to protect critical brain functions. These include speech, motor skills, and how we sense things. By keeping patients awake, surgeons can avoid harming areas that control these important functions.
Protecting Critical Brain Functions
During awake brain surgery, patients do tasks that test their brain functions. They might speak, move limbs, or react to sensory stimuli. This feedback helps surgeons map the brain’s areas and avoid them with more precision.
For example, if a tumor is near a language processing area, the patient might name objects or read sentences. This helps the surgeon locate and keep safe the language centers. It reduces the chance of language problems after surgery.
Improving Surgical Precision and Outcomes
Awake brain surgery improves surgical precision and outcomes. Surgeons can adjust as they go based on the patient’s responses. This is key when the tumor or lesion is close to important brain structures.
Research shows awake surgeries are often used when tumors or seizure spots are near brain areas that work. Keeping the patient awake helps avoid harming these areas. This leads to better results and less chance of neurological problems after surgery.
The benefits of awake brain surgery are backed by studies. They show it helps with improving surgical precision and keeping patients safe. As neurosurgery gets better, awake surgery will likely play an even bigger role in helping patients with complex brain issues.
Are U Awake During Brain Surgery? The Complete Picture
Deciding if patients should be awake during brain surgery is a big decision. We look at many factors. These include the type of brain condition, where it is, and the patient’s health.
When Awake Surgery Is Necessary
Awake surgery is needed for certain brain conditions. This is because some brain areas control important functions like language and movement. Being awake lets us watch these functions closely during surgery.
For example, if a tumor is near areas that control speech or movement, awake surgery helps. It lets us map the brain and avoid damaging important areas. This reduces the chance of problems after surgery, like trouble speaking or paralysis.
A great example of awake surgery’s success is a Parkinson’s patient playing the clarinet during surgery. This was reported in Irish News. It shows how awake surgery can be precise and flexible.
Cases Where Traditional Anesthesia Is Preferred
But, there are times when traditional anesthesia is better. This is for surgeries in less sensitive brain areas or when the patient can’t stay awake due to anxiety or health issues.
| Surgery Type | Awake Surgery | Traditional Anesthesia |
|---|---|---|
| Tumors near critical brain areas | Recommended | Not preferred |
| Deep brain stimulation for Parkinson’s | Often used | Possible but less common |
| Surgeries not involving critical areas | Not necessary | Preferred |
The table shows that choosing between awake surgery and traditional anesthesia depends on the surgery. We carefully decide what’s best for each patient.
“The ability to perform surgery on an awake patient allows for a more precise and safer procedure, even in delicate brain areas.”
Patient Selection for Awake Craniotomies
Choosing to do an awake craniotomy means looking at both medical and mental health factors. This careful choice is key to make sure patients are right for the surgery. It also helps them handle being awake during brain surgery.
Medical Criteria and Considerations
Doctors look at several medical things when picking patients for awake craniotomies. They check the brain lesion’s location and how complex it is. They also look at the patient’s health and brain status.
Lesions near important brain parts, like those for speech or movement, are a big deal. Patients with these lesions might be good for awake craniotomies. Being awake lets the team watch brain functions live, lowering damage risks.
| Medical Factor | Consideration |
|---|---|
| Location of Lesion | Proximity to critical brain areas |
| Complexity of Lesion | Difficulty of surgical access |
| Patient’s Overall Health | Presence of comorbidities |
Psychological Preparation and Evaluation
It’s not just about the medical stuff. The mental prep and check-up of patients are also key. Patients need to get what the surgery is about and follow directions while awake.
Psychological assessment checks if patients can handle the stress of being awake during surgery. They look at mental health history, understanding of the surgery, and how well they can cope.
Choosing patients for awake craniotomies is a detailed process. It looks at both medical and mental health aspects. This careful selection helps pick the right patients for this complex surgery, aiming for the best results.
The Awake Craniotomy Procedure Explained
The awake craniotomy procedure is a team effort between the surgical team and the patient. It’s a complex neurosurgical technique that needs careful planning and execution. This ensures the best possible results.
Pre-Surgical Preparation and Planning
Pre-surgical preparation is key for the awake craniotomy procedure. We start by reviewing the patient’s medical history and current health. We check their neurological status, look at imaging studies, and talk about the procedure’s risks and benefits.
We also prepare the patient mentally. We explain the surgery steps and what they’ll experience during the awake part. This helps lower anxiety and makes the patient more comfortable and cooperative.
Anesthesia Techniques and Management
Advanced anesthesia techniques are used to reduce pain and discomfort during awake craniotomies. We use a mix of local anesthesia and conscious sedation. This keeps the patient comfortable while they stay awake and responsive.
Local anesthetics numb the scalp and incision areas. Conscious sedation helps the patient relax at the start of surgery. We manage the sedation level so the patient can wake up easily when needed.
| Anesthesia Technique | Description | Benefits |
|---|---|---|
| Local Anesthesia | Numbing the scalp and incision areas | Pain management during surgery |
| Conscious Sedation | Relaxing the patient during initial surgery stages | Reduces anxiety, allows patient to remain responsive |
The Awakening Process During Surgery
During the awake craniotomy, the patient is slowly brought out of sedation. We check their language, motor, and sensory functions in real-time.
We monitor the patient’s response to different stimuli and tasks. This helps us map the brain’s functional areas and avoid critical regions during surgery. The awakening process is done slowly, with close attention to the patient’s comfort and neurological status.
By using advanced anesthesia techniques and careful planning, we ensure the patient stays comfortable and cooperative. This leads to a successful surgical outcome.
Brain Mapping and Functional Testing
Awake craniotomies rely on advanced brain mapping and testing. These tools help surgeons navigate the brain’s complex landscape. They identify key brain areas and check their function in real-time. This makes neurosurgery more precise and safe.
Language and Speech Assessment Methods
Language and speech tests are key in awake craniotomies. We use tasks like naming pictures, reading, and talking to check language skills. These tests help pinpoint brain areas for language, ensuring they’re not harmed during surgery.
We might ask patients to name objects or read sentences while stimulating brain areas. This creates a detailed map of language functions. It helps us safely remove tumors or lesions without affecting language.
Motor and Sensory Function Evaluation
We also test motor and sensory functions during awake craniotomies. This includes checking limb movement and sensory perception like touch. We aim to preserve these brain areas.
For example, patients might move their hands or feet in response to stimulation. They report any sensations they feel. This info is vital for creating a detailed brain map for surgery.
Real-Time Surgical Adjustments
Brain mapping and testing allow for real-time surgical adjustments. Feedback from the patient helps us refine our approach. This ensures the best possible outcome.
This might mean adjusting the surgery’s scope or technique. We work closely with the patient to optimize results. Advanced brain mapping techniques improve recovery.
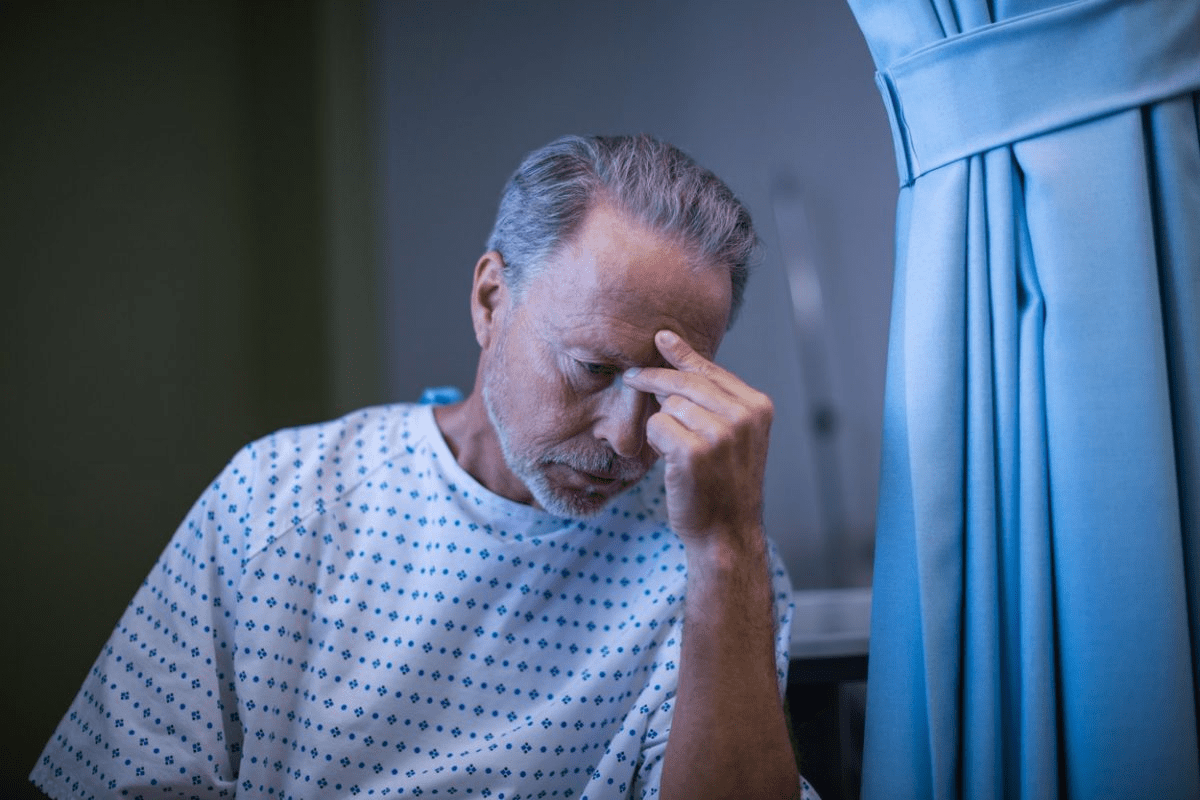
The Patient Experience During Conscious Neurosurgery
Having brain surgery while awake can seem scary. But with the right support, patients can feel confident. We make sure patients are ready and comfortable during the surgery.
Pain Management and Comfort Measures
Managing pain is key during awake neurosurgery. We use advanced anesthesia to keep patients comfortable. Our team listens to patients to tailor care for the best experience.
Some important steps we take include:
- Local anesthesia to numb the area
- Conscious sedation to relax patients
- Monitoring comfort and feedback
Communication With the Surgical Team
Good communication is vital during awake neurosurgery. Patients should share their feelings and any discomfort. This helps us adjust to keep patients comfortable and the surgery successful.
Our team is trained to talk clearly with patients. We reassure and explain things as needed. We also find ways for patients to communicate, like using hand signals.
Key aspects of our communication approach include:
- Pre-operative counseling to prepare patients
- Continuous dialogue during the procedure
- Emotional support and reassurance
Psychological Aspects and Support
The mental impact of awake neurosurgery is important. We offer support to help with anxiety or fear. Our team includes experts in patient care and emotional support.
To help with mental stress, we:
- Explain the procedure and what to expect
- Offer emotional support and counseling
- Encourage family involvement when possible
We focus on both the medical and mental sides of awake neurosurgery. This helps create a supportive environment for positive outcomes and patient satisfaction.
Risks, Benefits, and Side Effects
Exploring awake brain surgery, we must weigh risks against benefits. Awake craniotomies offer big advantages in some cases but also face challenges and complications.
Potential Complications and Challenges
Awake brain surgery risks include seizures, brain swelling, and infection, like traditional surgery. But, being awake adds extra challenges, like discomfort or anxiety. Careful patient selection and preparation help lessen these risks.
Keeping patients comfortable while mapping the brain is a big challenge. Advanced anesthesia techniques help balance comfort with the need for patient response during surgery.
Short-Term Side Effects
Patients may face fatigue, headache, and nausea after awake brain surgery. These effects are usually short-lived and managed with good care. Effective pain management is key to comfort after surgery.
Long-Term Advantages Over Traditional Surgery
Awake brain surgery has long-term benefits in some cases. It allows for precise brain mapping, leading to better outcomes and possibly shorter recovery times. This precision can help preserve brain functions.
Research shows awake craniotomies can improve outcomes and lower risks of long-term problems. Choosing awake brain surgery should be a careful decision, after weighing the pros and cons with a neurosurgical team.
Recovery and Outcomes After Awake Brain Surgery
Learning about recovery and outcomes after awake brain surgery can help ease patient worries. We’ll walk you through this journey. It’s key to understand the full care given after surgery.
Immediate Post-Operative Experience
Right after awake brain surgery, our team keeps a close eye on patients. They usually go to the ICU for careful watching. Important parts of early care include:
- Watching vital signs and brain function
- Managing pain to keep patients comfortable
- Looking for any complications or bad reactions
We focus on making patients comfortable and safe during this important time. Our team is ready to answer any questions patients or their families might have.
Long-Term Recovery Timeline
Recovery time after awake brain surgery can differ for everyone. Patients often see slow but steady progress over weeks or months. Things that affect recovery include:
- The size and location of the surgery
- The patient’s health before surgery
- Following doctor’s orders and rehab plans
Our team offers personalized help and support during recovery. We make sure patients get the care they need for the best results.
Research on Patient Outcomes
Studies on awake brain surgery outcomes are encouraging. Many patients see big improvements.
Looking at patient data, we see several benefits. These include:
| Outcome Measure | Benefit |
|---|---|
| Reduced risk of complications | Less chance of brain problems |
| Improved surgical precision | Keeping important brain functions safe |
| Enhanced patient recovery | Quicker return to daily life |
We keep watching and studying outcomes to improve our care even more.
Conclusion
Awake brain surgery is a big step forward in neurosurgery. We’ve looked at its purposes, benefits, and how it works. We’ve also talked about what it’s like for the patient.
This surgery lets doctors watch brain functions in real time. It helps avoid harming important areas like those for speech and movement. It’s a great option for some patients, leading to better results.
As neurosurgery keeps getting better, awake brain surgery is more important than ever. More research and improvements will help care for patients even more. Understanding awake brain surgery helps us see the progress in medicine and how it improves lives.
FAQ
Are you awake during brain surgery?
Yes, some brain surgeries are done while the patient is awake. This is called an awake craniotomy. It lets neurosurgeons check the brain’s functions as they work.
What is the purpose of being awake during brain surgery?
Being awake helps neurosurgeons map the brain. They test brain areas that control language, movement, and feeling. This way, they can avoid harming important parts.
What are the benefits of awake brain surgery?
Awake brain surgery is precise and safe. It reduces damage to key brain areas. It also lets the surgeon make changes during the surgery.
What are the risks associated with awake brain surgery?
Awake brain surgery is mostly safe. But, it can cause anxiety, pain, and surgery-related problems. The surgical team manages these risks carefully.
How is pain managed during awake brain surgery?
Pain is managed with local anesthesia and sedation. The anesthesiology team watches the patient closely. This ensures they stay comfortable during the surgery.
What tasks are patients asked to perform during awake brain surgery?
Patients do tasks like speaking, moving, or feeling tests. These help the neurosurgeon map the brain. It helps avoid important areas.
How long does it take to recover from awake brain surgery?
Recovery varies, but most stay in the hospital for days. Full recovery can take weeks to months. It depends on the surgery and the patient’s health.
Are there any long-term advantages to awake brain surgery compared to traditional surgery?
Yes, awake brain surgery might have long-term benefits. It could lead to fewer cognitive and functional problems. This is because it’s tailored to protect key brain areas.
Can anyone undergo awake brain surgery?
No, not everyone can have awake brain surgery. The decision depends on the brain lesion’s location and complexity. It also depends on the patient’s mental and physical health.
What is the role of brain mapping during awake craniotomies?
Brain mapping is key during awake craniotomies. It helps neurosurgeons find and protect important brain areas. They use various methods to check brain function in real-time.
How does awake brain surgery impact patient outcomes?
Studies show awake brain surgery can improve outcomes. It reduces the risk of neurological problems. It may also lead to better long-term recovery.