Experiencing a failed IVF cycle can be really tough. But knowing why transfers fail is a big step towards success. The Advanced Fertility Center of Chicago says IVF is a big leap in reproductive medicine. Yet, it doesn’t always lead to a pregnancy.Detailed analysis of the causes why do ivf transfers fail and potential solutions.
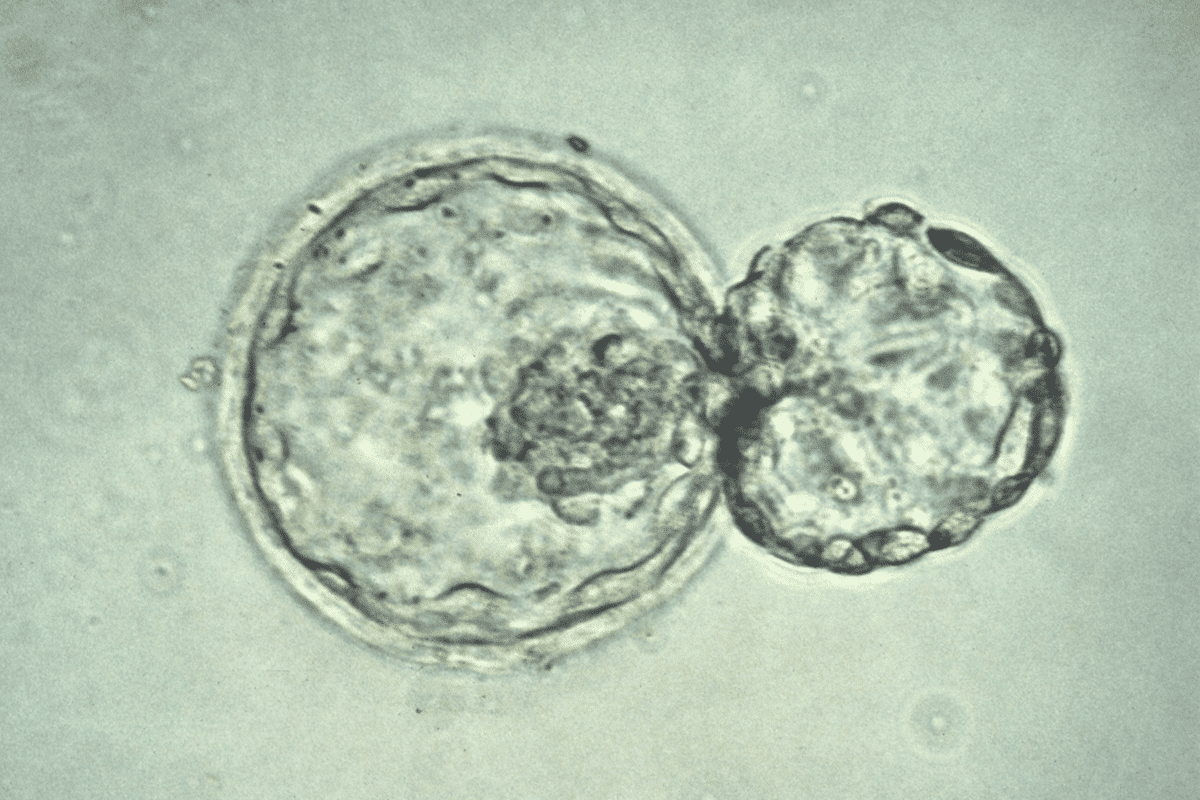
About 50 percent of embryo transfers don’t lead to pregnancy. This is often because of things we can’t see with the naked eye. Many patients wonder if there’s something they could have done differently.
Studies show that implantation failure is a complex issue. It involves how the embryo and the uterus interact.
Key Takeaways
- IVF transfer failures occur in approximately 50% of cycles.
- Genetic and chromosomal abnormalities are major contributors to IVF failure.
- Understanding the causes of IVF failure can inform treatment decisions.
- Complex interactions between the embryo and uterine environment play a role.
- Advanced laboratory techniques and embryo selection methods are key.
Understanding IVF Success Rates
IVF success rates change a lot because of different factors. Knowing these factors is key for those going through fertility treatments. It helps them know what to expect and make smart choices.
Current Success Statistics
Recent numbers show IVF success rates have gone up. The American Society for Reproductive Medicine (ASRM) says the average success rate for IVF in women under 35 is about 47.7% per cycle.
Age Group | Average IVF Success Rate |
<35 years | 47.7% |
35-37 years | 37.8% |
38-40 years | 26.8% |
Factors Affecting Success Rates
Two main things affect IVF success: embryo quality and uterine lining receptivity. Other important factors include the woman’s age, lifestyle, and the reason for infertility.
Setting Realistic Expectations
It’s vital for those going through IVF to have realistic hopes. Knowing what affects IVF success helps set reachable goals. It also helps deal with the emotional side of treatment.
Embryonic Factors: The Primary Cause of IVF Failure
IVF failure often comes down to issues with the embryo. These can include chromosomal problems and developmental issues. Knowing about these factors helps us understand why IVF might not work and how to make it better.
Chromosomal Abnormalities
Chromosomal issues in embryos are a big reason for IVF failure, and they get worse with age. These problems can cause aneuploidy, where an embryo has the wrong number of chromosomes. This makes it hard for the embryo to implant or can lead to miscarriage. Luckily, we can now screen embryos for the right number of chromosomes, which boosts IVF success.
Developmental Arrest
Developmental arrest happens when an embryo stops growing, often because of genetic or environmental reasons. This can occur at any stage of growth and is a major reason for IVF failure. Things like poor embryo culture conditions and internal embryo problems can cause this.
Embryo Quality Assessment
Checking the quality of embryos is key in IVF. Embryologists look at things like cell number, cell division, and how much the cells break apart. But, there are limits to this method. New techniques like time-lapse imaging and preimplantation genetic testing (PGT) give us more info. They help us pick the best embryo for transfer.
By grasping the role of embryonic factors in IVF success, we can customize treatments better. This can lead to more successful outcomes for those trying IVF.
The Impact of Maternal Age on Why IVF Transfers Fail
The quality of eggs gets worse with age, which affects IVF success rates. As women wait longer to have children, the effect of age on IVF results grows more important.
Egg Quality Decline with Age
As women get older, their eggs’ quality drops due to biological changes. This makes it harder for eggs to be fertilized and grow into healthy embryos.
- Increased oxidative stress: Older eggs are more likely to suffer from oxidative damage.
- Mitochondrial dysfunction: The energy-making structures in eggs work less well with age.
- Epigenetic changes: Age-related changes in gene expression can impact embryo health.
Increased Aneuploidy Risk After 35
Aneuploidy, or having an abnormal number of chromosomes, is a big reason for IVF failure. The chance of aneuploidy jumps up a lot after 35.
Some key facts are:
- Aneuploidy rates go from about 10% in women under 30 to over 50% in women over 40.
- The risk of miscarriage due to aneuploidy also goes up with age.
Strategies for Older Patients
Even though older age makes IVF harder, there are ways to improve success rates for older patients.
- Preimplantation genetic testing (PGT): Screening embryos for chromosomal issues can help pick the healthiest ones for transfer.
- Donor eggs: Using eggs from younger donors can greatly boost success rates for older women.
- Personalized treatment protocols: Customizing IVF plans to fit each patient’s needs can lead to better results.
By knowing how age affects IVF success and using the right strategies, older patients can increase their chances of a successful pregnancy.
Endometrial Receptivity Issues
A receptive endometrium is key for successful implantation. The endometrium, or uterine lining, is vital in IVF treatments. It must be thick and receptive for a good outcome.
Thin Endometrial Lining
A thin endometrial lining can cause IVF failure. The ideal thickness is above 7-8 mm on embryo transfer day. A thin lining may not support embryo implantation.
Causes of a thin endometrial lining include hormonal imbalances and poor blood supply. Uterine surgeries or infections also play a role. We treat these with hormonal therapy and uterine perfusion enhancement.
Window of Implantation Timing
The window of implantation is when the endometrium is most ready for an embryo. This time is between 6-10 days after ovulation. If the embryo and endometrium are not in sync, implantation fails.
Knowing the best time for embryo transfer is essential. We use advanced tools to find the perfect timing, boosting implantation success.
Endometrial Testing Options
We use several tests to check endometrial receptivity. These include:
- Endometrial biopsy for histological analysis
- Ultrasound to check thickness and shape
- Molecular tests for gene expression
These tests help us customize IVF treatments. This improves the chances of a successful outcome.
Uterine Anatomical Abnormalities
Uterine structural issues can make it hard for embryos to implant during IVF. These problems can be fibroids, polyps, or other malformations.
Fibroids and Polyps
Fibroids and polyps grow inside the uterus. They can mess with the environment where embryos try to implant.
Treatment options for these growths include surgery. Sometimes, this can really help improve IVF success rates.
Condition | Impact on IVF | Treatment |
Fibroids | May distort uterine cavity, affecting implantation | Surgical removal (myomectomy) |
Polyps | Can cause inflammation, affecting embryo attachment | Polypectomy (surgical removal) |
Uterine Septum and Adhesions
A uterine septum is a natural wall that divides the uterus. Adhesions are scar tissue inside the uterus, often from surgeries or infections.
Both can hurt IVF chances by making it hard for embryos to implant or by creating a bad environment.
Surgical correction of these issues, like removing the septum or adhesions, can help with IVF success.
Hydrosalpinx Impact
Hydrosalpinx is when fluid builds up in the Fallopian tubes, often because of a blockage. This can harm IVF by letting harmful fluid into the uterus, making it hard for embryos to implant.
Treatment might be to remove or block the affected tube. This stops harmful fluid from getting into the uterus.
Procedure | Description | Benefit |
Salpingectomy | Removal of the affected Fallopian tube | Prevents toxic fluid from entering the uterine cavity |
Tubal Ligation | Blocking the Fallopian tube | Stops fluid drainage into the uterus |
Implantation Failure: When Good Embryos Don’t Attach
The process of implantation is complex. Even with good-quality embryos, failure can happen for many reasons. Implantation is a key step in IVF, where a healthy embryo attaches to the uterine lining, starting a pregnancy.
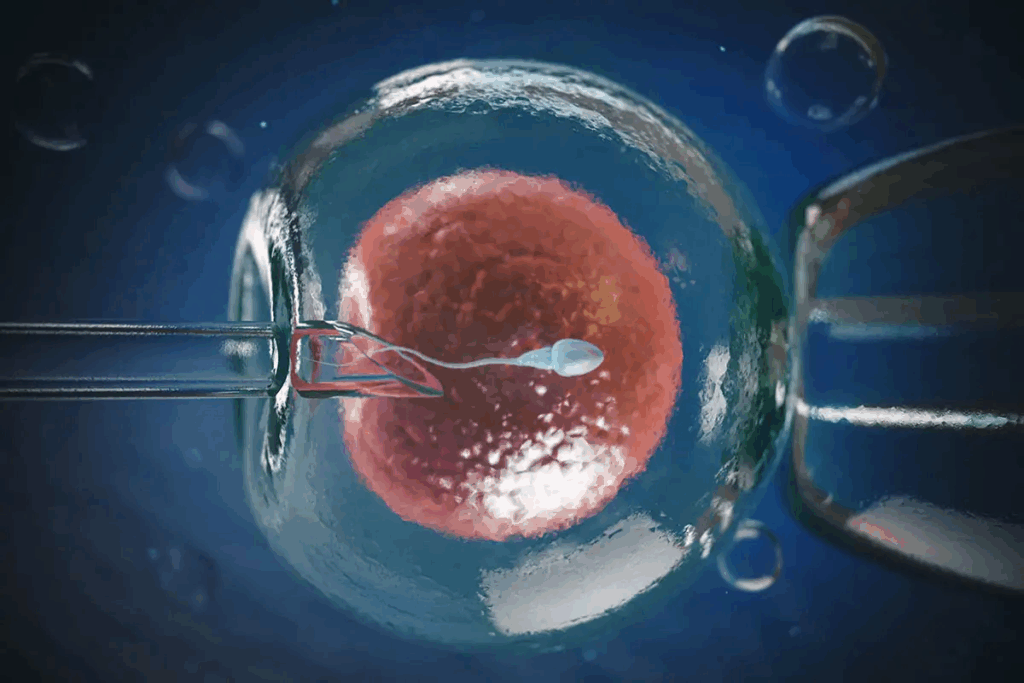
The Implantation Process
Implantation involves many steps. First, the embryo hatches from its outer shell. Then, it attaches to the endometrium. The endometrium must be ready for the embryo, and many molecular factors help this happen.
Knowing how implantation works is key to understanding why IVF might fail. Studies show that problems at the molecular level can greatly affect success rates.
Molecular Factors in Implantation
Molecular factors are very important in implantation. Cytokines and growth factors help the embryo and endometrium talk to each other. If these molecules are out of balance or not working right, implantation can fail.
Molecular Factor | Role in Implantation | Impact of Dysfunction |
Cytokines | Regulate inflammation and immune response | Altered levels can disrupt implantation |
Growth Factors | Promote endometrial receptivity and angiogenesis | Insufficient levels may hinder implantation |
Adhesion Molecules | Facilitate embryo-endometrium adhesion | Dysfunction can prevent embryo attachment |
Recurrent Implantation Failure
Recurrent implantation failure is tough. It happens when many good-quality embryos can’t implant. This is very hard for patients and needs a deep look to find the reasons.
To tackle recurrent implantation failure, we check both the embryo and the endometrium. Genetic testing of embryos and endometrial receptivity analysis help us understand why it keeps happening.
By understanding the complex factors in implantation, we can tackle the challenges of implantation failure. This helps improve IVF success rates for our patients.
Immunological Factors in IVF Failure
IVF success isn’t just about the embryo’s quality. Immunological factors also matter a lot. The immune system protects us from harm but can sometimes see the embryo as a threat. This can lead to implantation failure or early pregnancy loss.
“The immune system’s role in pregnancy is complex and multifaceted,” notes Medical Expert, a renowned fertility specialist. “Understanding and addressing immunological factors can significantly improve IVF outcomes for many patients.”
Autoimmune Conditions
Autoimmune conditions happen when the immune system attacks the body’s own tissues. In IVF, conditions like antiphospholipid syndrome (APS) or thyroid autoimmunity can raise the risk of implantation failure or miscarriage. Identifying and managing these conditions is key to better IVF success rates.
For example, APS can lead to blood clots and pregnancy complications. Testing for these conditions and treating them can lower these risks.
Elevated Natural Killer Cells
Natural Killer (NK) cells are immune cells that can impact IVF success. While NK cells are important, high levels in the uterus or blood can lead to implantation failure and miscarriage.
The exact role of NK cells in IVF failure is being studied. Monitoring NK cell levels and finding ways to control their activity is part of addressing immunological factors in IVF.
Immunotherapy Options
Immunotherapy is about treating the immune system to help IVF succeed. Options like intravenous immunoglobulin (IVIG) and low-dose aspirin are being explored. These treatments aim to reduce immune activity against the embryo, creating a better environment for implantation.
The success of these treatments can vary. Yet, they offer hope for patients facing IVF failure due to immunological issues.
As we learn more about immunological factors in IVF, we can offer more tailored care. By tackling these factors, we can boost the chances of successful IVF outcomes.
Male Factor Contributions to Failed IVF
Understanding male factors is key to solving IVF failures. While female factors get a lot of attention, male factors play a big role too. We’ll look at how sperm quality, like DNA fragmentation and selection, affects IVF success.
Sperm DNA Fragmentation
Sperm DNA fragmentation means there are breaks in the DNA of sperm. High levels can cause poor embryo quality and lower IVF success. Research shows sperm DNA fragmentation greatly impacts IVF success, making it a key area to focus on in male infertility.
A study in the Journal of Assisted Reproduction and Genetics linked high DNA fragmentation to lower pregnancy and higher miscarriage rates in IVF. So, checking and fixing sperm DNA fragmentation is vital for better IVF results.
Sperm Selection Challenges
Choosing the right sperm for IVF, like for ICSI, is tough. The task is to pick sperm with normal shape and movement, but even then, DNA integrity is not guaranteed. New methods are being created to better select sperm.
“The development of advanced sperm selection techniques has improved the chances of selecting healthy sperm for IVF, which boosts the chances of successful outcomes.”
Advanced Sperm Selection Techniques
Several new methods are available to enhance sperm selection for IVF. These include:
- Intracytoplasmic Morphologically Selected Sperm Injection (IMSI)
- Motile Sperm Organelle Morphology Examination (MSOME)
- High-Resolution Sperm Selection
These techniques let for a closer look at sperm shape and DNA integrity, helping embryologists pick the best sperm for fertilization.
Technical and Procedural Factors
Understanding the technical and procedural factors in IVF is key to better treatment results. The quality of the embryo and the uterus’s readiness are important. But, the technical steps of IVF also play a big role in success.
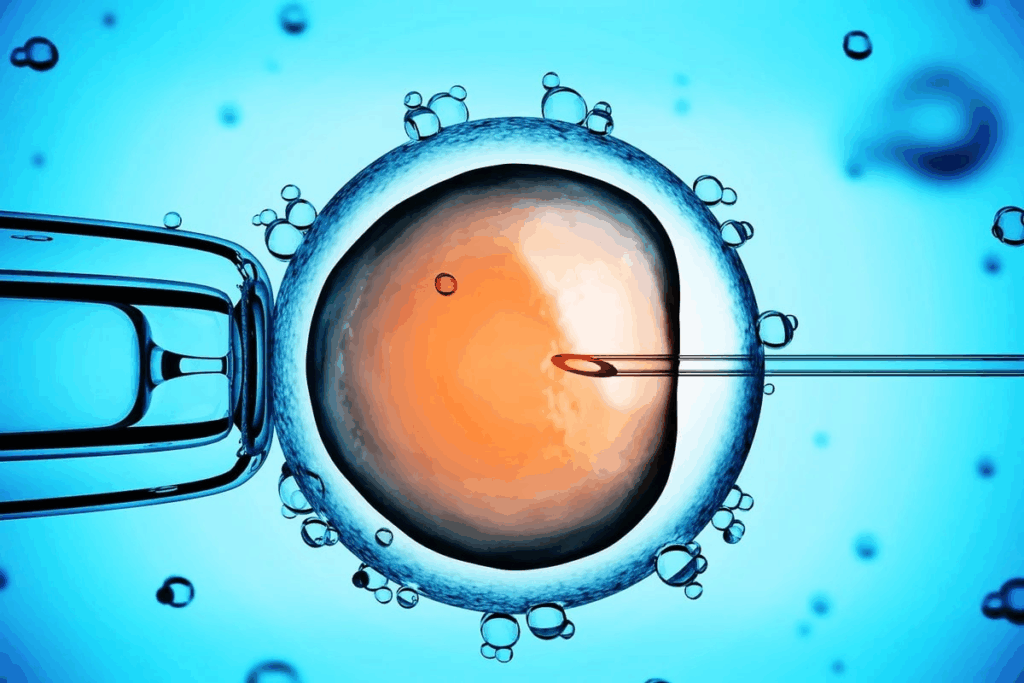
Embryo Transfer Technique
The way embryos are transferred is very important for IVF success. A careful and precise transfer can help the embryo and the uterine lining. Studies show that the skill of the person doing the transfer greatly affects results. It’s a good idea for patients to ask about their clinic’s transfer techniques and the experience of the practitioners.
Laboratory Conditions
The conditions in the lab where embryos are kept also matter. Things like the quality of the culture media and the stability of the incubation environment are key. Top labs use strict quality control and the latest equipment to improve embryo culture. It’s important to make sure the lab meets high standards for the best chance of success.
Timing of Transfer
The timing of the embryo transfer is also critical. It’s important to match the embryo’s growth stage with the uterine environment for implantation. Research shows that the window for implantation is small, making timing very important. We work with patients to find the best time for the transfer based on their cycle and embryo growth.
By focusing on these technical and procedural aspects, we can boost IVF success rates. It’s a detailed process that needs a commitment to using the latest in IVF technology and techniques.
Lifestyle and Environmental Influences
Our lifestyle and environment can greatly affect IVF success. Understanding how our daily choices and surroundings impact our chances is key. This knowledge is vital as we go through the IVF journey.
Nutrition and Weight
Eating a balanced diet is essential for reproductive health. Lack of nutrients can harm eggs, sperm, embryos, and the uterus. It’s important for a healthy outcome.
Key Nutritional Considerations:
- Maintaining a healthy weight to optimize hormone levels and improve IVF outcomes
- Consuming a diet rich in antioxidants to reduce oxidative stress
- Including essential fatty acids for hormone production and overall reproductive health
Nutrient | Food Sources | Benefit for IVF |
Folic Acid | Leafy greens, citrus fruits | Prevents neural tube defects |
Omega-3 Fatty Acids | Fatty fish, walnuts | Improves hormone production |
Antioxidants | Berries, nuts, dark chocolate | Reduces oxidative stress |
Stress and Psychological Factors
Stress is a big part of the IVF journey. But, too much stress can harm IVF success by affecting hormones and well-being.
Managing Stress:
- Engaging in stress-reducing activities like yoga or meditation
- Seeking support from counselors or support groups
- Practicing mindfulness and relaxation techniques
Toxin Exposure
Environmental toxins can harm reproductive health. It’s important to reduce exposure to these toxins for better IVF outcomes.
Minimizing Toxin Exposure:
- Avoiding endocrine disruptors found in some plastics and personal care products
- Reducing exposure to heavy metals through diet and environment
- Using non-toxic household cleaning products
By choosing a healthy lifestyle and avoiding harmful toxins, we can boost our chances of IVF success.
Moving Forward After Failed IVF Transfers
Dealing with a failed IVF cycle can be tough. But, it’s important to remember it’s not the end. We’re here to help you find your next steps and adjust your treatment plan for a successful pregnancy.
After a failed IVF, figuring out what went wrong is key. Things like the quality of the embryo, how well the uterus accepts it, and any issues with the uterus itself can cause problems. Knowing these can help you and your doctor plan better.
Talking to your fertility specialist about other options is a good idea. You might need to change your treatment plan or try different fertility methods. Our team is here to support you, giving you the care and advice you need to keep moving forward.
It’s okay to feel down after a failed IVF cycle. But, many people and couples have gone on to have successful pregnancies. By understanding the reasons behind implantation failure and making smart choices, you can take the next step towards having a family.
FAQ
Why does IVF fail with good embryos?
IVF can fail even with good embryos for many reasons. These include chromosomal problems, issues with the lining of the uterus, and problems with the shape of the uterus. Immunological factors also play a role.
What are the common causes of IVF failure?
IVF can fail for several reasons. These include genetic issues, poor embryo quality, and problems with the uterine lining. Uterine shape issues and male fertility problems, like sperm DNA damage, are also common causes.
How does maternal age affect IVF success?
Maternal age is a big factor in IVF success. As women get older, egg quality goes down. This increases the chance of genetic problems and lowers the success rate of IVF.
What is the impact of uterine anatomical abnormalities on IVF?
Uterine shape issues, like fibroids or polyps, can hurt IVF success. They can make it harder for embryos to implant and increase the risk of failure.
Can lifestyle and environmental factors influence IVF success?
Yes, lifestyle and environmental factors can affect IVF success. Things like diet, weight, stress, and exposure to toxins can impact outcomes. Making smart lifestyle choices can help improve IVF success.
What are the technical and procedural factors that can influence IVF outcomes?
Technical and procedural factors also play a role in IVF success. This includes the method of embryo transfer, lab conditions, and when the transfer happens. Improving these can help increase success rates.
Why do IVF transfers fail?
IVF transfers can fail for many reasons. These include problems with the embryo, issues with the uterine lining, and shape problems in the uterus. Immunological factors can also be a cause.
What is recurrent implantation failure?
Recurrent implantation failure is when embryos fail to implant, even with good-quality embryos. It can be caused by various factors, including immune and molecular issues.
How can immunological factors contribute to IVF failure?
Immunological factors, like autoimmune conditions and high natural killer cells, can affect IVF success. They can make it harder for embryos to implant and increase the risk of failure.
What are the options available after failed IVF transfers?
After failed IVF transfers, there are several options. People can try adjusting their treatment, look into other fertility options, or seek support to move forward.
References
National Health Service (NHS). Evidence-Based Medical Guidance. Retrieved from https://www.nhs.uk/medicines/clomifene/