Crohn’s disease is a chronic inflammatory bowel condition that affects millions worldwide. It causes significant discomfort and impacts quality of life chrome disease.
We understand the importance of this complex condition. It can affect any part of the digestive tract. At Liv Hospital, we use international expertise and patient-centered innovation to manage it. We ensure individuals get the best care and diagnostic protocols.
As a leading healthcare provider, we are dedicated to supporting international patients. We help those seeking advanced medical treatments.
Key Takeaways
- Crohn’s disease is a chronic inflammatory bowel condition.
- It can affect any segment of the digestive tract.
- Understanding the condition is key for effective management.
- Liv Hospital provides complete care and innovative treatments.
- International expertise is available for patients seeking advanced care.
What is Crohn’s Disease?
Crohn’s disease, also known as maladie de Crohn, is a type of inflammatory bowel disease (IBD). It can affect any part of the gastrointestinal tract. Symptoms include abdominal pain, diarrhea, fever, and weight loss.
Definition and Classification
Crohn’s disease can affect any part of the GI tract, from mouth to anus. It often hits the terminal ileum and the colon’s start. Knowing Crohn’s disease definition and how it’s classified helps doctors choose the right treatment.
Historical Context and Discovery
The history of Crohn’s disease began in the early 20th century. Medical Expert. Crohn and his team first described it in 1932. They called it “regional ileitis” because it often occurred in the ileum.
As more was learned, it became clear it could affect any GI tract part. This led to a broader understanding and the name Crohn’s disease, honoring Medical Expert’s work.
Key Fact #1: The Prevalence of Crohn’s Disease in America
Recent data shows a big impact of Crohn’s disease on America’s healthcare. Many Americans are dealing with this inflammatory bowel condition.
Current Statistics
About 1.011 million Americans have Crohn’s disease, estimates say. This means 305 people out of every 100,000 have it. It shows how common this condition is.
Prevalence Rate
The rate of 305 cases per 100,000 people shows Crohn’s disease is a big health issue in the U.S. We need to think about this when planning healthcare and treatments.
Knowing how common Crohn’s disease is helps everyone involved. It helps us plan better, create effective treatments, and improve care for patients.
Key Fact #2: Global Epidemiology Trends
Crohn’s disease is changing, with more cases in industrialized countries and new patterns in others. This change shows the disease’s growing impact worldwide. It’s important to understand its spread.
Rising Incidence in Industrialized Nations
Industrialized countries have seen more Crohn’s disease cases for a long time. The numbers keep going up.
- North America: The United States and Canada have some of the highest rates, with about 1.011 million Americans affected.
- Europe: Northern European countries have higher rates than Southern ones, but the difference is getting smaller.
- Oceania: Australia and New Zealand also have high rates, similar to North America and Northern Europe.
The reasons for this increase include genetic predisposition, environmental triggers, and lifestyle changes. Knowing these helps in finding better ways to fight the disease.
Emerging Patterns in Newly Industrialized Countries
Newly industrialized countries are seeing more Crohn’s disease, marking a shift in global trends.
- Rapid Urbanization: Countries quickly changing to cities and new lifestyles are seeing more cases.
- Changing Dietary Patterns: Taking on Western diets is thought to play a role in the increase.
- Increased Awareness: Better diagnosis and more doctors knowing about the disease also add to the numbers.
As Crohn’s disease spreads worldwide, it’s key to grasp these new trends. This helps healthcare systems get ready for the disease’s growing impact.
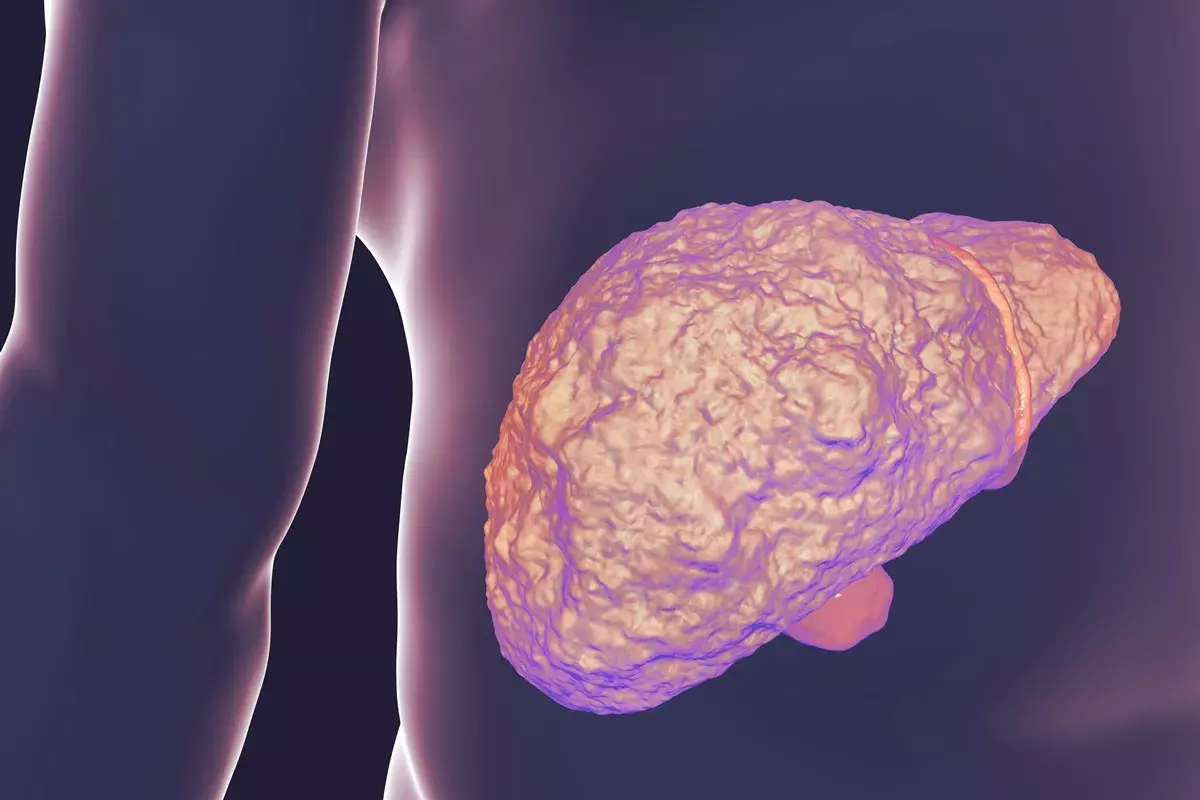
Key Fact #3: How Crohn’s Disease Affects the Digestive Tract
It’s important to know how Crohn’s Disease impacts the digestive tract. This knowledge helps manage symptoms and slow the disease’s progress. The small intestine and the start of the colon are most often affected.
Primary Target Areas: Small Intestine and Proximal Colon
The small intestine, mainly the ileum, is a key area for Crohn’s Disease. The start of the large intestine, or proximal colon, is also commonly hit. The disease leads to chronic inflammation, causing pain, diarrhea, and weight loss.
Patchy Inflammation Patterns
Crohn’s Disease is known for its patchy inflammation. It can affect different parts of the digestive tract, leaving some areas untouched. This pattern can cause the intestine to narrow and fistulas to form.
We’ll look at these complications and how to manage them later. But knowing how Crohn’s Disease affects the digestive tract is key.
Key Fact #4: Symptoms and Clinical Manifestations
It’s important for both patients and doctors to know the symptoms of Crohn’s disease. This knowledge helps in managing the condition well. The symptoms can vary a lot from person to person, making it hard to diagnose and treat.
Primary Digestive Symptoms
The main digestive symptoms of Crohn’s disease are abdominal pain, diarrhea, weight loss, and feeling very tired. These happen because the disease causes inflammation in the gut.
- Abdominal Pain: Pain is often in the lower right abdomen but can be anywhere.
- Diarrhea: Persistent diarrhea is common, sometimes with blood or mucus.
- Weight Loss: Unintentional weight loss happens because the body can’t absorb nutrients well.
- Fatigue: Feeling very tired is a common complaint among patients.
Extraintestinal Manifestations
Crohn’s disease can also show up outside the digestive system. These symptoms can include:
Manifestation | Description |
Arthritis | Joint pain and inflammation, often affecting large joints. |
Skin Rashes | Erythema nodosum and pyoderma gangrenosum are common skin manifestations. |
Eye Problems | Uveitis and episcleritis can occur, potentially leading to vision problems. |
These symptoms show that Crohn’s disease affects more than just the gut. It can affect other parts of the body too. Treating these symptoms requires a full treatment plan.
Key Fact #5: Risk Factors and Genetic Predisposition
It’s important to know the risk factors and genetic predisposition for Crohn’s disease. This knowledge helps in early diagnosis and better management. Both hereditary and environmental factors are key in developing this condition.
Hereditary Components
Crohn’s disease has a strong genetic link. Certain genetic markers increase the risk of getting the disease. Studies have found many genetic loci linked to Crohn’s disease risk.
People with a family history of the disease are more likely to get it. This shows how important genetics are.
Key genetic factors include:
- Mutations in the NOD2/CARD15 gene
- Variations in the IL23R gene
- Other genetic loci identified through genome-wide association studies
Environmental Triggers
Genetics are not the only factor. Environmental factors also play a big role in Crohn’s disease. Smoking is a major risk factor, making smokers more likely to get the disease and have worse symptoms. Other possible triggers include diet, stress, and changes in gut microbiota.
- Smoking
- Diet high in processed foods and low in fiber
- Stress and psychological factors
Knowing these risk factors and genetic predispositions helps in finding better treatments and prevention strategies. By identifying high-risk individuals and changing environmental factors, we can lower the disease’s incidence and severity.
Diagnostic Approaches and Testing Methods
Diagnosing Crohn’s disease requires a detailed approach. It includes lab tests, imaging, and endoscopy. This method is key to finding the right treatment.
Laboratory Tests and Biomarkers
Laboratory tests are essential in diagnosing Crohn’s disease. They check for inflammation and infection. Important tests include:
- Complete Blood Count (CBC) to check for anemia and infection
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP) to assess inflammation levels
- Stool tests to rule out infections that may cause similar symptoms
Biomarkers like fecal calprotectin help track intestinal inflammation. A study found that fecal calprotectin is useful for monitoring Crohn’s disease.
“Fecal calprotectin has emerged as a valuable tool in the management of Crohn’s disease, allowing for non-invasive monitoring of intestinal inflammation.”
Gastroenterology Research
Imaging and Endoscopic Procedures
Imaging and endoscopy are vital for seeing the extent of Crohn’s disease. These tools include:
- Colonoscopy to directly visualize the colon and ileum
- Computed Tomography (CT) scans and Magnetic Resonance Imaging (MRI) to assess the extent of disease and detect complications
- Endoscopic ultrasound to evaluate the layers of the intestinal wall
Using lab tests, imaging, and endoscopy together helps doctors accurately diagnose Crohn’s disease. A medical expert says, “The integration of laboratory tests, imaging studies, and endoscopic evaluations is essential for accurate diagnosis and management of Crohn’s disease.“
Treatment Strategies for Crohn’s Disease
Crohn’s disease treatment combines medication and surgery. It’s all about helping the patient feel better and live a good life.
Medication Therapies
Medicine is key in fighting Crohn’s disease. There are several types of drugs used:
- Aminosalicylates to reduce inflammation
- Corticosteroids for short-term control of flare-ups
- Immunomodulators to suppress the immune system
- Biologics targeting specific proteins involved in inflammation
Doctors pick the right mix of medicines based on how bad the disease is.
Medication Type | Primary Use | Examples |
Aminosalicylates | Mild to moderate Crohn’s disease | Mesalamine, Sulfasalazine |
Corticosteroids | Short-term control of flare-ups | Prednisone, Budesonide |
Immunomodulators | Maintaining remission | Azathioprine, Mercaptopurine |
Biologics | Moderate to severe Crohn’s disease | Infliximab, Adalimumab |
Surgical Interventions
Surgery is needed for serious problems like strictures and fistulas. It can fix these issues by removing the bad part of the bowel or fixing fistulas.
Even with surgery, Crohn’s disease can come back. So, patients usually need to keep seeing doctors for treatment.
Living with Crohn’s Disease: Lifestyle Management
Living with Crohn’s disease can be tough, but the right lifestyle can help. It’s all about making smart choices in diet, managing stress, and using support resources.
Dietary Considerations and Nutritional Support
Diet is key in managing Crohn’s disease. Patients often need to change their eating habits to feel better. Important dietary tips include:
- Avoiding foods that make symptoms worse
- Eating a balanced diet to get enough nutrients
- Using nutritional supplements if needed
Getting help from a healthcare provider or dietitian can create a diet plan that works for you.
Stress Management Techniques
Stress can make Crohn’s disease symptoms worse. So, finding ways to manage stress is important. Good stress management strategies are:
- Meditation and mindfulness
- Exercise that fits your health
- Cognitive-behavioral therapy (CBT)
Support Resources and Patient Communities
Connecting with others who have Crohn’s disease can offer emotional support and advice. Benefits include:
- Joining support groups
- Using online forums and resources
- Attending educational programs
By using these lifestyle strategies, people with Crohn’s disease can manage their condition better. This can greatly improve their quality of life.
Conclusion: Advances in Understanding and Managing Crohn’s Disease
Crohn’s disease is a complex condition that affects millions globally. It’s also known as regional enteritis or ileitis. Managing it requires a detailed approach.
We’ve looked at key facts about Crohn’s disease. This includes its prevalence, how it affects the digestive tract, symptoms, and risk factors. Research has improved diagnosis and treatment, helping those with the disease live better lives.
Effective management of Crohn’s disease involves medication, lifestyle changes, and sometimes surgery. Ongoing research is finding new ways to treat the condition. This leads to better outcomes for patients.
In summary, while Crohn’s disease is challenging, progress in understanding and managing it offers hope. By staying informed and involved, we can improve care and support for those affected.
FAQ
What is Crohn’s disease?
Crohn’s disease is a chronic condition that causes inflammation in the digestive tract. It can affect any part of the gut but often hits the lower small intestine, called the ileum.
What are the symptoms of Crohn’s disease?
Symptoms vary but include diarrhea, stomach pain, and feeling tired. People might also lose weight and have less appetite. Some experience joint pain, skin issues, and eye problems too.
What causes Crohn’s disease?
The exact cause is unknown but it’s thought to be a mix of genetics, environment, and immune system issues. Stress, diet, and some medicines can make it worse.
How is Crohn’s disease diagnosed?
Doctors use medical history, physical checks, lab tests, and imaging to diagnose. Endoscopy and biopsies help confirm and see how far the disease has spread.
What are the treatment options for Crohn’s disease?
Treatment includes medicines, lifestyle changes, and sometimes surgery. Medicines like aminosalicylates and biologics are used. Surgery might be needed to remove damaged parts of the intestine.
Can Crohn’s disease be cured?
There’s no cure but with the right treatment, many people manage well. The goal is to control symptoms and prevent complications.
How can I manage Crohn’s disease?
Managing it means following treatment plans, eating right, managing stress, and staying informed. Support from doctors, patient groups, and loved ones is key.
Is Crohn’s disease the same as ulcerative colitis?
No, they are different types of inflammatory bowel disease. Crohn’s can affect any part of the gut, while ulcerative colitis mainly hits the colon.
Can diet affect Crohn’s disease?
Yes, diet is important. Some foods can trigger or worsen symptoms. Eating a balanced, easy-to-digest diet and taking supplements can help manage it.
What is the prevalence of Crohn’s disease?
It affects about 1.6% of the world’s population. In the U.S., it’s estimated that 780,000 to 1 million people have it.
References:
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3268785/