
Heart health is key to feeling good overall. Yet, many face a silent danger: blocked coronary arteries. This can cause sudden heart attacks or severe chest pain. At Liv Hospital, we tackle this with the newest medical methods.
Stents are small mesh tubes that help open up blocked or narrowed arteries. This is often because of atherosclerosis, where plaque builds up inside the artery walls. When heart arteries get too narrow, they can’t carry enough blood. This leads to chest pain or even a heart attack.
Knowing why do people need stents helps patients understand their heart health better. Our team at Liv Hospital follows international standards and puts patients first, deciding if a stent is right for each person.
Key Takeaways
- Stents are used to reopen and support narrowed or blocked coronary arteries.
- Atherosclerosis is a common cause of artery narrowing.
- Severely narrowed arteries can lead to chest pain or heart attacks.
- Liv Hospital experts use the latest protocols to determine the necessity of a stent.
- Patient-centered care is a priority at Liv Hospital.
Understanding Coronary Artery Disease and Heart Health
The health of our coronary arteries is key to a healthy heart. These arteries carry blood to the heart muscle, helping it work right. If they get sick, it can cause serious problems like heart attacks.
How Healthy Coronary Arteries Function
Healthy coronary arteries are flexible and let blood flow freely to the heart. They have a thin layer of cells that helps control blood flow and stops clots. These arteries branch from the aorta and wrap around the heart, giving it the oxygen and nutrients it needs.
The Development of Atherosclerosis
Atherosclerosis is what leads to coronary artery disease. It’s when plaque, made of fat, cholesterol, and more, builds up in the arteries. This can narrow the arteries and cut off blood flow to the heart.
This process starts with damage to the artery lining, often from high blood pressure, smoking, or high cholesterol. Once damaged, plaque can start forming, and the artery gets inflamed. As the plaque grows, it narrows the artery, reducing blood flow to the heart muscle.
Risk Factors for Coronary Artery Disease
Several things can increase the risk of coronary artery disease. These include:
- High Blood Pressure: High blood pressure can damage the artery lining and raise the risk of atherosclerosis.
- High Cholesterol: Too much LDL cholesterol can help plaque form.
- Smoking: Smoking harms the heart and increases the risk of atherosclerosis.
- Diabetes: Diabetes can damage blood vessels and nerves, raising the risk of heart disease.
- Family History: A family history of heart disease can up your risk.
- Obesity and Physical Inactivity: Being overweight and not active can lead to several heart disease risks.
| Risk Factor | Description | Impact on Heart Health |
| High Blood Pressure | High blood pressure that can damage blood vessels. | Increases the risk of heart disease and stroke. |
| High Cholesterol | Too much LDL cholesterol that can lead to plaque buildup. | Can narrow arteries and reduce blood flow to the heart. |
| Smoking | Damages the heart and increases blood pressure. | Significantly raises the risk of heart disease and cardiovascular events. |
Knowing about these risk factors and how they affect heart health is key. By tackling these factors, people can lower their risk of heart disease and keep their heart healthy.
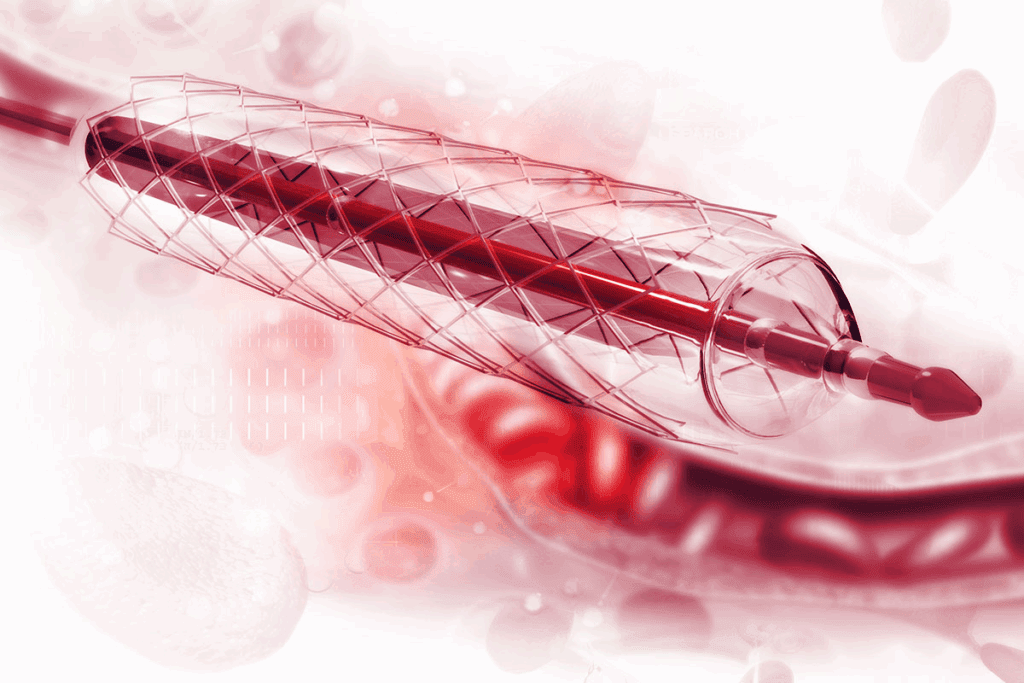
What Are Coronary Stents and How Do They Work?
Coronary stents are key for heart disease patients. They help restore blood flow effectively. These small, mesh-like tubes keep coronary arteries open, improving blood flow to the heart muscle.
Definition and Structure of Cardiac Stents
Coronary stents are made of metal mesh. They are designed to fit into narrowed or blocked coronary arteries. When deployed, they expand, pushing aside blockages to restore blood flow. The mesh design makes them flexible and fits the artery’s shape.
Evolution of Stent Technology
Stent technology has grown a lot over time. At first, bare metal stents were used but they often caused arteries to narrow again. Then, drug-eluting stents came along, releasing medication to prevent this narrowing.
Now, biodegradable stents are being used. They dissolve after doing their job, which might reduce long-term problems.
Different Types of Stents Available Today
There are many types of coronary stents, each with its own advantages:
- Bare Metal Stents: Simple metal mesh stents that provide structural support.
- Drug-Eluting Stents: Stents coated with medication to prevent restenosis.
- Biodegradable Stents: Stents that dissolve over time, potentially reducing long-term risks.
| Type of Stent | Description | Benefits |
| Bare Metal Stents | Simple metal mesh | Structural support, low risk of thrombosis initially |
| Drug-Eluting Stents | Metal mesh with medication coating | Reduces risk of restenosis, improved long-term outcomes |
| Biodegradable Stents | Dissolvable stent material | Reduces long-term complications, innovative technology |
Each stent type has its own use and benefits. The right stent depends on the patient’s condition, the blockage’s severity, and their medical history.
Why Do People Need Stents in Their Heart?
People need stents to get blood flowing to their heart muscle. Coronary arteries can get blocked by plaque. This stops the heart muscle from getting the oxygen and nutrients it needs, causing health problems.
Restoring Blood Flow to Heart Muscle
Stents help keep arteries open. This ensures blood flows well to the heart. It’s key for the heart muscle’s health and preventing damage from lack of oxygen.
The process involves:
- Using a balloon to expand the blocked area
- Deploying a stent to keep the artery open
- Restoring normal blood flow to the heart muscle
Preventing Heart Attacks and Damage
Stents are great at preventing heart attacks. They keep arteries open, lowering the risk of a heart attack caused by blockage.
Key benefits include:
- Reducing the risk of heart attack
- Minimizing damage to the heart muscle
- Improving overall heart health
Relieving Symptoms of Coronary Artery Disease
Stents also ease symptoms of coronary artery disease. This includes chest pain (angina) and shortness of breath.
By restoring blood flow, stents can:
- Reduce the frequency and severity of angina episodes
- Improve exercise tolerance
- Enhance overall quality of life
In conclusion, stents are vital in treating coronary artery disease. They restore blood flow, prevent heart attacks, and ease symptoms. Understanding these benefits helps patients see how important this treatment is.
Warning Signs and Symptoms That May Indicate Need for a Stent
Knowing the warning signs for a stent is key for quick medical help. Heart health is very important. Spotting symptoms that mean you might need a stent can greatly improve treatment results.
Recognizing Angina and Chest Pain Patterns
Angina, or chest pain, is a big sign you might need a stent. It feels like pressure or squeezing in the chest. It can also be felt in the arms, back, neck, jaw, or stomach.
It’s important to know the patterns of angina: it often starts with exertion or stress. Rest or medicine can help ease it. Spotting these patterns can help figure out if you need a stent.
Shortness of Breath and Fatigue
Other signs can also mean you need a stent. Shortness of breath, or dyspnea, happens when the heart doesn’t get enough blood. Feeling unusually tired, or fatigue, can also mean the heart isn’t working right.
These signs might seem small, but they’re big. Shortness of breath and fatigue can hint at heart disease. In some cases, they might mean you need a stent to help your heart and health.
Silent Ischemia: When Symptoms Aren’t Obvious
Sometimes, people have silent ischemia. This is when the heart muscle doesn’t get enough blood, but there’s no chest pain. Silent ischemia is just as risky as angina because it can cause a heart attack without warning.
Regular check-ups and screenings are vital for catching silent ischemia. This is true for people with risk factors for heart disease. We suggest being proactive about your heart health to catch problems early.
Diagnostic Procedures to Determine If You Need a Stent
Doctors use different tests to figure out if you need a stent. These tests show how your coronary arteries are doing. They help doctors know how bad any blockages or damage are. This guides them to the best treatment for you.
Non-Invasive Tests
First, doctors often use non-invasive tests to check for heart disease. Stress tests are common. They see how the heart works when it’s stressed, usually through exercise or medicine. This can show if parts of the heart aren’t getting enough blood.
CT Angiography is another test. It uses X-rays to make detailed pictures of the heart and arteries. It spots blockages and checks the arteries’ health.
Cardiac Catheterization and Angiography
For more detailed info, doctors might suggest cardiac catheterization. This involves putting a catheter into an artery in the leg or arm. It’s then guided to the heart. Doctors use contrast dye to see the arteries on an X-ray, called angiography.
Angiography gives a clear view of blockages in the arteries. It helps doctors figure out if you need a stent.
Measuring Artery Blockage Severity
During angiography, doctors check how bad the blockages are. This is key in deciding if a stent is needed. A blockage is serious if it cuts the artery’s size by 70% or more.
| Diagnostic Test | Description | Invasiveness |
| Stress Test | Evaluates heart function under stress | Non-invasive |
| CT Angiography | Creates detailed images of heart arteries | Non-invasive |
| Cardiac Catheterization | Involves inserting a catheter to visualize arteries | Invasive |
| Angiography | Uses contrast dye to visualize coronary arteries | Invasive |
Emergency Situations: When Stents Are Immediately Necessary
During a heart attack, stents are needed right away to lessen damage. In emergencies like myocardial infarction, unstable angina, and acute coronary syndrome, quick stent use can save lives.
Heart Attack (Myocardial Infarction) Intervention
A heart attack happens when a blockage cuts off blood to the heart for too long. This damages or kills heart muscle. Immediate stent placement is key to getting blood back to the heart, reducing damage.
Thinking about a stent procedure can be scary. But during a heart attack, it’s often the only way to survive. Our team acts fast to check the situation and do the needed procedure to get blood flowing again.
Unstable Angina and Acute Coronary Syndrome
Unstable angina and acute coronary syndrome (ACS) show different levels of heart disease. Unstable angina causes chest pain without effort, showing the heart isn’t getting enough blood. ACS includes both unstable angina and heart attack. Emergency stenting is often needed to keep the heart stable and prevent more damage.
Quick stent use can greatly help by making sure the heart gets the oxygen and nutrients it needs.
Time-Critical Nature of Emergency Stenting
The urgency of emergency stenting is huge. The faster a stent is put in after a heart attack or ACS, the less heart damage there will be. Time is muscle highlights how critical quick treatment is.
We team up with emergency teams and hospitals to get patients the care they need fast. Our aim is to give top-notch care as quickly as we can.
Elective Stent Placement: Criteria and Considerations
Knowing when to use elective stent placement is key for heart health. This procedure is chosen when certain conditions are met. It shows the procedure could greatly help the patient.
Significant Blockage (70% or Greater)
A blockage of 70% or more in a coronary artery is a main reason for stent placement. Such blockages can cut down blood flow to the heart. This might cause symptoms like angina or even heart attacks. Stenting can restore blood flow, easing symptoms and boosting heart health.
Failed Medical Management of Stable Angina
If meds and lifestyle changes don’t control stable angina, stent placement is considered. We check if symptoms are well-managed. If not, stenting might be a good option to control symptoms and improve life quality.
Quality of Life Improvements
The main goal of elective stent placement is to better the patient’s life quality. Stenting can reduce angina symptoms, improve physical ability, and overall well-being. This is key for those whose daily life is affected by heart issues.
Age Considerations for Stent Placement
Age is a big factor in deciding on stent placement. While age isn’t a no-go, older patients have more health issues to consider. We look at overall health, comorbidities, and the procedure’s benefits and risks for each patient, no matter their age.
In summary, elective stent placement is a thoughtful choice based on specific criteria. These include blockage severity, medical management failure, quality of life gains, and patient factors like age. Understanding these points helps patients make informed heart health decisions.
The Stent Placement Procedure: What to Expect
The stent placement procedure is a common treatment for coronary artery disease. Knowing the steps involved can help patients feel more at ease. We know that undergoing a medical procedure can be daunting. But being informed can significantly reduce anxiety.
Preparation for Angioplasty and Stenting
Before the stent placement procedure, patients undergo a series of preparations. These preparations ensure a smooth and successful operation. These preparations include:
- Stopping certain medications that may interfere with the procedure
- Undergoing blood tests to check for any underlying conditions
- Receiving instructions on post-procedure care
- Signing an informed consent form after discussing the risks and benefits with your doctor
It’s essential to follow these instructions carefully. This minimizes any possible risks.
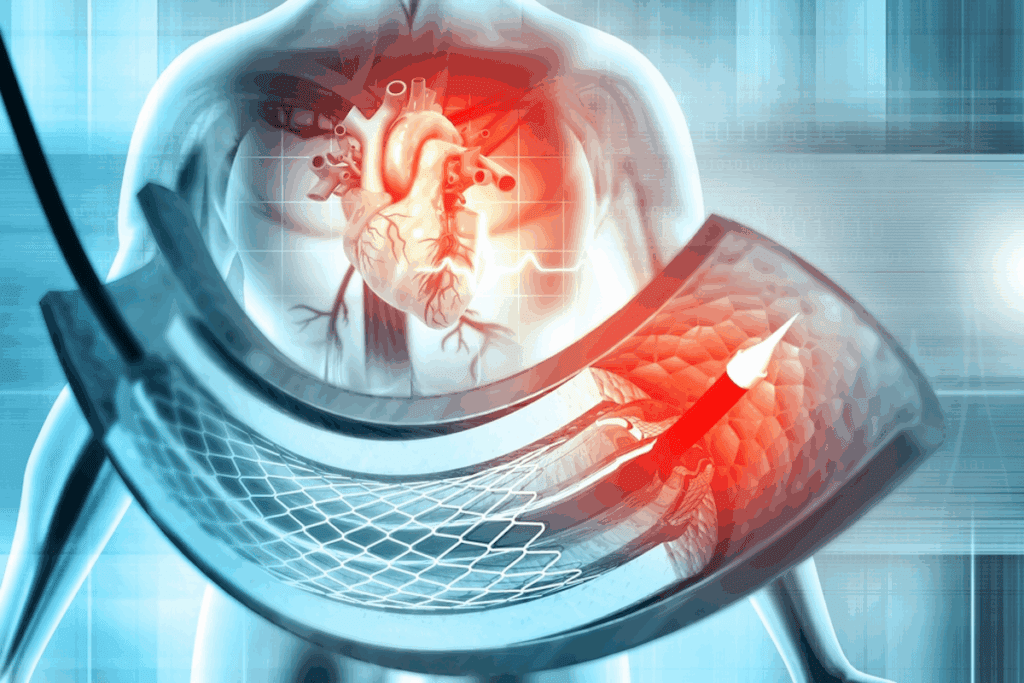
Step-by-Step Process of Stent Deployment
The stent placement procedure involves several key steps:
- Administering Local Anesthesia: The area where the catheter will be inserted is numbed to minimize discomfort.
- Inserting the Catheter: A small incision is made, and a catheter is inserted into the artery.
- Guiding the Catheter: Using X-ray imaging, the catheter is guided to the blocked coronary artery.
- Angioplasty: A balloon on the catheter is inflated to open the blocked artery.
- Stent Deployment: The stent is placed at the site of the blockage and expanded, holding the artery open.
- Removing the Catheter: Once the stent is in place, the catheter is removed, and the incision is closed.
Immediate Post-Procedure Care
After the procedure, patients are monitored in a recovery area for a few hours. Immediate post-procedure care includes:
- Resting to allow the incision site to heal
- Monitoring for any signs of complications
- Receiving instructions on medication, including antiplatelet therapy
- Following a specific recovery plan to ensure a smooth healing process
We emphasize the importance of adhering to the post-procedure instructions. This ensures the stent functions properly and minimizes the risk of complications.
Life After Receiving a Heart Stent
After getting a heart stent, you’ll need to recover, make lifestyle changes, and get ongoing medical care. This ensures the stent works well. Understanding these steps is key to a good outcome.
Recovery Timeline and Expectations
The recovery time after a stent is usually quick. Most people can get back to normal in a few days to a week. But, it depends on your health and the procedure details.
Immediate Recovery (First 24-48 hours): Rest is very important in the first couple of days. Avoid heavy lifting, bending, or hard activities.
Short-Term Recovery (1-2 weeks): You can usually get back to normal in a week or two. Always follow your doctor’s advice on exercise and medicine.
Medication Requirements (Dual Antiplatelet Therapy)
Patients often take two medicines to prevent blood clots on the stent. These are aspirin and a P2Y12 inhibitor, like clopidogrel.
| Medication | Purpose | Duration |
| Aspirin | Antiplatelet effect | Indefinitely |
| P2Y12 Inhibitor | Prevents clot formation on stent | 6-12 months or more |
Lifestyle Modifications for Long-Term Success
Healthy lifestyle choices are important for your stent’s success and heart health. This includes:
- Eating a heart-healthy diet rich in fruits, vegetables, and whole grains
- Engaging in regular physical activity, as recommended by your doctor
- Quitting smoking if you’re a smoker
- Managing stress through techniques like meditation or yoga
Follow-Up Care and Monitoring
Regular check-ups with your doctor are key to watch the stent and heart health. These visits may include:
- Checking for any signs of stent failure or blockage
- Adjusting medications as necessary
- Monitoring for any symptoms or changes in condition
By following the recovery plan, taking your medicines, making lifestyle changes, and going to follow-up visits, you can greatly improve your heart stent outcome.
Conclusion: Making Informed Decisions About Heart Stents
Understanding heart stents is key to making smart choices about treatment. Knowing the good and bad sides helps patients and doctors pick the best plan. This way, patients get the care they need for their health.
We’ve looked at many parts of heart stents, from tests to the procedure itself. Knowing all about it helps patients be more involved in their care. This knowledge lets them make choices that improve their life and health.
When deciding on heart stents, think about your health and disease severity. Also, weigh the benefits and risks of stents. This careful thought ensures patients get the best treatment. It helps them live a healthier, happier life.
FAQ
Why do people need stents in their heart?
People get stents to fix blood flow to the heart. This helps prevent heart attacks and eases symptoms of coronary artery disease.
When is a stent necessary?
You might need a stent if your coronary arteries are blocked by 70% or more. It’s also needed if treatments for stable angina don’t work.
What are the warning signs that may indicate the need for a stent?
Signs you might need a stent include chest pain, shortness of breath, and feeling very tired. Silent ischemia, where you don’t feel symptoms, is also a warning sign.
How do doctors determine if a stent is needed?
Doctors use tests like stress tests and CT angiography to check if you need a stent. They also do cardiac catheterization and angiography.
What is the stent placement procedure like?
Getting a stent involves preparation and a step-by-step process. This includes deploying the stent and care right after.
What is the recovery timeline after receiving a heart stent?
After getting a heart stent, you’ll likely stay in the hospital for a short time. You’ll need to take medication and make lifestyle changes. Follow-up care is also important.
Are there age considerations for stent placement?
Yes, age is a factor when deciding on stent placement. Each case is looked at individually.
Can stents prevent heart attacks?
Yes, stents can stop heart attacks by keeping arteries open. This improves blood flow to the heart.
How do stents work?
Stents keep arteries open, improving blood flow to the heart. This relieves symptoms of coronary artery disease.
What are the different types of stents available?
There are many stent types, including bare metal stents, drug-eluting stents, and biodegradable stents.
Why would someone need a stent in an emergency situation?
In emergencies like heart attacks or unstable angina, stents are used quickly. They’re critical for timely treatment.
How do I know if I need a stent?
To find out if you need a stent, talk to your doctor. They’ll do tests to see how bad your coronary artery disease is.
References
Alebi̇osu, C. O., et al. (2004). Percutaneous renal biopsy as an outpatient procedure. Nigerian Journal of Clinical Practice, 7(2), 56-59. https://pubmed.ncbi.nlm.nih.gov/15481751/

































