Our immune system is meant to protect us. But sometimes, it can go wrong and attack the very things it’s supposed to keep safe. When it attacks our eyes, the results can be very serious and even threaten our sight. Autoimmune eye diseases are a big problem where the body’s defenses fight against the eyes, which can lead to permanent blindness.Wondering why would your immune system attack your eyes? Uncover the shocking causes and triggers behind this serious autoimmune response.
Conditions like uveitis, which is inflammation inside the eye, can happen when the immune system fights off an eye infection or attacks healthy eye tissue. It’s important to understand why this happens to find better treatments and stop vision problems.
Key Takeaways
- The immune system can attack the eyes through autoimmune conditions.
- Uveitis is a common autoimmune eye disease that can cause inflammation.
- Autoimmune eye diseases can lead to permanent vision loss if left untreated.
- Understanding the causes of autoimmune eye diseases is key for effective treatment.
- Early detection and treatment can help prevent vision problems.
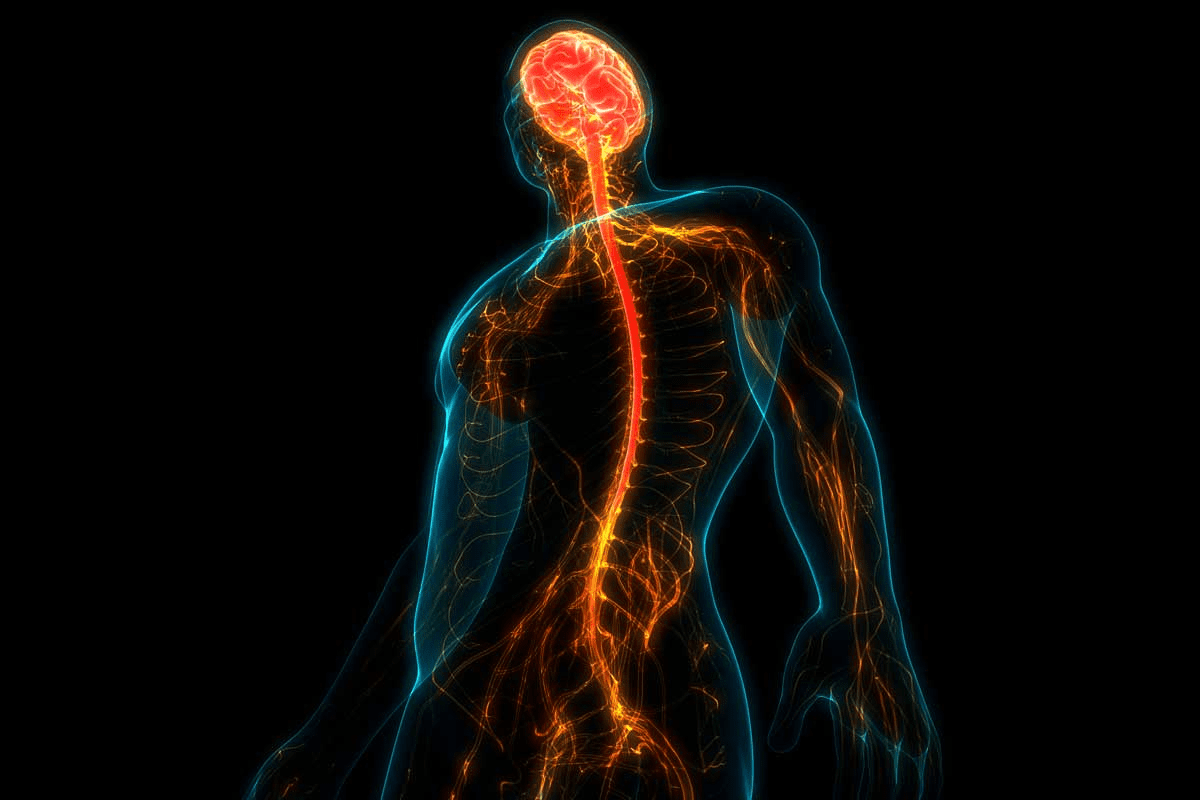
Understanding the Immune System and Ocular Health

Our immune system is like a shield for our body. It fights off infections and diseases. But, it has a special job with our eyes.
The Normal Function of the Immune System
The immune system fights off bad guys like bacteria and viruses. It uses cells, tissues, and organs to do this. Immune cells, such as T cells and B cells, are key in finding and fighting these invaders.
This fight is carefully managed to avoid harming our own body. It’s all about keeping a balance between fighting off threats and calming down the body. If this balance is off, it can cause problems.
Special Immune Privileges of the Eye
The eye is special because it doesn’t let the immune system go wild. This is important for keeping our vision clear, as too much fighting can hurt the eye.
The eye keeps itself safe with special helpers. These helpers calm down the immune system and keep it from getting too excited. This helps the eye stay healthy and avoid problems.
The Blood-Retina Barrier
The blood-retina barrier is a key part of the eye’s safety. It’s made of tight connections that keep things from getting into the retina from the blood. This helps protect the retina from harm.
- The blood-retina barrier keeps bad guys out of the retina, which helps avoid damage.
- It also helps control what gets in and out of the retina, keeping it healthy.
Knowing how the blood-retina barrier works is important. If it gets broken, bad things can get into the retina. This can start an autoimmune reaction in the eye.
When Protection Turns to Attack: Autoimmunity Basics

Autoimmunity happens when the immune system can’t tell the body’s own tissues apart. This can cause various autoimmune diseases, including eye problems. We’ll look into how autoimmunity starts and what makes it happen.
Mistaken Identity: How Autoimmunity Develops
Autoimmunity occurs when the immune system stops recognizing its own cells. Normally, it knows the difference between its own cells and foreign invaders. But in autoimmune diseases, it attacks the body’s own tissues instead.
Key factors in the development of autoimmunity include:
- Genetic predisposition
- Environmental triggers
- Molecular mimicry
Molecular Mimicry and Cross-Reactivity
Molecular mimicry happens when the immune system sees the body’s proteins as foreign because they look like pathogen proteins. This can cause cross-reactivity, where the immune system attacks both the pathogen and the body’s own tissues.
“Molecular mimicry is a key mechanism in the development of autoimmune diseases, as it can trigger an immune response against self-antigens.”
Genetic and Environmental Triggers
Genetics and environment both play big roles in starting autoimmunity. Genetic factors can make someone more likely to get autoimmune diseases. Environmental triggers like infections or chemicals can start the autoimmune response.
Trigger | Description | Example |
Genetic Predisposition | Inherited genetic factors that increase susceptibility to autoimmune diseases | Family history of autoimmune conditions |
Environmental Triggers | External factors that can initiate an autoimmune response | Infections, chemical exposure |
Molecular Mimicry | Immune response to self-antigens due to similarity with pathogen-derived proteins | Cross-reactivity between microbial and host antigens |
Understanding these mechanisms is key to finding treatments for autoimmune eye diseases. By knowing the causes and triggers, we can manage and maybe even prevent these diseases.
Why Would Your Immune System Attack Your Eyes?
It’s important to understand why the immune system might attack the eyes. The eyes need a balance between protection and suppression to work right. This balance keeps them clear and functional.
The Paradox of Ocular Immunity
The eye is special because it’s “immune-privileged.” This means it has ways to avoid too much immune activity. But, sometimes, the immune system can attack the eyes.
Key factors contributing to the paradox of ocular immunity include:
- The blood-retina barrier, which limits the access of immune cells to the retina
- The presence of anti-inflammatory cytokines in the ocular microenvironment
- The expression of immune-modulatory molecules on ocular cells
Breaking of Immune Tolerance
Immune tolerance helps the immune system ignore self-antigens. When this fails, autoimmune diseases can start. In the eyes, this can cause uveitis and autoimmune retinopathy.
Factors that contribute to the breaking of immune tolerance in the eyes include:
- Genetic predisposition
- Environmental triggers, such as infections or injuries
- Molecular mimicry, where immune responses to pathogens cross-react with self-antigens
Common Pathways of Ocular Autoimmunity
Autoimmune eye diseases have common causes. These include the activation of autoreactive T cells and the production of autoantibodies. Pro-inflammatory cytokines also play a role.
Understanding these pathways is key for developing new treatments. These treatments aim to control the immune response and prevent damage. Scientists are working hard to find better ways to help patients.
Uveitis: When Inflammation Targets the Eye’s Middle Layer
Uveitis is a group of eye conditions caused by inflammation in the uvea. This middle layer of the eye has pigmentation and blood supply to the retina. When it gets inflamed, it can cause a lot of pain and serious vision problems.
Types and Classification
Uveitis can be classified in different ways. It depends on which part of the uvea is affected, how long the inflammation lasts, and what causes it. The main types are:
- Anterior Uveitis: This affects the front part of the uvea and is often linked to autoimmune disorders.
- Intermediate Uveitis: It impacts the middle part of the uvea, mostly seen in young adults.
- Posterior Uveitis: This type affects the back part of the uvea and can cause serious vision loss.
- Panuveitis: It involves inflammation of all layers of the uvea.
Symptoms and Progression
The symptoms of uveitis vary based on the type and how severe it is. Common symptoms include:
- Eye pain and redness
- Blurred vision
- Sensitivity to light
- Floaters
Uveitis can be either acute or chronic. Chronic cases can lead to serious complications like cataracts, glaucoma, and retinal damage if not treated properly.
Immune Mechanisms Behind Uveitis
The immune system plays a key role in uveitis. It involves complex interactions of cells and molecules. Autoimmune responses, where the body attacks its own tissues, are a major factor. Understanding these mechanisms is key to finding effective treatments.
Type of Uveitis | Common Associations | Typical Symptoms |
Anterior Uveitis | Autoimmune disorders, infections | Eye pain, redness, sensitivity to light |
Intermediate Uveitis | Multiple sclerosis, infections | Floaters, blurred vision |
Posterior Uveitis | Toxoplasmosis, autoimmune conditions | Vision loss, floaters |
We know that uveitis is a condition where the immune system’s response can harm the eye. By understanding the types, symptoms, and immune mechanisms, we can improve diagnosis and treatment. This is important to prevent sight-threatening complications.
Autoimmune Retinopathy: Attacking the Vision Center
Autoimmune retinopathy happens when the body’s immune system mistakenly sees retinal proteins as invaders. This rare condition causes vision to get worse over time. It greatly affects the quality of life for those who have it.
Anti-Retinal Antibodies
A key sign of autoimmune retinopathy is the presence of anti-retinal antibodies. These antibodies attack various proteins in the retina, disrupting its function. Finding these antibodies is key to diagnosing the condition.
Lab tests can spot anti-retinal antibodies. Knowing about these antibodies helps doctors understand the disease. It also helps them find the right treatments.
Paraneoplastic and Non-Paraneoplastic Forms
Autoimmune retinopathy comes in two main types: paraneoplastic and non-paraneoplastic. The paraneoplastic form is linked to cancer. The immune system attacks the tumor and also the retina.
The non-paraneoplastic form doesn’t have cancer. Both types have similar symptoms, making it hard to tell them apart.
Characteristics | Paraneoplastic Autoimmune Retinopathy | Non-Paraneoplastic Autoimmune Retinopathy |
Association with Cancer | Yes | No |
Immune Response | Cross-reacts with retinal antigens | Targets retinal proteins |
Diagnostic Approach | Involves cancer screening | Based on clinical features and antibody tests |
Diagnostic Challenges
Diagnosing autoimmune retinopathy is hard because it’s rare and looks like other eye problems. Doctors use a detailed approach. This includes checking the patient, testing for antibodies, and imaging.
Because of these challenges, a team of experts is needed. Ophthalmologists, immunologists, and others work together. They make sure the diagnosis is right and treatment is effective.
Susac Syndrome: When Blood Vessels Become Targets
The immune system is meant to protect us. But in Susac syndrome, it attacks the blood vessels in the eyes, brain, and ears. This rare condition causes inflammation in small blood vessels, leading to serious problems.
The Clinical Triad: Eyes, Brain, and Ears
Susac syndrome shows up in a unique way. It includes encephalopathy, branch retinal artery occlusions, and hearing loss. Not all symptoms appear at once, making it hard to diagnose.
Encephalopathy can cause brain problems and mental issues. Branch retinal artery occlusions affect vision. Hearing loss, which can change, is also a big worry for those affected.
“The symptoms of Susac syndrome can vary a lot,” doctors say. “It needs a strong suspicion to diagnose.”
Retinal Vessel Occlusion Mechanisms
In Susac syndrome, the immune system blocks retinal vessels. This can cause damage and vision loss. How it happens is not fully understood, but autoantibodies are thought to play a big part.
Diagnostic Imaging and Findings
Imaging is key in spotting Susac syndrome. Fluorescein angiography shows blocked retinal vessels. MRI reveals brain lesions. These tools, along with symptoms, help confirm the diagnosis. Audiometry checks for hearing loss.
Diagnosing Susac syndrome takes a team effort. Ophthalmologists, neurologists, and audiologists work together. Early treatment is vital to avoid lasting harm.
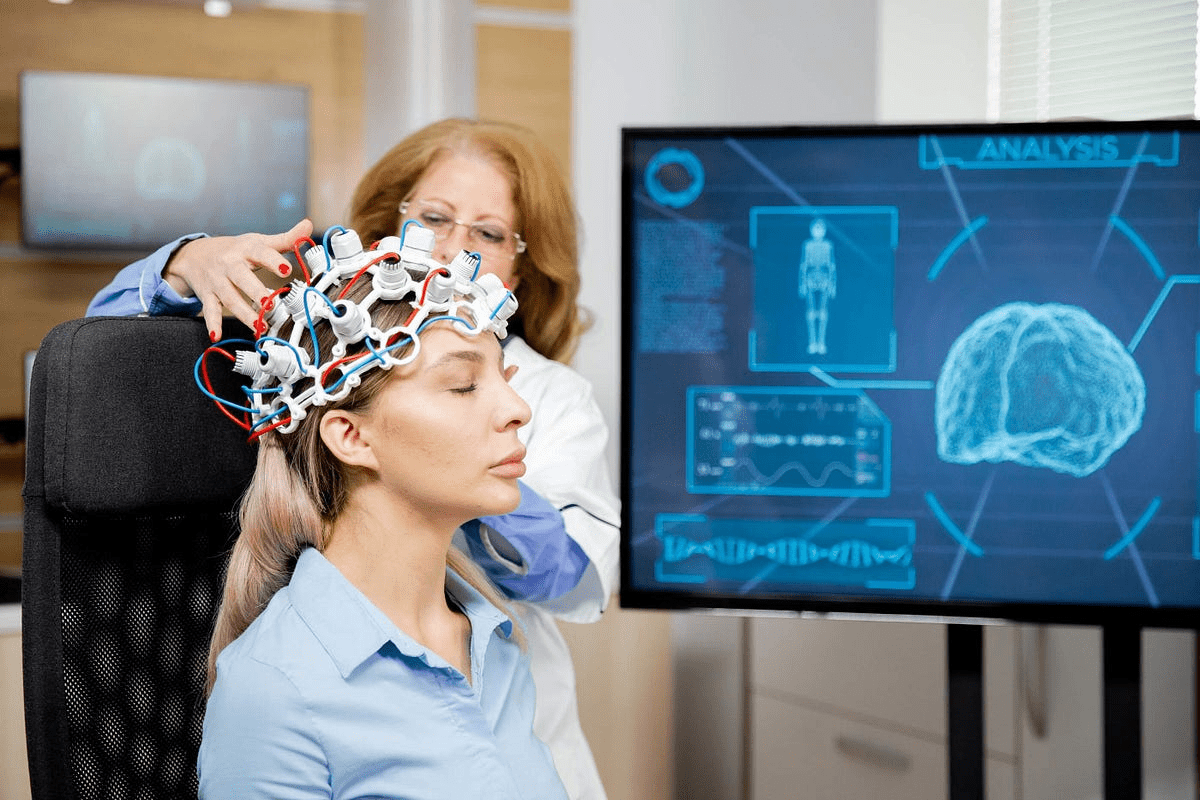
Neuromyelitis Optica: Aquaporin-4 Under Attack
Neuromyelitis optica, also known as Devic’s disease, is when the immune system attacks the aquaporin-4 protein. This leads to severe optic neuritis and myelitis. It greatly affects patients’ vision and mobility.
The Role of NMO-IgG Antibodies
NMO-IgG antibodies are key in neuromyelitis optica. They target the aquaporin-4 water channel protein on astrocytes. These antibodies help doctors tell neuromyelitis optica apart from other diseases like multiple sclerosis.
Research shows NMO-IgG antibodies cause inflammation and damage. This damage affects the optic nerve and spinal cord.
Testing for NMO-IgG antibodies is important for diagnosing neuromyelitis optica. Advanced tests help doctors make the right diagnosis.
Optic Neuritis and Visual Outcomes
Optic neuritis is common in neuromyelitis optica. It causes inflammation in the optic nerve. This can lead to severe vision loss, even blindness.
The impact of optic neuritis on vision is critical. Early treatment can help save vision and prevent long-term loss.
Distinguishing from Multiple Sclerosis
Neuromyelitis optica and multiple sclerosis are both autoimmune diseases. But they have different symptoms and treatments. Neuromyelitis optica mainly affects the optic nerve and spinal cord.
- Clinical Presentation: Neuromyelitis optica often has severe optic neuritis and spinal cord inflammation. Multiple sclerosis has more widespread lesions.
- Imaging and Diagnostic Tests: MRI and NMO-IgG antibodies help tell them apart.
- Treatment Approaches: Neuromyelitis optica treatment focuses on reducing antibodies and inflammation. Multiple sclerosis treatments aim to slow the disease and manage symptoms.
Getting the right diagnosis is key for proper treatment. Knowing the differences between neuromyelitis optica and multiple sclerosis is important for better patient care.
Other Autoimmune Conditions Affecting the Eyes
Many autoimmune diseases can harm your eyes and vision. These conditions need a detailed plan to manage their effects on your eyes.
Graves’ Ophthalmopathy
Graves’ ophthalmopathy is linked to Graves’ disease. It affects the eye’s tissues, like the eyelids and lacrimal gland. This can cause bulging eyes, double vision, and even vision loss.
Managing Graves’ ophthalmopathy requires a team effort. This includes medicines to reduce swelling and sometimes surgery to relieve pressure.
Sjögren’s Syndrome and Dry Eyes
Sjögren’s syndrome is an autoimmune disease known for dry eyes and mouth. It happens when the glands, like the lacrimal and salivary glands, get inflamed.
Dry eyes from Sjögren’s can cause discomfort and vision problems. It also raises the risk of eye infections. Early diagnosis and treatment are key. This may include artificial tears, medicines, and plugs to keep tears in.
Rheumatoid Arthritis-Related Eye Complications
Rheumatoid arthritis (RA) mainly affects joints but can also harm the eyes. People with RA might get conditions like scleritis, episcleritis, and peripheral ulcerative keratitis.
These eye problems can be serious and threaten your sight. Regular eye checks are vital for RA patients. They help catch early signs and start treatment quickly.
Multiple Sclerosis and Optic Neuritis
Multiple sclerosis (MS) is an autoimmune disease that affects the central nervous system, including the optic nerves. Optic neuritis, inflammation of the optic nerve, is a common symptom of MS. It can cause vision loss, eye pain, and color changes.
Managing MS and its eye problems requires treatments to slow disease progression. For optic neuritis, corticosteroids are often used to help recovery.
Condition | Ocular Manifestations | Management Approaches |
Graves’ Ophthalmopathy | Exophthalmos, double vision, vision loss | Anti-inflammatory medications, surgical decompression |
Sjögren’s Syndrome | Dry eyes, vision disturbances, eye infections | Artificial tears, anti-inflammatory medications, punctal plugs |
Rheumatoid Arthritis | Scleritis, episcleritis, peripheral ulcerative keratitis | Regular eye exams, timely treatment of complications |
Multiple Sclerosis | Optic neuritis, vision loss, altered color perception | Disease-modifying therapies, corticosteroids for optic neuritis |
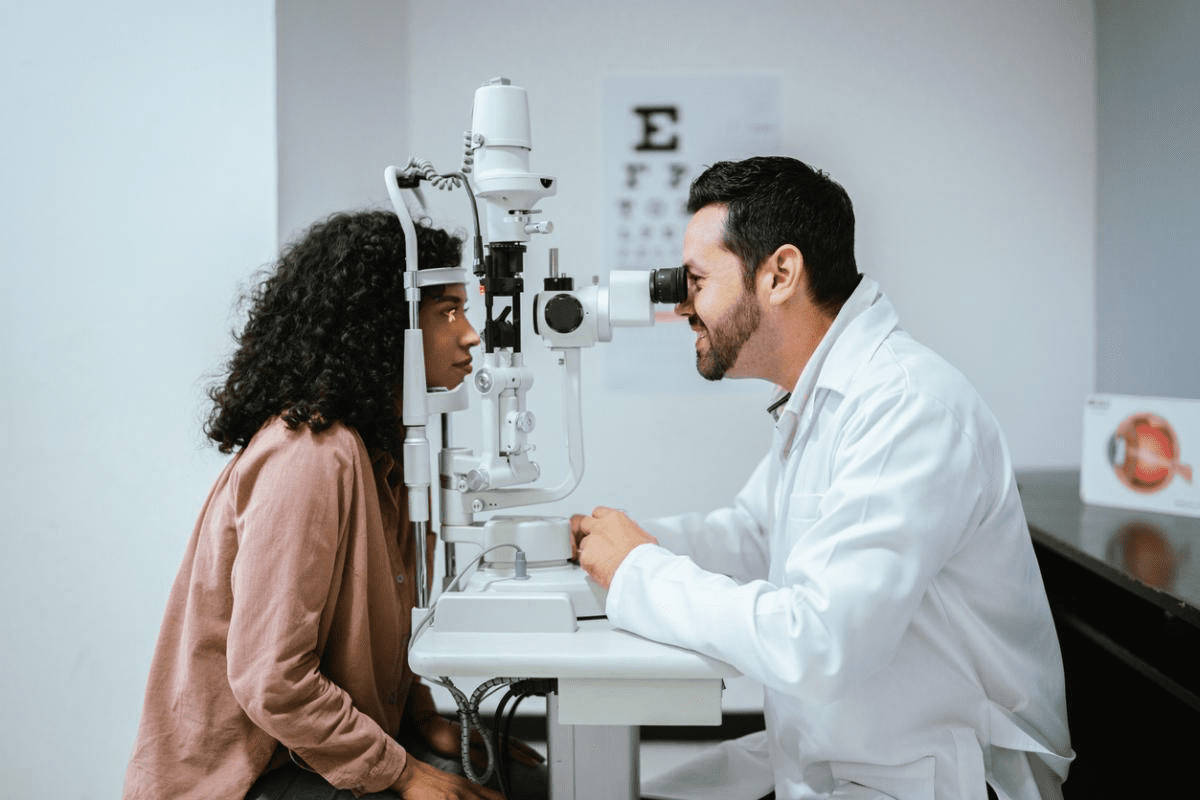
Diagnosis of Ocular Autoimmune Conditions
To diagnose ocular autoimmune disorders, doctors use a mix of clinical skills, lab tests, and advanced imaging. This detailed method is key to spotting the eye problems caused by autoimmune diseases.
Clinical Evaluation and History
Diagnosing ocular autoimmune conditions starts with a detailed patient history. We look for symptoms like vision changes, eye pain, and light sensitivity. Then, we do a thorough eye exam to check vision, eye movement, and eye structure.
Laboratory Testing for Autoantibodies
Lab tests are vital for spotting autoimmune eye diseases. We test for specific autoantibodies linked to different conditions. For example, the ANA test can show if systemic diseases like lupus or rheumatoid arthritis are affecting the eyes.
- Common Autoantibody Tests:
- Antinuclear Antibody (ANA) Test
- Rheumatoid Factor (RF) Test
- Anti-Retinal Antibody Tests
Imaging Techniques
Advanced imaging is key for diagnosing and tracking ocular autoimmune conditions. We use:
- Optical Coherence Tomography (OCT): Gives detailed images of the retina and optic nerve.
- Fluorescein Angiography: Shows how well the retinal blood vessels are working and if there’s leakage.
- Ultrasonography: Helps see the back of the eye when it’s cloudy.
Differential Diagnosis Challenges
Figuring out the right diagnosis for ocular autoimmune conditions can be tough. Symptoms can look like other eye or body diseases. We must think about many conditions to get it right.
By using clinical skills, lab tests, and imaging, we can accurately diagnose and treat ocular autoimmune conditions. This helps patients keep their vision and improves their health.
Treatment Approaches for Immune-Mediated Eye Disorders
There are many ways to treat immune-mediated eye disorders. These treatments aim to reduce inflammation and protect vision. The right treatment depends on the condition, its severity, and the patient’s health.
Corticosteroids and Anti-Inflammatory Medications
Corticosteroids are often the first choice for treating these disorders. They work well because they reduce inflammation. They can be applied directly to the eye, injected, or taken by mouth, based on the condition’s severity.
But, using corticosteroids for a long time can cause problems. These include cataracts, glaucoma, and a higher chance of infections.
Table 1: Corticosteroid Administration Routes and Their Implications
Administration Route | Advantages | Disadvantages |
Topical | Targeted delivery, fewer systemic side effects | Limited to superficial conditions, possible local side effects |
Oral | Systemic effect, good for severe or both eyes | More risk of side effects, needs careful watch |
Injection | Direct to the area, quick action | More invasive, risk of infection or other issues |
Immunosuppressive Therapies
For long-term treatment or severe cases, immunosuppressive therapies are used. These drugs weaken the immune system. This reduces inflammation and damage. Common drugs include methotrexate, cyclosporine, and azathioprine.
Biologics and Targeted Treatments
Biologic agents are a newer type of treatment. They target specific parts of the immune response. Drugs like TNF-alpha inhibitors (e.g., infliximab, adalimumab) are effective against uveitis and scleritis. They offer targeted therapy with fewer side effects than traditional drugs.
Managing Symptoms and Complications
It’s also important to manage symptoms and complications. This includes treatments for pain, inflammation, and vision correction. Sometimes, surgery is needed for issues like cataracts or retinal detachment.
By treating the condition and its symptoms, we can greatly improve patients’ lives. This approach helps them live better with immune-mediated eye disorders.
Conclusion: Living with Ocular Autoimmune Disease
Living with ocular autoimmune disease means having a detailed plan to keep your vision and life quality good. It’s key to know why the immune system attacks the eyes to find the right treatments.
Getting a diagnosis early and the right treatment is very important. We need to work together to help those with these diseases keep their vision. This will make a big difference in their lives.
Teaching patients about their disease and involving them in their care is also very important. This way, they can take charge of their health and make smart choices about their treatment.
As we learn more about the immune system and eyes, we can find better treatments for these diseases. This will help us manage these conditions better and improve the lives of those affected by autoimmune disease.
FAQ
Does the immune system know I have eyes?
Yes, the immune system knows we have eyes. But it usually doesn’t attack them. The eye has special protection that keeps it safe from too much inflammation.
Why does the immune system attack the eyes in autoimmune conditions?
In autoimmune conditions, the immune system gets confused. It sees healthy eye tissues as threats. This leads to inflammation and can cause vision loss.
What is the role of the blood-retina barrier in ocular immunity?
The blood-retina barrier is key in keeping the eye safe. It controls what moves between the blood and the retina. This helps prevent too much inflammation.
What is uveitis, and how is it related to autoimmune responses?
Uveitis is when the uvea gets inflamed. It’s often linked to autoimmune responses. In these cases, immune cells attack healthy eye tissue, causing inflammation and vision problems.
Can autoimmune conditions like rheumatoid arthritis affect the eyes?
Yes, conditions like rheumatoid arthritis can harm the eyes. So can Graves’ ophthalmopathy, Sjögren’s syndrome, and multiple sclerosis. These can cause various eye problems.
How are autoimmune eye conditions diagnosed?
Doctors use many ways to diagnose these conditions. They do a full check-up, test for autoantibodies, and use advanced imaging. They also compare symptoms to find the right diagnosis.
What are the treatment approaches for immune-mediated eye disorders?
Treatment includes using corticosteroids and immunosuppressive drugs. Biologics and targeted treatments are also used. The goal is to manage symptoms and improve quality of life.
Is autoimmune retinopathy a common condition?
Autoimmune retinopathy is rare. It happens when the immune system attacks the retina. This can lead to vision loss. Diagnosing it can be hard because it’s similar to other eye conditions.
What is Susac syndrome, and how does it affect the eyes?
Susac syndrome is a rare condition. It affects the retina, brain, and inner ear. It can cause retinal vessel occlusion and vision loss.
How does neuromyelitis optica affect the eyes?
Neuromyelitis optica is a severe condition. It affects the optic nerve and spinal cord. NMO-IgG antibodies play a big role in its development. It can cause significant vision loss.
Can the immune system be modulated to prevent attacks on the eyes?
Yes, treatments aim to control the immune system. This helps prevent it from attacking the eyes. Immunomodulatory therapies and biologics are used for this purpose.
Does the brain know I have eyes?
Yes, the brain knows we have eyes. It processes the visual information from them. This is important for understanding what we see.
How do genetic and environmental factors contribute to autoimmune eye diseases?
Genetics and environment play a role in these diseases. They can affect how the immune system reacts to eye tissues. This can lead to autoimmune eye diseases.
What is the paradox of ocular immunity?
The paradox of ocular immunity is about balance. The eye needs to protect itself from harm. But it also can’t let inflammation damage its delicate tissues.
Are there different forms of autoimmune retinopathy?
Yes, there are different types of autoimmune retinopathy. There’s paraneoplastic and non-paraneoplastic forms. Each has its own causes and treatment options.
References
National Center for Biotechnology Information. Autoimmune Eye Disease: When Immunity Turns Inward. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK459445/