Thrombosis is when a blood clot forms inside a blood vessel. It can block blood flow and cause serious problems. Knowing about the different types of thrombosis is key to treating it early.
At Liv Hospital, we focus on top-notch patient care. We follow global standards to handle blood clot diseases. We aim to help you understand the 5 types of thrombosis, their signs, and why getting medical help is important.
Thrombosis can have severe consequences if not properly managed. We will look at the main types of thrombosis. This will help you spot the risks and know how to treat them.
Key Takeaways
- Thrombosis is a serious condition that obstructs blood flow.
- Understanding the different types of thrombosis is key to treatment.
- Liv Hospital offers advanced care for complex blood clot diseases.
- Spotting thrombosis symptoms early is vital.
- Getting medical help is essential for managing thrombosis.
Understanding Thrombosis: The Basics of Blood Clots
It’s key to know about thrombosis to avoid its dangers. This condition can take many forms and happen in different parts of the body. It’s hard to spot and treat.
What Is Thrombosis and How Does It Develop?
Thrombosis is when a blood clot forms in a blood vessel. This clot can block blood flow, causing health problems. Venous thrombosis happens in veins, and arterial thrombosis affects arteries.
Thrombosis starts with changes in blood flow, injuries to blood vessel walls, and blisters. Virchow’s triad explains these three main factors.
- Blood flow changes: Stasis or turbulence can lead to clotting.
- Vessel wall injuries: Damage to the endothelium can start thrombosis.
- Alterations in blood constitution: Hypercoagulability increases clotting tendency.
The Importance of Early Detection
Finding thrombosis early is vital for managing it well. Knowing the risk factors and symptoms helps get timely medical help. For example, deep vein thrombosis (DVT) might show as swelling, pain, or color changes in the leg.
Studies show that quick diagnosis and treatment can lower severe outcome risks, like pulmonary embolism. We should watch for warning signs and get medical help if they don’t go away or get worse.
“Early recognition and treatment of thrombosis can be lifesaving. Both healthcare providers and patients need to be vigilant about the signs and symptoms.”
Knowing how thrombosis works helps us see why finding it early is so important. We can then take steps to prevent it.
The 5 Types of Thrombosis Explained

It’s important to know about the different types of thrombosis. This is because thrombosis, or blood clots, can happen in many ways. Each type has its own causes and effects.
Classification of Blood Clots by Location and Severity
Thrombosis is classified by where and how severe the clot is. There are five main types: arterial thrombosis, venous thrombosis (like Deep Vein Thrombosis or DVT), pulmonary embolism, microthrombosis, and superficial vein thrombosis. Each type has its own signs and symptoms.
- Arterial Thrombosis: Happens in arteries and can cause heart attacks and strokes.
- Venous Thrombosis: Forms in veins, with DVT being a common type in the legs.
- Pulmonary Embolism: A clot in the lungs can be very dangerous.
- Microthrombosis: Small clots in tiny blood vessels can harm organs.
- Superficial Vein Thrombosis: Clots in veins close to the skin’s surface.
Prevalence and General Risk Factors
Some types of thrombosis are more common than others. For example, venous thrombosis is more common than arterial thrombosis in some groups. Risk factors include genetic predispositions, immobility, cancer, and surgical procedures. Knowing these can help prevent and catch thrombosis early.
Understanding the different types of thrombosis and their risks can help patients. Healthcare providers can then tailor treatments to each patient’s needs.
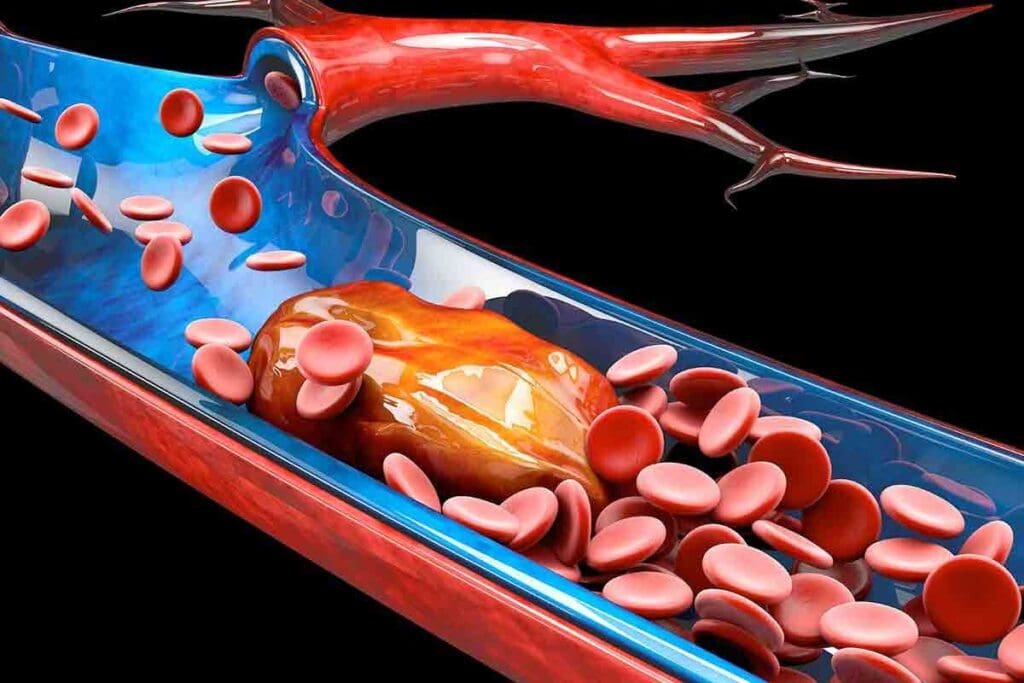
Arterial Thrombosis: Blood Clots in the Arteries
Arterial thrombosis happens when a blood clot blocks an artery. This stops blood from reaching important organs. It often starts with an atheroma rupture, leading to atherothrombosis. These clots can cause serious problems, like tissue damage and death.
Characteristics and Formation Mechanisms
Arterial thrombosis is different because it happens in arteries. Blood flows fast here, and oxygen levels are high. It usually starts with a plaque rupture, exposing material that makes blood clot.
These clots have lots of platelets and look white. Knowing how they form helps us find ways to stop them.
Femoral Artery Blood Clots and Other Common Locations
Arterial thrombosis can happen in many arteries. Common spots include:
- The femoral artery in the legs
- Coronary arteries, which can cause heart attacks
- Cerebral arteries, leading to strokes
- Renal arteries, affecting the kidneys
Femoral artery clots can cause severe leg problems. They need quick medical help to avoid losing a limb.
Health Consequences and Complications
The effects of arterial thrombosis can be very serious. When an artery is blocked, the area it supplies can become damaged. The damage depends on where the clot is:
| Location | Potential Consequence |
| Coronary Artery | Myocardial Infarction (Heart Attack) |
| Cerebral Artery | Ischemic Stroke |
| Femoral Artery | Acute Limb Ischemia |
Quick medical help is vital to avoid serious damage. Knowing the risks and signs of arterial thrombosis is important to prevent harm.
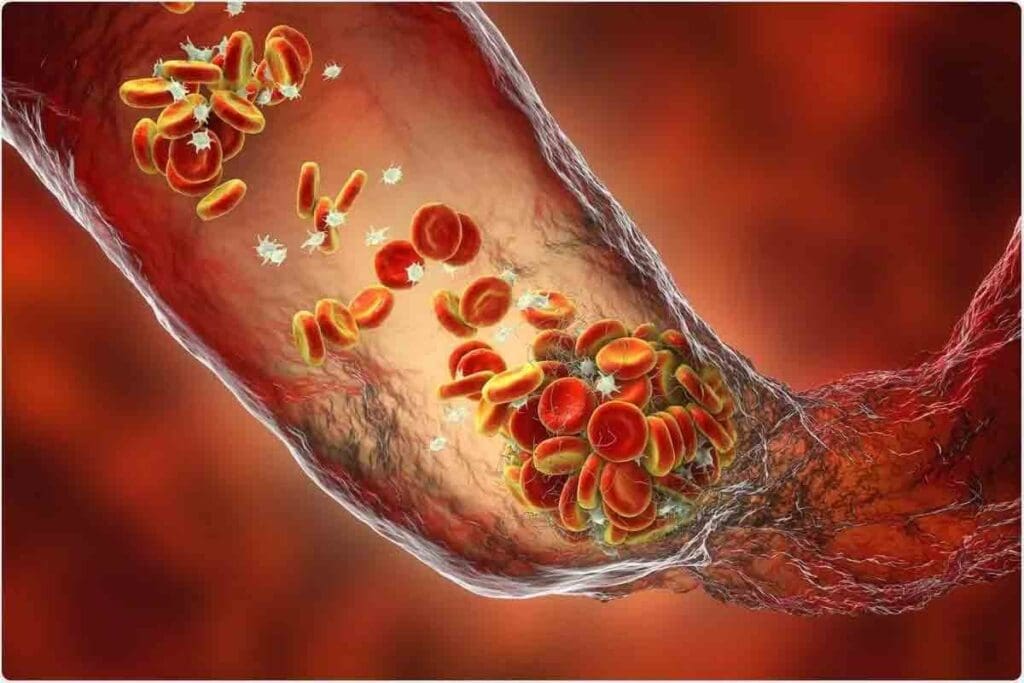
Venous Thrombosis: Deep Vein Thrombosis (DVT)
It’s important to know about venous thrombosis, like DVT. This is when a blood clot forms in a vein. DVT happens in the deep veins, often in the legs.
Formation of DVT in Deep Veins
DVT forms in deep veins due to several reasons. These include slow blood flow, injury to the vein, and changes in blood clotting. A blood clot can block blood flow, causing serious problems.
Types of Thrombosis in Legs, Arms, and Pelvis
DVT can happen in the legs, arms, and pelvis. The femoral vein in the leg is a common spot for DVT. In arms, it can be in the subclavian or axillary veins. Pelvic DVT affects the iliac veins.
Risk Factors for DVT include:
- Prolonged immobility or bed rest
- Major surgery or trauma
- Cancer and its treatment
- Family history of DVT
- Obesity
Risk Factors and Warning Signs
Knowing the risk factors and warning signs of DVT is key. Look out for swelling, pain, or tenderness in the limb. Also, watch for warmth or redness of the skin.
If you notice these symptoms, seek medical help. This is very important, as early treatment can prevent serious issues like pulmonary embolism.
Pulmonary Embolism: When Clots Travel to the Lungs
When a deep vein thrombosis breaks loose, it can cause a pulmonary embolism, a potentially life-threatening condition. This happens when a clot from the deep veins of the legs travels to the lungs. It blocks blood flow to the lungs.
The Connection Between DVT and Pulmonary Embolism
The Link Between DVT and Pulmonary Embolism
Deep vein thrombosis (DVT) and pulmonary embolism (PE) are closely related. DVT is when a blood clot forms in the deep veins, usually in the legs. If a part of this clot breaks loose, it can travel to the lungs, causing a pulmonary embolism.
This shows why it’s important to quickly diagnose and treat DVT. This can prevent the serious complication of PE.
Studies show that about 50% of patients with DVT also have asymptomatic PE. This highlights the strong link between these two conditions. The risk of PE is higher in patients with DVT closer to the body’s center. This means early detection and management are key.
Recognizing Symptoms and Emergency Warning Signs
Pulmonary embolism can have mild to severe symptoms. Common signs include:
- Dyspnea (shortness of breath)
- Chest pain that worsens with deep breathing
- Coughing up blood
- Rapid heart rate
- Lightheadedness or fainting
Some patients may not show symptoms until the condition is severe. Severe dyspnea, chest pain, or syncope (fainting) need immediate medical attention.
“Prompt recognition and treatment of pulmonary embolism are critical to saving lives. Delaying medical care can significantly increase the risk of mortality.”
Mortality Rates and Survival Factors
The mortality rate for pulmonary embolism varies. It depends on the clot’s size and location, the patient’s health, and the treatment’s effectiveness. Studies show the mortality rate can be between 1% and 30% within the first three months after diagnosis.
Early diagnosis and proper treatment can greatly improve survival chances. Anticoagulation therapy is the main treatment. Thrombolytic therapy is used in severe cases. The choice of treatment depends on the PE’s severity, the patient’s risk factors, and any therapy contraindications.
Understanding DVT and PE risk factors, recognizing symptoms, and seeking quick medical care are key steps in managing these conditions effectively.
Microthrombosis: Small Thrombosis with Serious Consequences
Microthrombosis is when tiny blood clots form in small blood vessels. This can cause serious health problems. It’s a big issue in critical illnesses, leading to organ failure.
Formation in Small Blood Vessels
Microthrombosis happens when small clots form in tiny blood vessels. These vessels are key to delivering oxygen and nutrients. Factors like inflammation, infection, and trauma can trigger this.
Key factors contributing to microthrombosis include:
- Activation of the coagulation cascade
- Endothelial dysfunction
- Platelet activation
Role in Sepsis and Organ Damage
Microthrombosis is key in sepsis, a deadly condition. It happens when the body’s fight against infection harms its own tissues and organs. In sepsis, microthrombi can block organs, causing them to fail.
The consequences of microthrombosis in sepsis can be severe, including:
- Acute kidney injury
- Respiratory failure
- Cardiac dysfunction
Recent Research Findings
Recent studies show the importance of many diseases. It’s not just a sepsis complication but also a target for treatment. Researchers are looking into ways to stop and treat it, like anticoagulants and improving blood vessel function.
As we learn more about microthrombosis, its role in organ failure is clear. More research is needed to understand it better and find effective treatments.
Superficial Vein Thrombosis: Clots Near the Skin
Superficial vein thrombosis is a blood clot in a vein close to the skin. It’s not as dangerous as deep vein thrombosis, but it needs medical care. We’ll look at what superficial vein thrombosis is, where it happens, and its link to serious conditions.
Distinguishing Features and Locations
Superficial vein thrombosis happens in veins near the skin’s surface. These veins can swell and become inflamed when a clot forms. Symptoms include pain, redness, and swelling in the affected area.
Superficial vein thrombosis occurs in the veins close to the skin. This makes it less likely to cause a pulmonary embolism than deep vein thrombosis. Yet, it’s important to get medical help because it might be linked to deep vein thrombosis.
Partial Thrombus: Incomplete Vessel Blockage
A partial thrombus is a blood clot that doesn’t block the vein completely. In superficial vein thrombosis, it can cause pain and swelling. This shows the clotting process is ongoing, with risks of the clot growing or breaking off.
Research in medical journals says managing partial thrombus means watching the clot’s size. It’s also about checking if it might become a bigger blockage or cause other problems.
Connection to Deeper Thrombosis Types
Superficial vein thrombosis is generally safer than deep vein thrombosis. But there’s a link between the two. Studies show people with superficial vein thrombosis might be at higher risk for deep vein thrombosis or other blood clots. So, it’s key for those with superficial vein thrombosis to get checked for other risks and get the right treatment to avoid complications.
If you have symptoms like pain or swelling in a superficial vein, see a doctor. Early treatment can help manage the condition and lower the risk of serious problems.
Uncommon but Dangerous: Blood Clots in the Neck and Shoulder
Thrombosis in the neck and shoulder is rare but very dangerous. Most people know about leg blood clots. But clots in the neck and shoulder are just as risky and need quick medical help.
Neck Blood Clots and Jugular Vein Thrombosis
Neck blood clots, like those in the jugular vein, are serious. They can cause pulmonary embolism and stroke. The jugular vein carries blood from the head to the heart.
When a clot blocks this vein, it can cause swelling, pain, and serious problems. We’ll look at what causes these clots and how to treat them. Knowing about risks like central venous catheters, cancer, and genetic disorders is key.
Clots in the Shoulder and Upper Extremity
Clots in the shoulder and upper arm are less common but serious. These clots can happen in the deep veins of the arm, known as upper extremity deep vein thrombosis (UEDVT). UEDVT can be caused by hard exercise, injury, or a central venous catheter.
Symptoms include swelling, pain, and arm discoloration. Untreated, these clots can cause serious problems like pulmonary embolism or post-thrombotic syndrome. We’ll talk about how to diagnose and treat these clots, stressing the need for fast medical care.
Knowing the risks and symptoms of neck and shoulder blood clots helps. It lets people get medical help quickly, avoiding serious issues.
Diagnosis and Detection of Different Thrombosis Types
Diagnosing thrombosis requires imaging and blood tests. Accurate diagnosis is key to effective treatment and preventing complications.
Imaging Techniques and Blood Tests
Several imaging methods are used to find thrombosis, based on its location and type. These include:
- Ultrasound: Great for spotting Deep Vein Thrombosis (DVT) and superficial vein thrombosis.
- Computed Tomography (CT) scans: Often used for diagnosing pulmonary embolism and other thrombosis types.
- Magnetic Resonance Imaging (MRI): Useful for detecting thrombosis in the brain and pelvis, among other areas.
Blood tests are also vital in diagnosing thrombosis. The D-dimer test is the most common. It checks D-dimer levels, a protein fragment from dissolving blood clots.
When to Seek Emergency Medical Care
Knowing when to get emergency care is important. Look out for these symptoms:
- Severe chest pain or trouble breathing, which might mean a pulmonary embolism.
- Severe pain or swelling in one leg, a sign of DVT.
- Sudden confusion, trouble speaking, or weakness, which could be a stroke caused by thrombosis.
Quick medical help can greatly improve outcomes for thrombosis. If you’re experiencing symptoms or have concerns, talk to your healthcare provider.
Treatment and Prevention Strategies for Thrombosis
Managing thrombosis well needs a mix of medical care, surgery, and lifestyle changes. We’ll look at how to treat and prevent thrombosis. We’ll focus on the best methods available today.
Medical Treatments for Different Types of Thromboembolism
For treating thrombosis, doctors often use anticoagulation therapy. This stops clots from getting bigger and new ones from forming. Anticoagulant medications are chosen based on the patient’s health and the clot’s location and size. For deep vein thrombosis (DVT), anticoagulation is key to avoiding pulmonary embolism.
Anticoagulation therapy has two parts. The first part aims to stop clot growth and prevent immediate problems. The second part is for long-term prevention of clots coming back.
Thrombolysis is another treatment. It uses drugs to dissolve clots. This is usually for severe cases like massive pulmonary embolism or DVT that could harm limbs.
Surgical Interventions
Surgery might be needed for some thrombosis cases. Options include removing the clot (thrombectomy) and putting in vena cava filters to stop pulmonary embolism in those who can’t take anticoagulants.
Surgery is considered when anticoagulation risks are high or other treatments fail. The decision to have surgery depends on the patient’s health and situation.
Lifestyle Changes to Prevent Blood Clots
To prevent thrombosis, big lifestyle changes are needed. Stay hydrated, avoid sitting for too long, and exercise regularly. People at high risk, like those with a DVT or pulmonary embolism history, might need more steps.
Keeping a healthy weight, managing conditions like high blood pressure and diabetes, and not smoking are also key. Some might need anticoagulants during high-risk times, like surgery or long trips.
| Lifestyle Change | Benefit |
| Staying Hydrated | Reduces blood viscosity, lowering clot risk |
| Regular Physical Activity | Improves circulation, reduces immobility-related risks |
| Avoiding Prolonged Immobility | Reduces the risk of clot formation |
“Prevention is key in managing thrombosis. By understanding the risk factors and making appropriate lifestyle changes, individuals can significantly reduce their likelihood of developing blood clots.”
In conclusion, treating and preventing thrombosis needs a mix of medical care, surgery, and lifestyle changes. Knowing the strategies and working with healthcare providers can help manage risk and prevent complications.
Conclusion: Understanding Your Risk and Taking Action
Knowing your risk for thrombosis is key to avoiding this serious condition. We’ve looked at the different types of thrombosis, their signs, and the dangers they pose.
By learning about risk factors and warning signs, you can lower your chance of getting thrombosis. Simple steps like keeping a healthy weight, drinking plenty of water, and exercising regularly can help.
To prevent thrombosis, you need to know your risk, watch for symptoms, and get medical help when needed. By being proactive and informed, we can cut down on thrombosis cases and their serious effects.
By understanding and managing your risk for thrombosis, you can keep yourself healthy. Being aware and careful is essential to avoid the serious problems that thrombosis can cause.
FAQ
What are the main types of thrombosis?
The main types are arterial thrombosis, venous thrombosis (like deep vein thrombosis), pulmonary embolism, microthrombosis, and superficial vein thrombosis.
What is the difference between venous and arterial thrombosis?
Venous thrombosis happens in veins and forms clots in deep veins. Arterial thrombosis forms in arteries and can cause tissue damage by reducing blood flow.
Can you get a blood clot in your neck?
Yes, blood clots can form in the neck. This is known as jugular vein thrombosis and is a serious condition needing quick medical help.
What are the symptoms of a femoral artery blood clot?
Symptoms include pain, swelling, and decreased pulses in the leg. If not treated, it can cause severe ischemia.
How is deep vein thrombosis (DVT) diagnosed?
Doctors use ultrasound and clinical assessment to diagnose DVT. Blood tests like D-dimer may also be used.
What is the connection between DVT and pulmonary embolism?
DVT can cause pulmonary embolism if a clot breaks loose and goes to the lungs. This is a life-threatening condition needing immediate care.
What are the risk factors for developing thrombosis?
Risk factors include immobility, surgery, cancer, genetic predispositions, and certain medical conditions.
How can thrombosis be prevented?
Prevention includes regular exercise, a healthy weight, avoiding immobility, and sometimes anticoagulant medications.
What is microthrombosis and its significance?
Microthrombosis is the formation of small clots in small blood vessels. It’s critical in conditions like sepsis and organ damage.
Can superficial vein thrombosis lead to more serious conditions?
Superficial vein thrombosis is usually less severe. But it can increase the risk of deep vein thrombosis or other thrombotic events.
When should someone seek emergency medical care for thrombosis?
Seek emergency care for severe symptoms like sudden breathing trouble, severe chest pain, or severe limb pain and swelling.
Is femoral vein thrombosis dangerous?
Yes, femoral vein thrombosis is dangerous. It can lead to pulmonary embolism or post-thrombotic syndrome.
What are the treatment options for thrombosis?
Treatments include anticoagulant medications, thrombolytic therapy, and sometimes surgery to remove or bypass the clot.
References
- Ayyoub, S., et al. (2023). Thrombosis models: An overview of common in vivo and in vitro models of venous and arterial thrombosis. Frontiers in Cardiovascular Medicine, 10, Article 1060553. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9917341/




































