Last Updated on November 27, 2025 by Bilal Hasdemir
For those dealing with brain or spinal fluid buildup, shunt procedures can change lives. At Liv Hospital, we offer trusted care and top-notch results. We make sure you get the newest treatments and the best shot at long-term health.
Conditions like hydrocephalus need surgery to drain extra cerebrospinal fluid (CSF). This helps avoid high pressure on the brain or spinal cord. We use the latest in medical imaging and navigation systems to boost surgery success. Our team is dedicated to giving full care to patients from around the world looking for top medical treatments.
Key Takeaways
- Modern shunt procedures can greatly improve life quality for those with brain or spinal fluid buildup.
- Liv Hospital provides patient-focused care and top results for shunt surgeries.
- Advances in medical imaging and navigation systems improve surgery accuracy and success.
- Conditions like hydrocephalus need quick and effective surgery to manage.
- Comprehensive care is available for international patients at Liv Hospital.
Understanding Cerebrospinal Fluid and Its Circulation
It’s key to understand cerebrospinal fluid and how it moves. This fluid is vital for our brain’s health.
What is Cerebrospinal Fluid?
Cerebrospinal fluid is a clear liquid in our brain and spine. It acts as a shock absorber for our brain. It also helps remove waste and brings nutrients to the brain.
Normal CSF Circulation Pathways
The fluid is made in the brain’s ventricles. It moves through the brain and spinal cord. Then, it goes back into the blood through special filters. This keeps the brain’s pressure just right.
When CSF Buildup Becomes Dangerous
Too much fluid can cause hydrocephalus. This is when fluid builds up in the brain. Symptoms include headaches and trouble thinking. If not treated, it can get very serious.
What’s a Shunt? Defining Medical Shunt Procedures

A shunt is a medical device that helps by moving fluid in the body. It’s used to manage conditions like too much cerebrospinal fluid (CSF).
Basic Definition and Purpose of Shunts
Medical shunts move fluid from one area to another. This helps relieve pressure and protects tissues. They’re mainly used for conditions like hydrocephalus.
Components of a Typical Shunt System
A shunt system has three parts: the catheter, valve, and reservoir. The catheter goes into the fluid buildup area. The valve controls how fast the fluid moves. The reservoir is for checking or to ease pressure.
| Component | Function |
|---|---|
| Catheter | Inserted into the area of fluid accumulation |
| Valve | Regulates fluid flow through the shunt |
| Reservoir | Accessed for diagnostics or pressure relief |
How Shunts Redirect Excess Fluid
Shunts create a new path for fluid to drain. For hydrocephalus, they move CSF from the brain to the belly. This helps keep brain pressure normal and prevents damage.
Hydrocephalus and Other Conditions Requiring Shunt in the Brain to Drain Fluid
Hydrocephalus often leads to the need for a brain shunt. It happens when too much cerebrospinal fluid (CSF) builds up in the brain. This causes the brain’s pressure to rise.
Congenital Hydrocephalus
Congenital hydrocephalus is present at birth. It can be caused by genetics, infections during pregnancy, or other developmental problems. Early diagnosis and surgery are often needed to manage it.
Acquired Hydrocephalus
Acquired hydrocephalus develops later in life. It can be caused by head trauma, infections like meningitis, or bleeding in the brain. Symptoms vary, so treatment plans must be tailored to each person.
Normal Pressure Hydrocephalus
Normal Pressure Hydrocephalus (NPH) mainly affects older adults. It’s marked by CSF buildup without high brain pressure. Symptoms include trouble walking, memory loss, and bladder control issues.
Other Neurological Conditions
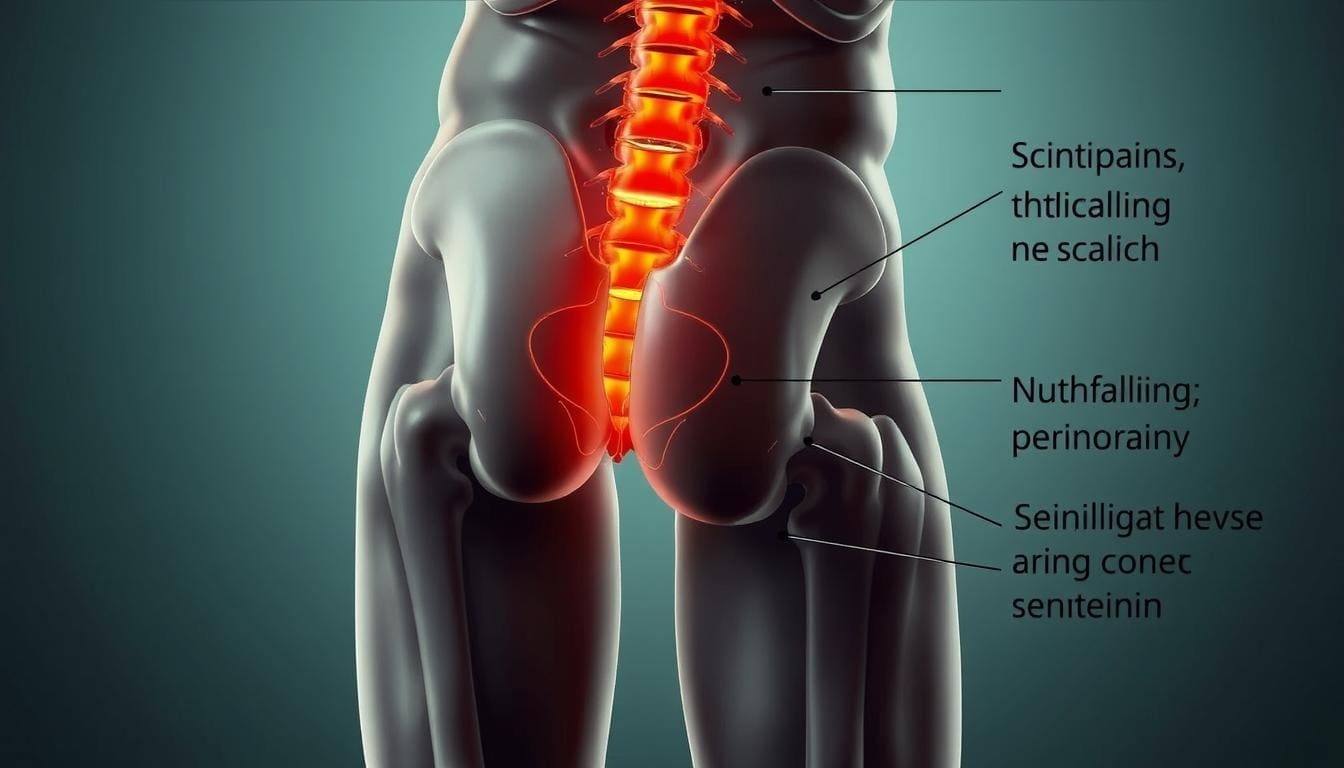
Other conditions needing a shunt include syringomyelia and arachnoid cysts. Syringomyelia forms a fluid-filled cavity in the spinal cord. Arachnoid cysts are fluid collections between the brain or spinal cord and the arachnoid membrane. Both can cause various neurological symptoms based on their size and location.
Spinal Shunt Procedures: Types and Applications
Spinal shunt procedures are key in neurosurgery. They help manage fluid buildup around the spinal cord. This helps patients with complex neurological issues find relief.
Syringomyelia and Spinal Cord Shunts
Syringomyelia causes a fluid-filled cavity in the spinal cord. This can damage the cord and worsen symptoms. Shunts help by moving excess fluid and easing pressure.
Shunts have greatly helped those with syringomyelia. They improve function and reduce symptoms. Early treatment is vital to avoid lasting damage.
Lumboperitoneal Shunting
Lumboperitoneal shunting moves cerebrospinal fluid from the lower back to the belly. It’s used for conditions like high pressure in the brain and some hydrocephalus.
This method is less invasive than traditional VP shunts. But, it needs to be placed correctly to work well.
Spinal Cord Cysts and Fluid Collections
Spinal cord cysts and fluid collections can come from trauma, tumors, or birth defects. Shunts help drain these, reducing pressure and improving function.
| Condition | Shunt Procedure | Primary Benefit |
|---|---|---|
| Syringomyelia | Spinal Cord Shunt | Relieves pressure on the spinal cord |
| Idiopathic Intracranial Hypertension | Lumboperitoneal Shunt | Reduces intracranial pressure |
| Spinal Cord Cysts | Spinal Cord Shunt | Drains fluid accumulation |
In conclusion, spinal shunt procedures are vital for treating many spinal conditions. Knowing the different types helps doctors provide better care for their patients.
Brain Shunt Procedures: Ventriculoperitoneal and Other Approaches
Brain shunts help move extra cerebrospinal fluid from the brain to other parts of the body. This is key for managing hydrocephalus, where fluid builds up in the brain.
Ventriculoperitoneal (VP) Shunts
Ventriculoperitoneal shunts are a common choice. They move fluid from the brain’s ventricles to the abdomen. The abdomen can handle a lot of fluid, making it a good spot for drainage. These shunts are often chosen because they have fewer complications and the body can easily absorb the fluid.
Ventriculoatrial (VA) Shunts
Ventriculoatrial shunts send fluid to the heart’s atrium. This is an option when the abdomen isn’t a good choice, like if there are infections or adhesions. VA shunts can be harder to keep working because of heart risks.
Ventriculopleural Shunts
Ventriculopleural shunts send fluid to the space around the lungs. This method is less common but can work for some patients. Yet, it might cause problems like fluid buildup in the lungs.
Choosing the Right Shunt Type
Choosing a shunt depends on many things. These include the patient’s health, the reason for hydrocephalus, and past surgeries. Our team looks at each case carefully to pick the best shunt for the best results.
In summary, brain shunt procedures are a critical treatment for hydrocephalus and other fluid disorders. Knowing about ventriculoperitoneal, ventriculoatrial, and ventriculopleural shunts helps patients make better choices for their care.
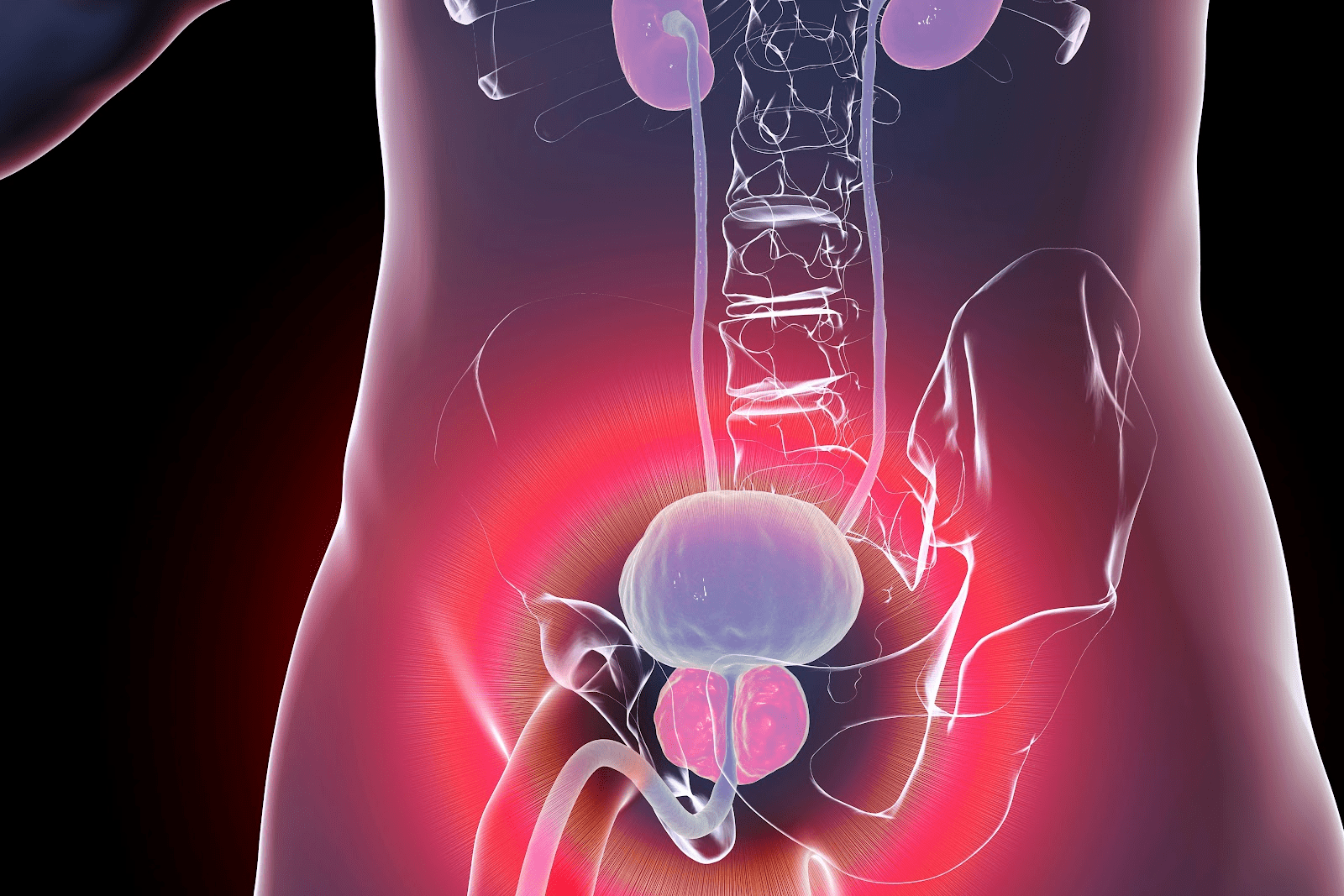
Shunt Brain to Stomach: The VP Shunt Process Explained
The VP shunt procedure is a common treatment for hydrocephalus. It involves moving cerebrospinal fluid from the brain to the stomach. This helps to reduce the pressure caused by too much fluid in the brain.
Surgical Placement of Catheters
The VP shunt process starts with surgical placement of catheters. Surgeons put a catheter in the brain’s ventricle to drain excess CSF. Another catheter goes into the stomach, where the fluid is absorbed.
The catheters are connected by a valve. This valve controls the flow of CSF, making sure it only goes from the brain to the stomach.
CSF Absorption in the Peritoneal Cavity
When CSF reaches the peritoneal cavity, it’s absorbed by the surrounding tissues. This process lowers the brain’s pressure from excess fluid. The peritoneal cavity’s large area makes it perfect for VP shunt placement.
Advantages of Abdominal Placement
The abdominal placement of the VP shunt has many advantages. It can handle more CSF, lowering the chance of shunt failure. Also, the stomach can grow with children, making VP shunts a good long-term option for kids.
The Surgical Shunt Procedure: From Preparation to Recovery
Understanding the surgical shunt procedure is key. It covers preparation to recovery stages. This guide helps patients and families know what to expect during treatment.
Preoperative Evaluation and Planning
Before surgery, patients get a detailed check-up. This includes imaging like MRI or CT scans to find the best shunt placement. We also look at their medical history and current health to spot risks.
Step-by-Step Surgical Process
The surgery has several steps. First, patients get general anesthesia for comfort. Then, a small scalp incision is made, and a hole is drilled in the skull. The shunt catheter is placed in the ventricle.
Immediate Postoperative Care
After surgery, patients are watched closely in the recovery room. We manage pain and check vital signs. We also look for any neurological issues or changes in mental status.
Hospital Stay and Initial Recovery
The hospital stay varies based on the patient’s condition and surgery complexity. We keep monitoring the patient, manage any issues, and teach about postoperative care and follow-ups.
Permanent Shunt Brain Technology and Modern Advancements
Medical technology has made big strides in making permanent shunt brain devices better. These improvements help treat hydrocephalus and other cerebrospinal fluid issues. They also make patients’ lives better and more comfortable.
Biocompatible Materials in Modern Shunts
Today’s shunts are made from biocompatible materials. These materials lower the chance of bad reactions and make the devices last longer. Silicone and polyurethane are often used because they’re strong and safe for the body.
Programmable Valve Systems
Programmable valve systems let doctors control how cerebrospinal fluid is drained. This means they can tailor treatment to each patient. It’s helped manage hydrocephalus better and cut down on the need for more surgeries.
Anti-Siphon and Gravity-Compensating Devices
Anti-siphon and gravity-compensating devices stop too much cerebrospinal fluid from draining. This is a big problem with shunts. These devices help keep the fluid balance right, which lowers the risk of complications.
Future Innovations in Shunt Technology
The future of shunt technology looks bright. Scientists are working on smart shunts that can watch intracranial pressure and adjust drainage as needed. A recent report says the market for cerebrospinal fluid management will grow a lot. This is because of new medical devices and more people getting neurological disorders (source).
| Feature | Traditional Shunts | Modern Shunts |
|---|---|---|
| Material | Basic plastics | Biocompatible materials (silicone, polyurethane) |
| Valve System | Fixed pressure | Programmable valve systems |
| Complications | Higher risk of overdrainage | Reduced risk with anti-siphon devices |
AV Shunt in Brain: Vascular Shunts vs. CSF Shunts
When we talk about shunts in the brain, it’s key to know the difference between vascular and CSF shunts. This is important for finding the right treatment for brain problems.
Understanding Arteriovenous Malformations
Arteriovenous malformations (AVMs) are weird connections between arteries and veins in the brain. They can cause big health problems, like bleeding and brain damage. AV shunts are used to treat AVMs by changing how blood flows and helping symptoms.
How Vascular Shunts Differ from CSF Shunts
Vascular shunts, like those for AVMs, deal with blood flow issues. CSF shunts, on the other hand, help with too much fluid in the brain. Each type of shunt is made for a specific problem, showing why picking the right one is so important.
| Characteristics | Vascular Shunts | CSF Shunts |
|---|---|---|
| Purpose | Manage abnormal blood flow | Drain excess CSF |
| Common Conditions Treated | Arteriovenous Malformations | Hydrocephalus |
Treatment Approaches for Vascular Issues
Fixing vascular problems like AVMs needs a team effort. This includes surgery, blocking blood flow, and radiation. The best treatment depends on the malformation’s size, where it is, and the patient’s health.
Revision Shunt Surgery: Complications and Solutions
Shunt procedures can lead to complications like malfunction or infection. Revision surgery is needed to fix these issues. It aims to ensure proper cerebrospinal fluid (CSF) drainage.
Common Causes of Shunt Malfunction
Shunt malfunction can happen for several reasons. These include mechanical failures, infections, or blockages in the shunt system. Knowing these causes helps in managing and preventing future problems.
Infection Risks and Management
Infections are a big risk with shunt revision surgery. We take strict infection control measures. This includes using antibiotics and careful surgical techniques.
Obstruction and Mechanical Failures
Blockages in the shunt system can cause malfunction. This often needs quick revision surgery. Mechanical failures, like broken catheters or faulty valves, also require revision to fix CSF drainage.
Success Rates of Revision Procedures
The success of revision shunt surgery depends on the cause of the problem and the patient’s health. Usually, these procedures have a high success rate. They help solve the immediate issue and improve patient outcomes.
Understanding the complications of shunt procedures and the solutions of revision surgery helps patients make better choices. Our team is dedicated to providing top care for those undergoing revision shunt surgery.
Cranial Shunt vs. Traditional Head Shunt: Surgical Approaches
It’s important to know the differences between cranial shunt and traditional head shunt surgeries. We’ll look at the various surgical methods. This includes endoscopic techniques and traditional open surgery. We’ll discuss their outcomes and how long it takes to recover.
Endoscopic Minimally Invasive Techniques
Endoscopic surgery has changed neurosurgery a lot. It’s a less invasive way to place shunts. A small camera and tools are used through tiny cuts. This method causes less damage and helps patients recover faster.
Traditional Open Surgical Methods
Traditional open surgery uses a bigger cut to reach the brain or spine. It’s more invasive but gives surgeons a better view. They can access the area more directly.
Comparing Outcomes and Recovery Times
Research shows endoscopic surgery leads to shorter hospital stays and quicker recovery. But, the choice depends on the patient’s condition and the surgeon’s opinion.
| Surgical Approach | Recovery Time | Hospital Stay |
|---|---|---|
| Endoscopic | 1-2 weeks | 2-3 days |
| Traditional Open Surgery | 4-6 weeks | 5-7 days |
Latest Advancements in Surgical Techniques
New advancements in neurosurgery aim to make shunt procedures more precise and safe. The development of new materials and techniques is improving patient results.
Conclusion
Shunt procedures are key for managing cerebrospinal fluid (CSF) issues. This is true for patients with hydrocephalus and other neurological problems. Both spinal and brain shunts help by moving excess CSF away from the brain and spinal cord.
We’ve talked about different shunt types, like ventriculoperitoneal (VP) shunts. These shunts move CSF from the brain to the belly. New technologies, like programmable valves and biocompatible materials, have made these treatments better.
For patients from other countries looking for top medical care, knowing about shunt procedures is important. Understanding these basics helps patients make better choices about their health. It also helps them deal with the complex world of neurosurgery.
As medical tech keeps getting better, we’ll see even more improvements in shunt procedures. This will lead to better lives for patients. Our goal is to offer the best healthcare to international patients. We want to make sure they get the care they need for their brain and spinal health.
FAQ
What is a shunt procedure, and how does it work?
A shunt procedure is a surgery that implants a device. This device redirects excess cerebrospinal fluid (CSF) from the brain or spinal cord. It sends the fluid to another part of the body where it can be absorbed.
References
- PMC – PubMed Central : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6153620