Last Updated on November 27, 2025 by Bilal Hasdemir

Arteriovenous malformations (AVMs) are abnormal connections between arteries and veins. They can happen in the brain, skin, and legs. These blood vessel tangles can cause big health problems. At Liv Hospital, we know how serious AVMs are and how important it is to care for our patients well.
It’s key for patients and families to understand the risks, spot the signs, and know the latest treatment options. The National Institute of Neurological Disorders says AVMs can lead to seizures, headaches, and vision problems. We aim to give top-notch healthcare and support to patients from around the world.
Key Takeaways
- Arteriovenous malformations can occur in various parts of the body, including the brain, skin, and legs.
- Rupture of an AVM can lead to serious health complications.
- Symptoms of AVMs can include seizures, headaches, and visual problems.
- Treatment options for AVMs include conventional surgery, endovascular embolization, and radiosurgery.
- Understanding the risks and recognizing the signs of AVMs is critical for timely medical care.
What Are Arteriovenous Malformations?

An arteriovenous malformation, or AVM, is an abnormal connection between arteries and veins. This condition disrupts the normal flow of blood. It can lead to various health complications.
Definition and Abnormal Blood Vessel Structure
An AVM is a tangled network of blood vessels. They directly connect arteries to veins, skipping the capillary system. This can cause tissue damage and organ dysfunction. The arteriovenous malformation definition covers a wide range of vascular anomalies, each with its own risks.
How AVMs Disrupt Normal Blood Flow
AVMs create a high-flow, low-resistance pathway between arteries and veins. This can lower blood pressure and oxygen delivery to tissues. People with AVMs may feel pain, swelling, and tissue damage. Knowing how AVMs affect blood flow is key to finding effective treatments.
What Does AVM Stand for in Medical Terms?
In medical terms, AVM stands for Arteriovenous Malformation. It refers to the abnormal connection between arteries and veins. The acronym AVM is used in medical literature and patient communications to describe this vascular anomaly.
| Term | Definition |
|---|---|
| Arteriovenous Malformation (AVM) | An abnormal connection between arteries and veins. |
| AVM | Acronym for Arteriovenous Malformation. |
| Vascular Anomaly | A birthmark or abnormal formation of blood vessels. |
Understanding AVMs and their effects on the body is vital. It helps us see why proper diagnosis and treatment are so important. Our medical team is dedicated to providing the best care for those with AVMs.
Common Locations Where AVMs Develop

Arteriovenous malformations (AVMs) can happen in many parts of the body. Each location has its own special features and possible problems. We’ll look at where AVMs can appear, what makes them different, and what they might mean for health.
Brain AVMs
Brain AVMs are well-studied because they can cause serious brain problems. They can mess up blood flow, leading to a high risk of bleeding. People often find out they have a brain AVM when they have seizures or headaches.
Skin AVMs
Skin AVMs show up as spots or swellings on the skin. They might be there from birth or show up later. These spots can be a concern for how they look and might cause problems like bleeding or ulcers.
Leg and Arm AVMs
AVMs can also happen in the arms and legs. They can cause pain, swelling, and make it hard to move. AVMs in the limbs need special care to help manage symptoms and avoid more serious issues.
Heart AVMs and Other Rare Locations
AVMs can also be found in the heart and other rare places. These cases are tricky to diagnose and treat because of where they are. Heart AVMs, for example, can affect how well the heart works and need careful handling to avoid serious problems.
Understanding AVM Rupture and Its Consequences
AVM rupture happens when the abnormal blood vessels in the malformation tear or burst. This can cause serious health problems. It’s important for patients and doctors to know the risks and what can happen.
The Mechanism of Rupture
The exact reason for AVM rupture is complex. High-pressure blood flow through these vessels can weaken the walls. Hypertension and vascular stress also play a role in the risk of rupture.
- Increased pressure within the AVM
- Weakening of the blood vessel walls
- Presence of other vascular abnormalities
Hemorrhage and Stroke Risk
When an AVM ruptures, it can cause hemorrhage or bleeding in the brain. This can lead to a stroke, causing serious brain damage. The risk of stroke after an AVM rupture is very high and needs quick medical help.
Neurological Deficits Following Rupture
The effects of an AVM rupture can vary. They may include weakness, numbness, vision changes, and cognitive impairments. Quick medical care is key to reduce long-term harm.
- Immediate medical evaluation
- Diagnostic imaging to assess the rupture
- Treatment to prevent further bleeding and repair damage
Knowing the risks and effects of AVM rupture is key to managing it well. We will look at the statistical risks and how AVMs present clinically next.
Statistical Risks of AVM Rupture
Knowing the risks of AVM rupture helps us make better treatment choices. Arteriovenous malformations (AVMs) are unusual connections between arteries and veins. They can burst, causing serious health problems. It’s important for both patients and doctors to understand these risks.
2-4% Annual Risk for Unruptured AVMs
The chance of an unruptured AVM bursting each year is between 2% and 4%. This shows that the risk can vary based on the patient and the AVM itself. We see this risk as high and important for planning treatment.
6% Re-rupture Risk in the First Year
For those who have had an AVM burst, the risk of it happening again is high, up to 6% in the first year. This risk is why we watch these patients closely and might suggest more aggressive treatments.
Factors That Increase Rupture Probability
Several things can make an AVM more likely to burst. These include the AVM’s size and where it is, as well as the patient’s age and health. We also look at other vascular issues as risk factors. Knowing these helps us tailor treatments to each patient’s needs.
By understanding these risks, we can manage AVMs better and lower the chance of them bursting. Our goal is to give each patient care that fits their unique situation and risks.
Skin AVM: Symptoms and Identification
Spotting the signs of skin AVMs is key to getting the right treatment. These malformations can show up in many ways, making it important for doctors to know what to look for.
Visual Characteristics of Arteriovenous Malformation Skin Lesions
Skin AVMs often look like discolored lesions on the skin. They can be red, purple, or blue because of the blood vessels underneath. These spots can be flat or raised and feel warm or pulsatile to the touch.
Discoloration and Swelling Patterns
The color of skin AVMs can change, showing up as a patch or a mass. Sometimes, the skin over the AVM gets thinned or ulcerated. The way the color and swelling look can hint at what’s going on under the surface.
When to Seek Medical Attention
If you see any odd skin spots or changes, get medical help. Look out for these signs:
- Rapid growth or change in the lesion
- Pain or tenderness associated with the lesion
- Ulceration or bleeding from the lesion
- Significant cosmetic concern
Seeing a doctor early can make a big difference in treating skin AVMs. If you’re worried about a skin spot, talk to a healthcare professional.
| Symptom | Description | Action |
|---|---|---|
| Discoloration | Red, purple, or blue lesions | Monitor and consult a doctor |
| Swelling | Swollen area around the lesion | Seek medical evaluation |
| Pain/Tenderness | Pain associated with the lesion | Consult a healthcare provider |
Leg and Arm AVMs: Clinical Presentation
AVMs in the legs and arms can cause pain, swelling, and serious problems. These symptoms come from the abnormal blood vessel structure of AVMs. It disrupts normal blood flow, leading to noticeable symptoms.
Pain and Swelling in Extremities
Pain and swelling are common in leg and arm AVMs. The abnormal blood flow and increased pressure cause discomfort and swelling. Patients may feel a range of pain, from mild to severe, which gets worse with activity.
Ulceration and Tissue Damage
In severe cases, AVMs can cause ulcers and tissue damage. The poor blood flow leads to skin ulcers, which are painful and hard to heal. Prompt medical attention is key to prevent more damage and complications.
Impact on Mobility and Quality of Life
AVMs in the legs and arms can greatly affect mobility and quality of life. The pain, swelling, and tissue damage limit physical activity and daily tasks.
“Effective management of extremity AVMs requires a complete approach to reduce symptoms and improve outcomes.”
Living with an AVM in the leg or arm is tough. Our team is committed to personalized care for each patient. We aim to enhance their quality of life with advanced treatments.
Advanced Diagnostic Imaging for AVMs
Advanced imaging is key in finding and checking AVMs. It helps doctors plan the best treatments. AVMs are complex, so we need top-notch imaging to see them clearly.
MRI Capabilities for AVM Detection
Magnetic Resonance Imaging (MRI) is a top tool for spotting AVMs. It shows detailed pictures of the malformation and nearby tissues. MRI helps figure out the AVM’s size, where it is, and how it flows, which is vital for treatment.
A leading medical expert says, “MRI has changed how we diagnose AVMs, giving us unmatched detail and clarity.”
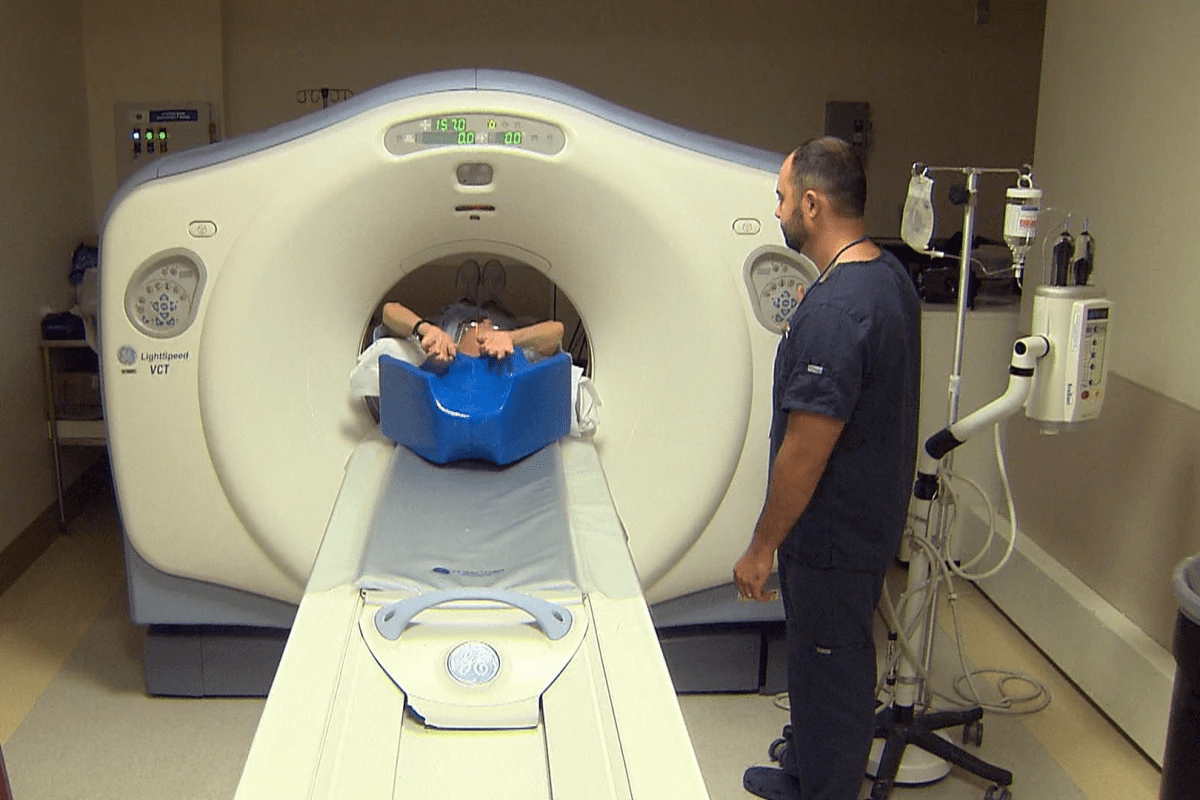
CT Angiography Techniques
CT angiography is also a key tool in AVM diagnosis. It uses CT scans with contrast to see blood vessels and find AVMs. It’s great for spotting AVMs in the brain and other tricky spots.
CT angiography gives detailed pictures of the AVM’s structure. This is key for picking the right treatment.
Cerebral Angiography for Detailed Mapping
Cerebral angiography is the top choice for brain AVMs. It involves injecting contrast into blood vessels to see the AVM’s layout and its connections. It gives the needed info for planning surgeries or endovascular treatments.
Cerebral angiography is essential for detailed AVM checks, guiding treatment choices and better patient results
Thanks to these advanced imaging methods, doctors can better diagnose and manage AVMs. This leads to better care and outcomes for patients.
Microsurgical Resection: Removing the AVM
Microsurgical resection is a top choice for treating AVMs. It involves removing the AVM with great care. This method offers a lasting fix for many patients.
Surgical Approach and Techniques
This surgery is done under general anesthesia. Neurosurgeons use advanced tools and imaging to find and remove the AVM. The precision of microsurgical techniques helps keep nearby brain areas safe.
The surgery plan is made just for each patient. It considers the AVM’s size, location, and depth. For AVMs in key brain spots, the surgery must be very careful to protect important brain tissue.
Ideal Candidates for Surgical Intervention
Not every AVM patient is right for surgery. The choice to have surgery depends on the AVM’s size, location, and the patient’s health. Patients with small to medium-sized AVMs that are easy to reach and not in critical spots are usually the best candidates.
- AVMs with previous hemorrhage
- Young patients with a long life expectancy
- AVMs causing significant symptoms
Recovery Timeline and Expectations
Recovery times after surgery vary. It depends on how complex the surgery was and the patient’s health. Most patients stay in the ICU for at least 24 hours after surgery. Recovery can take weeks to months, with full recovery expected within 6-12 months for many.
After surgery, patients see their neurosurgeon regularly. This is to check on healing and handle any issues. They also learn about rehabilitation to help regain lost functions.
Knowing about microsurgical resection helps patients and their families make better choices. This leads to better results in treating AVMs.
Embolization of AVMs: Minimally Invasive Treatment
Embolization is a key treatment for arteriovenous malformations (AVMs). It’s a less invasive option compared to traditional surgery. This method blocks blood flow to the AVM using special materials. It can be used alone or before surgery.
How AVM Embolization Works
To start, a small incision is made in the groin. A catheter is then inserted and guided to the AVM. Embolic materials like coils or glue are used to block the abnormal vessels.
This reduces the risk of rupture and relieves symptoms. It’s a vital step in treating AVMs.
Types of Embolic Materials Used
Different materials are used in AVM embolization, each with its own benefits. These include:
- Coils: Mechanical coils that cause blood clots in the AVM.
- Liquid Embolic Agents: Glue-like substances that harden in blood.
- Particles: Tiny particles that block small vessels.
Standalone vs. Preparatory Embolization
Embolization can be a standalone treatment for some AVMs. It’s also used as a preparatory step before surgery. This makes the surgery safer and easier.
Understanding embolization’s role in AVM treatment helps us see the different ways to manage this complex condition.
Are AVMs Genetic? Understanding Causes and Risk Factors
To understand if AVMs are genetic, we need to look at several factors. These include hereditary conditions and cases that happen by chance. We will dive into what we know about the genetic side of arteriovenous malformations.
Hereditary Hemorrhagic Telangiectasia
Hereditary Hemorrhagic Telangiectasia (HHT) is linked to AVMs. It’s also known as Osler-Weber-Rendu syndrome. This genetic disorder causes abnormal blood vessels, including AVMs, in different parts of the body.
People with HHT are more likely to get AVMs. This is true for the brain, lungs, and liver.
Sporadic vs. Inherited AVMs
Not all AVMs come from genetics like HHT. Many happen without a family history. Studies show that sporadic AVMs might be caused by genes and environment together.
Knowing the difference between sporadic and inherited AVMs is key. It helps us find better ways to treat them.
Current Research on Genetic Factors
Scientists are working hard to find the genetic causes of AVMs. New tests and research in molecular biology are helping.
By studying AVMs’ genetics, we can better understand and treat these complex conditions.
Conclusion: Living with AVMs and Future Treatment Directions
Living with an arteriovenous malformation (AVM) means you need to manage it closely. AVMs can really affect your life, so knowing about new treatments is key. AVMs are rare, happening in less than 10.3 per 100,000 people, with a 2% – 4% chance of bleeding each year. For more info on AVMs, including causes and treatments, check out Auctores Online.
We’re all about top-notch healthcare for everyone, including international patients. Our team helps those with AVMs explore their treatment choices. This includes surgery, embolization, and stereotactic radiosurgery (SRS). With ongoing research, we’re excited for new treatments and better management plans.
Keeping up with AVM treatment advances is important. Together, we can improve life for those with AVMs. Our aim is to give full care and support. This way, patients can handle their condition well and live a good life.
FAQ
What does AVM stand for in medical terms?
AVM stands for Arteriovenous Malformation. It’s a condition with an abnormal tangle of blood vessels. This can happen in different parts of the body.
What are the symptoms of a skin AVM?
Skin AVMs can cause visible discoloration and swelling. They might also lead to ulceration or bleeding. If you notice any unusual skin changes, get medical help right away.
Can AVMs occur in the legs or arms?
Yes, AVMs can happen in the legs and arms. They can cause pain and swelling. This might affect your mobility and quality of life.
What is the risk of AVM rupture?
The risk of rupture for unruptured AVMs is about 2-4% each year. The risk of re-rupture is higher, at around 6% in the first year. Several factors can increase this risk.
How are AVMs diagnosed?
Advanced imaging like MRI, CT angiography, and cerebral angiography are used to find and evaluate AVMs. These tests provide detailed information for treatment planning.
What are the treatment options for AVMs?
Treatment options include microsurgical resection and embolization. These can be used alone or together. The choice depends on the AVM’s location, size, and the patient’s individual factors.
Are AVMs genetic?
Some AVMs are linked to genetic conditions, like Hereditary Hemorrhagic Telangiectasia. But many cases are not. Research is ongoing to understand the genetic factors and causes of AVMs.
What is embolization of AVMs?
Embolization is a minimally invasive treatment. It involves delivering materials to block abnormal blood flow in the AVM. This reduces the risk of rupture and can alleviate symptoms.
Can AVMs be treated with surgery?
Yes, microsurgical resection is a treatment option. It involves surgically removing the abnormal blood vessel tangle. The choice of treatment depends on various factors, including the AVM’s location and size.