Last Updated on November 27, 2025 by Bilal Hasdemir

Arteriovenous malformations (AVMs) are unusual connections between arteries and veins. They skip the capillary system and can be found in the skin, legs, and other organs. Knowing about AVMs is key to finding the right treatment.
At Liv Hospital, we offer patient-focused care and the latest treatments for AVMs. Our goal is to provide personalized care and the best results for our patients.
We will look at seven effective treatment methods for AVMs in the leg and skin. This information will help patients make better choices about their care.
Key Takeaways
- Understanding AVMs is vital for effective treatment.
- AVMs can affect various body parts, including the skin and legs.
- Liv Hospital offers patient-centered care and advanced treatment options.
- Seven key methods are available for treating AVMs in the leg and skin.
- Personalized approaches ensure optimal results for patients.
Understanding Arteriovenous Malformations (AVMs)
It’s important to know about arteriovenous malformations (AVMs) to diagnose and treat them. AVMs are abnormal blood vessel formations that can happen anywhere in the body. They disrupt blood flow and can cause health problems.
What Does AVM Stand For in Medical Terms
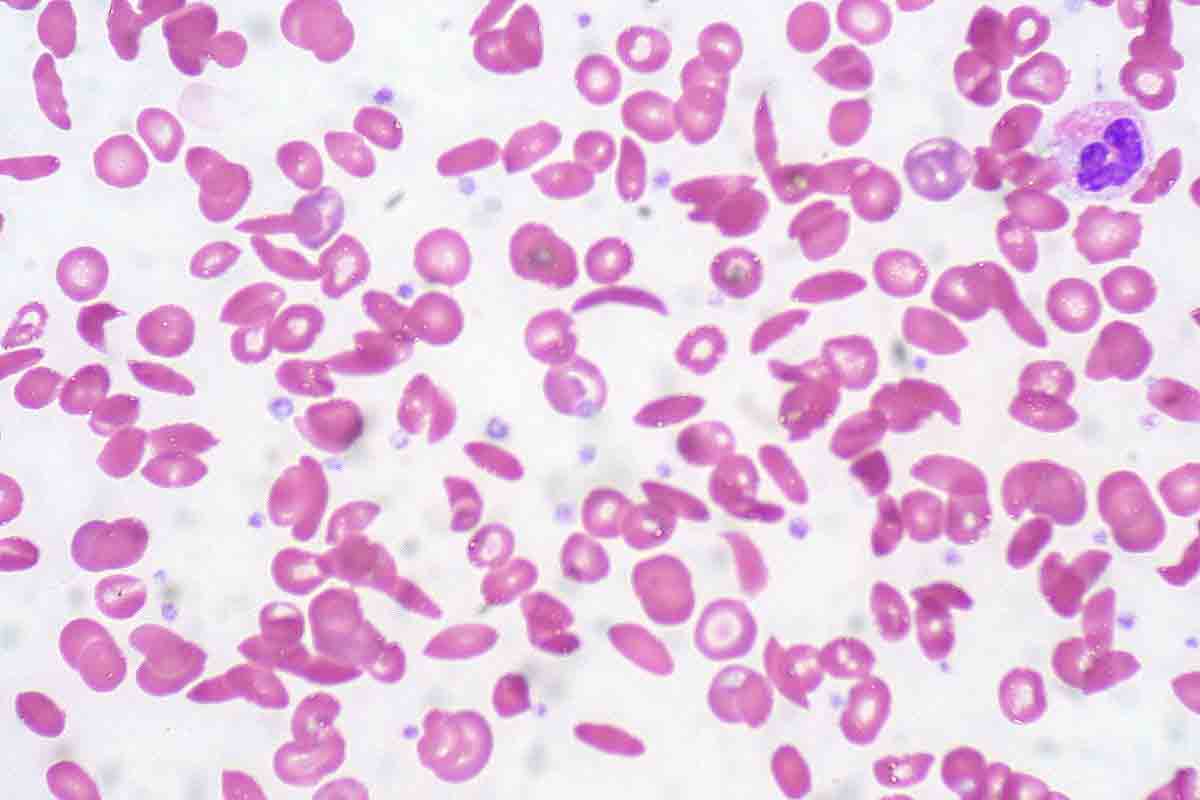
In medical terms, AVM means Arteriovenous Malformation. It’s a condition where arteries and veins connect abnormally. Usually, arteries carry oxygen-rich blood to capillaries, then veins take deoxygenated blood back to the heart. But in an AVM, blood goes straight from arteries to veins, skipping capillaries.
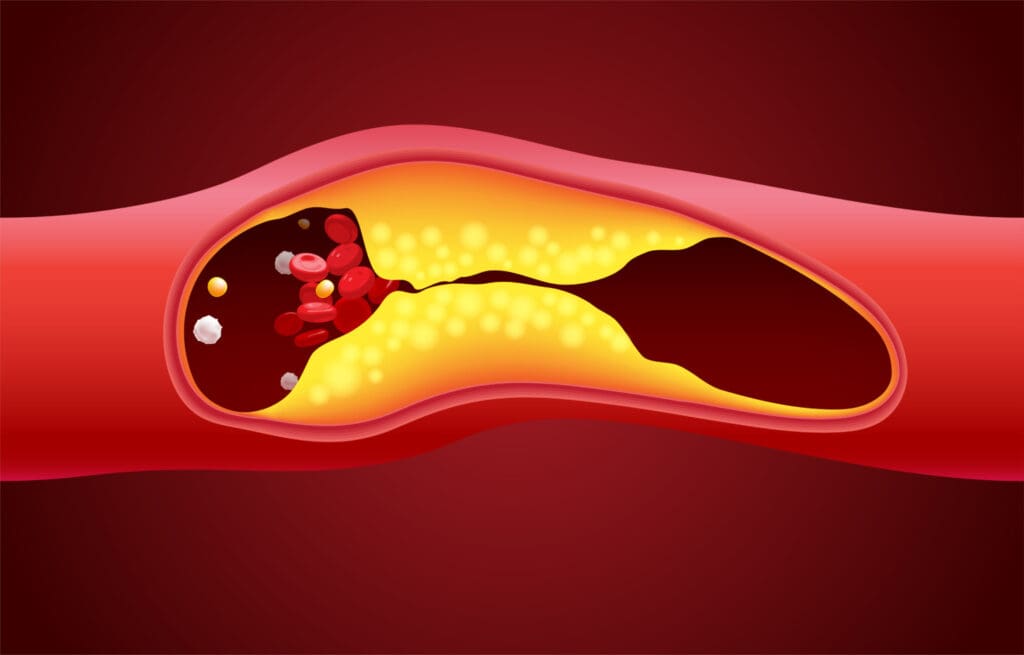
How AVMs Affect the Vascular System
AVMs can harm the vascular system by causing abnormal blood flow. This can lead to swelling, pain, bleeding, and even rupture. These issues can be serious or even life-threatening. AVMs can also cause new, fragile blood vessels to form, raising the risk of more problems.
| Effect on Vascular System | Potential Complications |
|---|---|
| Abnormal blood flow | Swelling, Pain |
| Bypassing capillary system | Bleeding, Ulceration |
| Formation of new fragile vessels | Rupture, Life-threatening conditions |
Understanding AVMs and their effects on blood vessels helps doctors create good treatment plans. This way, they can manage symptoms and prevent serious issues.
Common Locations and Types of AVMs
AVMs can appear in many parts of the body, like the skin, legs, and other organs. Doctors and researchers have found where AVMs usually show up. This knowledge is key for figuring out what’s wrong and how to fix it.
Skin AVMs: Characteristics and Presentation
Skin AVMs happen in the skin. They might look like a visible lesion or a color change. Sometimes, they cause pain or bleeding.
These skin AVMs have abnormal connections between arteries and veins. They are near the skin’s surface.
Leg AVMs: Unique Features and Concerns
AVMs in the leg can be serious. They might cause pain, swelling, and trouble moving. Leg AVMs can also lead to ulcers or bleeding, which is risky.
It’s important to know how leg AVMs work. This helps doctors manage them better.
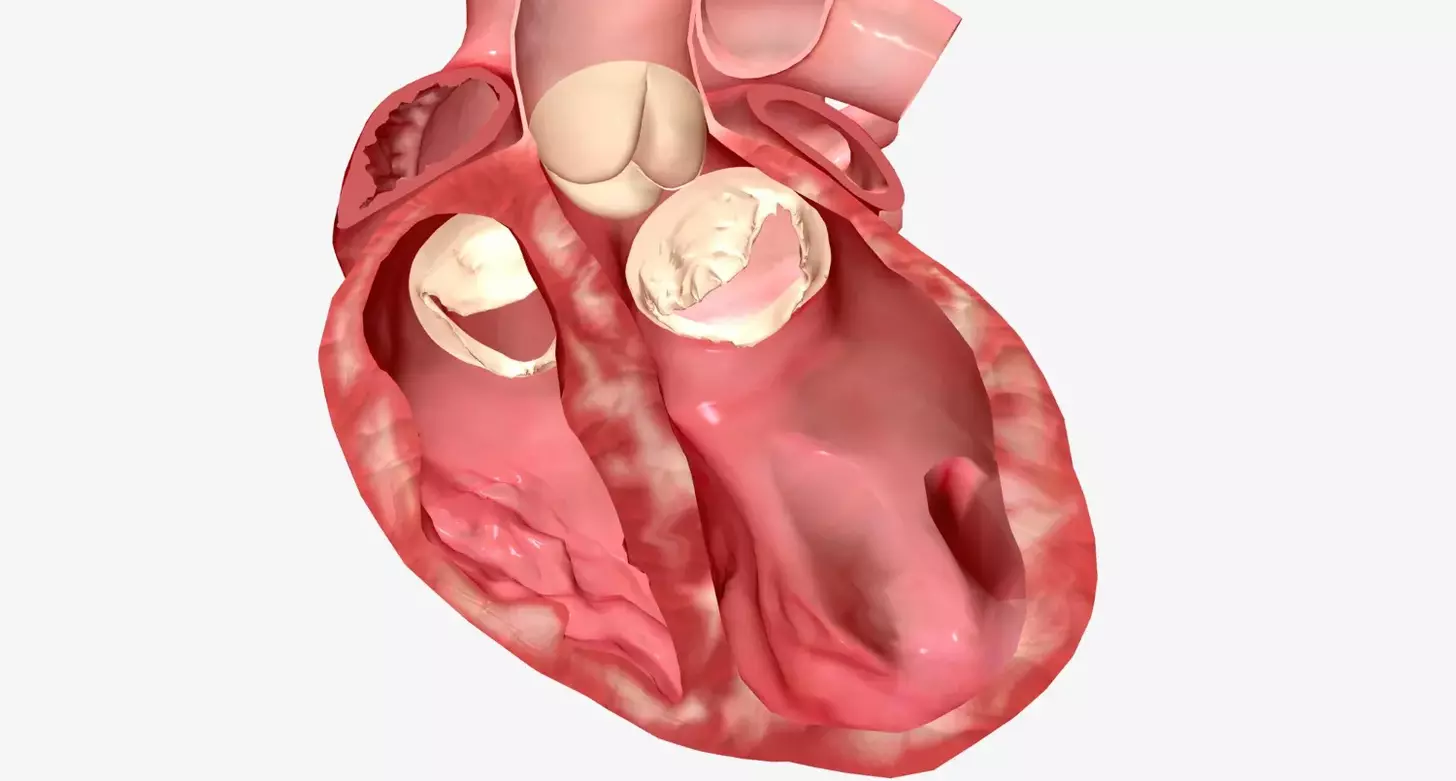
AVMs in Other Body Regions (Heart, Arms, Torso)
AVMs can also show up in the heart, arms, and torso. Each place has its own set of problems. For example, heart AVMs are tricky because they’re close to important heart parts.
Doctors need to tackle AVMs in all parts of the body in a detailed way. Knowing where and how AVMs occur helps doctors come up with the best treatment plans.
Symptoms and Complications of Untreated AVMs
Untreated Arteriovenous Malformations can cause serious health problems. It’s important to get medical help quickly. AVMs are abnormal connections between arteries and veins. They can lead to symptoms and serious conditions if not treated.
Early Warning Signs of AVMs
Finding AVMs early is key to avoiding serious issues. Early warning signs include swelling, pain, or color changes in the affected area. AVMs in the brain or spine can cause numbness, tingling, or weakness.
AVMs in the leg or skin might make the limb look different. You might see it’s warmer or have more visible veins. Spotting these signs early can help get the right treatment fast.
Bleeding AVMs: Risk Assessment and Management
Bleeding is a big risk with AVMs, more so for those that are close to the surface. Bleeding AVMs can cause a lot of blood loss, needing quick medical care. Doctors look at the AVM’s size, location, and type to figure out the bleeding risk.
To manage bleeding AVMs, doctors use embolization and sclerotherapy. Sometimes, surgery is needed to take out the AVM or fix damaged blood vessels.
Potential for AVM Rupture and Associated Dangers
The risk of AVM rupture is very serious. It can cause huge bleeding, damage to organs, and even death. The size, location, and history of bleeding are key factors.
Knowing the risks of AVM rupture shows why early treatment is so important. People with AVMs need close monitoring and treatment plans that fit their needs and risks.
Causes and Risk Factors of Arteriovenous Malformations
AVMs are caused by a mix of genetic, environmental, and developmental factors. Knowing these causes helps in creating better treatment plans and setting realistic expectations for patients.
Are AVMs Genetic? Understanding Hereditary Factors
Research shows that genetics play a role in some AVMs. Certain genetic disorders, like Hereditary Hemorrhagic Telangiectasia (HHT), raise the risk of AVMs. HHT is marked by multiple AVMs in organs like the lungs, liver, and brain.
Studies have found specific genetic mutations linked to AVMs. For example, mutations in the ENG, ACVRL1, and SMAD4 genes are tied to HHT and AVMs. While not all AVMs are genetic, knowing the genetic link helps in early detection and management.
| Genetic Disorder | Associated Gene Mutation | AVM Risk |
|---|---|---|
| Hereditary Hemorrhagic Telangiectasia (HHT) | ENG, ACVRL1, SMAD4 | High |
| Capillary Malformation-Arteriovenous Malformation Syndrome | RASA1 | Moderate |
Acquired and Developmental Arteriovenous Malformation Causes
Not all AVMs are genetic; some are acquired or developmental. Trauma, infection, and environmental factors can cause AVMs.
Developmental AVMs happen during fetal development. Abnormal vascular system formation leads to AVMs. While the exact causes are not fully known, genetics and environment both play a part.
Understanding AVM causes and risk factors is key to effective treatments. By identifying the factors behind AVMs, healthcare providers can tailor treatments. This improves outcomes and lowers complication risks.
Diagnostic Approaches for AVM Detection
Diagnosing AVMs involves several steps, from a first check-up to detailed scans like MRI. We use a detailed process to find and check arteriovenous malformations accurately.
Physical Examination and Initial Assessment
The first step is a detailed physical check-up. We look at the patient’s health history and do a clinical check. This helps us spot signs of an AVM, like unusual blood vessels or swelling.
MRI for AVM Diagnosis and Mapping
Magnetic Resonance Imaging (MRI) is key in finding AVMs. It shows us the malformation’s details, like size and where it is. MRI is great because it can show the AVM’s structure without needing contrast agents in some cases.
Additional Imaging Techniques for Complete Evaluation
We also use other scans to get a full picture of the AVM. These include:
- Angiography to see the blood vessels and flow in the AVM
- Ultrasound to check blood flow and find any issues
- CT scans to look at the AVM’s structure and how it affects nearby tissues
These tests help us plan the best treatment. By combining findings from physical checks, MRI, and other scans, we get a clear view of the AVM. Then, we can make a treatment plan that fits the patient’s needs.
| Diagnostic Technique | Primary Use in AVM Diagnosis | Benefits |
|---|---|---|
| Physical Examination | Initial assessment, identifying signs of AVM | Non-invasive, quick, and cost-effective |
| MRI | Detailed imaging of AVM structure and extent | High-resolution images, no radiation |
| Angiography | Visualizing blood vessels and flow within the AVM | Detailed vascular structure information |
AV Malformation Treatment: Overview of 7 Key Therapeutic Approaches
Treating arteriovenous malformations (AVMs) needs a detailed plan. We use many treatment options based on the malformation’s details. AVM treatment is not the same for everyone. It depends on the malformation’s type, location, and how severe it is.
Treatment Selection Criteria for Different AVM Types
Choosing the right treatment for AVMs involves several factors. These include the AVM’s type, where it is, its size, and the patient’s health. We use these details to pick the best treatment.
- Type of AVM: Different AVMs need different treatments. For example, some might be treated with sclerotherapy, while others might need embolization or surgery.
- Location: Where the AVM is located affects the treatment choice. AVMs in hard-to-reach places might need more precise, less invasive methods.
- Size and Severity: Bigger or more serious AVMs often need a mix of treatments for the best results.
Multidisciplinary Treatment Planning
Planning AVM treatment involves a team of experts. This team includes interventional radiologists, vascular surgeons, and others. Together, we create a treatment plan that meets each patient’s needs.
| Treatment Modality | Description | Typical Use Cases |
|---|---|---|
| Embolization | Minimally invasive procedure to block blood flow to the AVM | Large or complex AVMs, high-risk AVMs |
| Sclerotherapy | Injection of a sclerosing agent to close off the AVM | Superficial AVMs, small to medium-sized AVMs |
| Surgical Resection | Surgical removal of the AVM | Accessible AVMs, failed or incomplete embolization/sclerotherapy |
Measuring Treatment Success and Outcomes
We check if AVM treatment worked by looking at several things. These include how the patient feels, what imaging studies show, and what the patient says. Good treatment means fewer symptoms, better quality of life, and no complications.
By using a detailed and team-based approach to AVM treatment, we can help patients get better. This way, we provide the best care for those with arteriovenous malformations.
Embolization and Sclerotherapy for AVM Management
Embolization and sclerotherapy are key treatments for arteriovenous malformations (AVMs). These methods are less invasive than traditional surgery. They offer safe and effective ways to manage AVMs.
AVM Embolization: Procedure, Benefits, and Limitations
AVM embolization uses a catheter to deliver materials into the AVM. The goal is to block the abnormal blood vessels. It can be used alone or with other treatments.
This method is less invasive, reducing risks compared to surgery. It’s also good for AVMs in hard-to-reach spots. But, it might not remove the AVM completely, and there’s a chance it could come back.
Key aspects of AVM embolization include:
- Precision in targeting the AVM
- Minimally invasive, reducing recovery time
- Potential for combination with other treatments
Sclerotherapy for Superficial Skin AVMs
Sclerotherapy injects a sclerosing agent into the AVM. This causes it to shrink or disappear. It’s best for AVMs on the surface of the skin.
Sclerotherapy is beneficial because it’s simple and can be done without staying in the hospital. It has a low risk of serious side effects. But, it might need to be done more than once and works best for surface AVMs.
Advantages of sclerotherapy for superficial AVMs include:
- Minimally invasive with quick recovery
- Effective for superficial lesions
- Can be performed on an outpatient basis
Embolization and sclerotherapy are important for AVM management. They offer various treatment options based on each patient’s needs. Knowing the pros and cons of each helps us give personalized care that improves outcomes.
Surgical and Mechanical AVM Interventions
Surgical methods are key in treating arteriovenous malformations (AVMs). We’ll look at the various surgical and mechanical ways to tackle AVMs. This includes traditional surgery, endovascular techniques, and compression therapy.
Conventional Surgical Removal of AVMs
Traditional surgery is used for AVMs that are easy to reach and not too big. Surgical removal of AVM is chosen when the malformation is causing problems or could bleed a lot.
We check if surgery is possible based on the AVM’s size, where it is, and the patient’s health. Our goal is to remove the AVM completely without harming nearby tissues.
Endovascular Surgical Techniques
Endovascular surgery for AVM is a less invasive option compared to open surgery. It involves going through blood vessels to get to the AVM.
Endovascular methods include embolization, where materials are used to block blood flow to the AVM. This can be done alone or with other treatments to shrink the malformation and ease symptoms.
| Technique | Description | Benefits |
|---|---|---|
| Embolization | Blocking blood flow to the AVM | Reduces AVM size, alleviates symptoms |
| Sclerotherapy | Inducing clotting within the AVM | Effective for superficial AVMs |
Compression Therapy for Leg and Extremity AVMs
Compression therapy for AVM is great for leg and extremity AVMs. It uses pressure to help manage symptoms. This is done with special garments or devices.
Compression therapy can lessen swelling, ease pain, and improve movement. It’s often used along with other treatments. It’s a good long-term plan for patients with AVMs in their legs or arms.
We customize compression therapy for each patient. We adjust the pressure and type of garment based on the AVM’s size and location.
Conclusion: Advances in AVM Treatment and Patient Outlook
Recent breakthroughs in treating arteriovenous malformations (AVMs) have greatly improved patient care. These advances help doctors understand AVMs better. This knowledge leads to more effective treatments.
Thanks to new therapies like embolization and sclerotherapy, patients have more options. These treatments, along with surgery, have made life better for those with AVMs. They help improve the quality of life for many.
The future of AVM treatment is bright. Ongoing research aims to make treatments even better. As we learn more, we’ll see even better care for those with AVMs.
Healthcare providers are working hard to keep up with these advances. This means they can give patients the best care possible. It improves patients’ outlook and quality of life.
FAQ
What does AVM stand for in medical terms?
AVM stands for Arteriovenous Malformation. It’s a condition where arteries and veins connect abnormally. This disrupts normal blood flow.
What is an Arteriovenous Malformation?
An Arteriovenous Malformation (AVM) is a vascular anomaly. It’s an abnormal connection between arteries and veins. This connection bypasses the capillary system, leading to health issues.
Are AVMs genetic?
The exact cause of AVMs is not fully understood. But, genetic factors might play a role in their development. Some AVMs are linked to genetic disorders.
What are the symptoms of an AVM?
Symptoms of AVMs vary based on their location and size. Common symptoms include pain, swelling, and visible lesions or discoloration. In severe cases, AVMs can cause bleeding or rupture.
How are AVMs diagnosed?
Diagnosing AVMs involves a physical exam and imaging tests like MRI. Sometimes, additional imaging is needed to assess the AVM’s extent and characteristics.
What is the role of MRI in diagnosing AVMs?
MRI is key in diagnosing AVMs. It provides detailed images. These images help determine the AVM’s size, location, and how it affects surrounding tissues.
What are the treatment options for AVMs?
Treatment options for AVMs include embolization, sclerotherapy, and surgical removal. The choice depends on the AVM’s type, location, and size.
What is embolization of AVM?
Embolization is a minimally invasive procedure. It involves injecting materials into the AVM to block blood flow. This aims to reduce its size and alleviate symptoms.
Can AVMs rupture, and what are the dangers?
Yes, AVMs can rupture, leading to life-threatening bleeding. The risk of rupture depends on the AVM’s characteristics. Managing this risk is critical in AVM treatment.
How is treatment success measured for AVMs?
Success in treating AVMs is measured by symptom reduction, AVM size reduction, and improved quality of life.
REFERENCES
- PMC – “Vascular malformations: An overview of their molecular pathways, detection of mutational profiles and subsequent targets for drug therapy”. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9950274 PMC
- PMC – “Targeted therapies for vascular malformations”. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11405217 PMC