Last Updated on November 26, 2025 by Bilal Hasdemir
A dying bowel, also known as bowel gangrene or intestinal gangrene, is a life-threatening condition. It happens when the intestine loses blood supply, causing tissue death.Understand dying bowel symptoms, causes, and gangrene risks you need to know.
This severe condition often results from sudden colonic infarction. It needs immediate medical attention to prevent high mortality rates. Knowing the symptoms and causes is key for timely treatment.
At Liv Hospital, we are committed to delivering world-class, patient-centered care in complex gastrointestinal emergencies, including bowel gangrene.
Key Takeaways
- Understanding the severity of a dying bowel is key for prompt treatment.
- Bowel gangrene is a life-threatening condition needing immediate medical attention.
- Colonic infarction is a main cause of intestinal gangrene.
- Recognizing symptoms early can greatly improve treatment outcomes.
- Liv Hospital provides specialized care for gastrointestinal emergencies.
What is a Dying Bowel? Understanding Intestinal Gangrene

A dying bowel, also known as intestinal gangrene, is a serious condition that needs quick action. It happens when the blood flow to the intestines is cut off, causing tissue necrosis.
Medical Definition and Terminology
Intestinal gangrene is when the intestines die due to lack of blood or infection. Terms like bowel infarction and gangrene of the bowel are used to describe this. They mean the intestines have died because of no blood flow.
Knowing these terms is key for doctors to spot and treat this condition right.
The Pathophysiology of Intestinal Tissue Death
The cause of intestinal gangrene is when blood stops flowing to the intestines, leading to death. This can happen for many reasons like blockages or strangulation. Without blood, the intestines get damaged and eventually die.
Understanding how this happens is important for finding ways to treat intestinal gangrene.
The Dying Bowel: Mechanisms and Critical Timeline

Blood supply disruption to the intestine is a medical emergency. It can lead to irreversible damage if not treated quickly. The bowel is very sensitive to blood flow changes. Knowing how tissue death happens is key for quick action.
How Blood Supply Disruption Leads to Tissue Death
The intestine needs a steady flow of oxygenated blood to stay healthy. Without it, the tissue becomes ischemic. This starts a chain of cell damage.
- Reduced Oxygen Delivery: The first sign is less oxygen reaching the intestinal tissue.
- Accumulation of Toxic Metabolites: As it goes on, the tissue starts to break down, making harmful substances.
- Inflammatory Response: The damaged tissue sets off an inflammatory response, which can harm the bowel more.
Progression from Ischemia to Irreversible Damage
The move from ischemia to gangrenous bowel is complex. At first, the injury might be fixable. But, as time goes on, the damage becomes permanent.
How fast this happens depends on several things. These include how bad the blood supply issue is and any health problems the person has. Important steps in this process are:
- The start of ischemia, when tissue injury begins.
- The point when damage is no longer reversible, usually a few hours after ischemia starts.
- The development of bowel infarction, where tissue dies and might even burst.
Doctors need to understand these steps and the timeline to act fast. This could save a patient’s life.
Primary Causes of Bowel Infarction and Gangrene
Knowing why bowel infarction happens is key to quick medical help. It happens when the intestine’s blood supply is cut off, causing tissue death. Several main factors lead to this, like arterial embolism, thrombosis, bowel strangulation, and mesenteric venous thrombosis.
Arterial Embolism and Thrombosis
Arterial embolism and thrombosis are big reasons for bowel infarction. An arterial embolism happens when a blood clot or particle blocks an artery to the intestine. Thrombosis is when a blood clot forms in the arteries or veins of the bowel. Both can cause ischemia and intestinal tissue death.
Things that increase the risk of these include:
- Atrial fibrillation
- Atherosclerosis
- Cardiac valve disorders
- Hypercoagulable states
Bowel Strangulation and Volvulus
Bowel strangulation is when a part of the intestine gets cut off by constriction. This can be due to hernias, adhesions, or volvulus. A volvulus is when a part of the intestine twists around its mesentery, blocking blood vessels and causing ischemia.
The main reasons for bowel strangulation are:
- Hernias
- Adhesions from previous surgeries
- Volvulus
Mesenteric Venous Thrombosis
Mesenteric venous thrombosis is when a blood clot forms in the veins draining the intestine. This can cause bowel infarction by blocking venous outflow, leading to congestion and ischemia.
Risk factors for mesenteric venous thrombosis include:
- Hypercoagulable states
- Inflammatory conditions such as pancreatitis
- Recent surgery
- Cirrhosis and portal hypertension
In conclusion, bowel infarction and gangrene come from several critical causes that disrupt the intestine’s blood supply. Knowing these causes is vital for early diagnosis and treatment.
High-Risk Populations for Gangrenous Intestine
It’s important to know who is most at risk for gangrenous intestine. Some groups face a higher risk due to age, health issues, and lifestyle choices.
Age-Related Vulnerabilities
Older adults are more likely to get gangrenous intestine. Age-related declines in cardiovascular health and more health problems play a role. As people get older, they’re more likely to have issues that affect blood flow to the intestines, like atherosclerosis.
Cardiovascular Conditions and Hypercoagulability
Those with heart problems are at a higher risk for gangrenous intestine. Conditions like atrial fibrillation, heart failure, and peripheral artery disease can cause problems with blood flow to the intestines. This increases the risk of ischemia and gangrene. Also, being prone to blood clots, due to genetics or certain meds, raises this risk even more.
Chronic Gastrointestinal Disorders
People with long-term gut problems are also at high risk. Conditions like inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis, can lead to complications. These can include bowel obstruction or volvulus, which can cause gangrenous intestine. Other long-term issues, like diverticulitis, can also increase the risk by causing bowel strangulation or other problems.
It’s key to know who’s at high risk to act early. Healthcare providers should keep a close eye on these groups. They should provide quick diagnosis and treatment to stop gangrenous intestine before it starts.
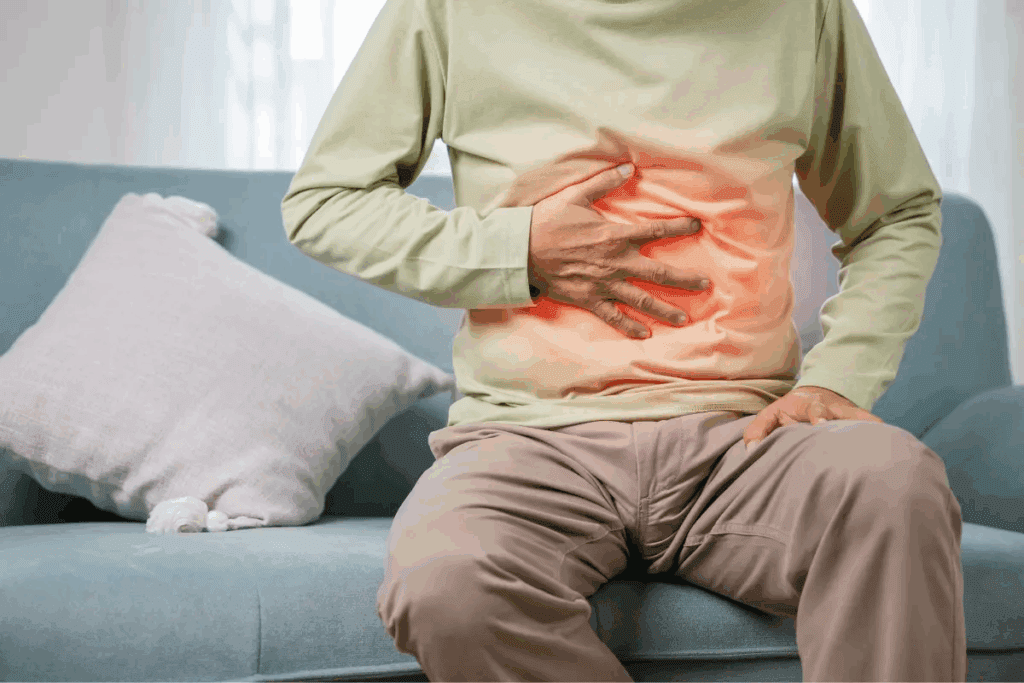
Recognizing Gangrenous Bowel Symptoms: Warning Signs
It’s vital to know the warning signs of gangrenous bowel to get medical help quickly. Symptoms can get worse fast, so spotting them early is key.
Early Clinical Manifestations
The first signs of gangrenous bowel can be tricky to spot. They might look like other issues. Look out for:
- Severe abdominal pain, often out of proportion to physical examination findings
- Nausea and vomiting
- Abdominal tenderness
- Fever
These signs can be similar to other problems. So, a detailed check-up is important.
Progressive Symptom Development
As gangrene gets worse, symptoms can get more severe. You might see:
- Increased abdominal pain and guarding
- Signs of intestinal obstruction, such as abdominal distension and constipation
- Tachycardia and hypotension, indicating possible sepsis
Clinical deterioration can happen fast. This shows why quick diagnosis and treatment are so critical.
Signs of Systemic Involvement and Sepsis
In severe cases, gangrenous bowel can spread and cause sepsis. Look out for:
| Signs | Symptoms |
| Tachycardia | Rapid heart rate |
| Hypotension | Low blood pressure |
| Fever or hypothermia | Abnormal body temperature |
| Confusion or altered mental status | Signs of severe sepsis |
Spotting these signs is vital. Sepsis is a serious condition that needs quick medical care.
Going from local bowel gangrene to widespread sepsis shows the importance of being alert and acting fast with patients suspected of gangrenous bowel.
Diagnostic Approaches for Infarcted Bowel
To diagnose an infarcted bowel, doctors use several methods. These include clinical checks, lab tests, and imaging studies. This detailed approach helps find the problem quickly and accurately.
Clinical Evaluation and Laboratory Markers
Doctors start by looking at the patient’s history and symptoms. They also do a physical exam. Lab tests are key in supporting the diagnosis. Important tests include:
- Complete Blood Count (CBC) to check for signs of infection or inflammation
- Blood chemistry tests to assess electrolyte imbalances and metabolic acidosis
- Lactate levels, as elevated lactate can indicate tissue ischemia
- C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) to assess inflammation
These tests, while not alone enough, give important clues when looked at with the patient’s symptoms.
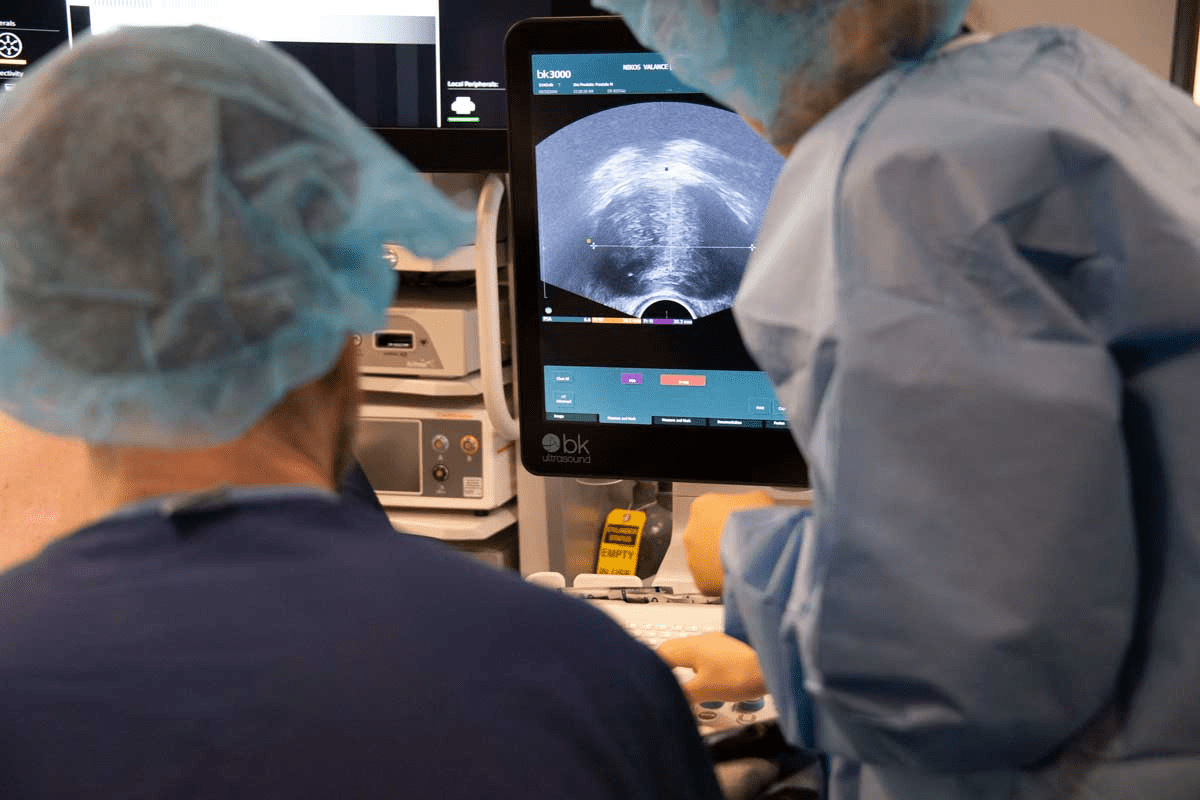
Imaging Studies for Bowel Ischemia and Necrosis
Imaging is vital for spotting bowel ischemia and necrosis. The right imaging depends on the situation and what’s available. Common methods include:
| Imaging Modality | Key Features | Advantages |
| Computed Tomography (CT) | Shows bowel wall thickening, pneumatosis, and portal venous gas | High sensitivity and specificity for diagnosing bowel ischemia |
| Plain Abdominal Radiography | May show signs of bowel obstruction or pneumatosis | Quick and readily available |
| Magnetic Resonance Imaging (MRI) | Can assess bowel wall viability and mesenteric vessels | No radiation exposure |
Exploratory Laparotomy and Direct Visualization
If tests and imaging don’t show what’s wrong, surgery might be needed. An exploratory laparotomy lets doctors see the bowel directly. It’s very helpful for patients who are very sick and need quick help.
Doctors usually choose surgery when they think the bowel might be infarcted and the patient needs help right away.
Emergency Treatment for Gangrene of the Bowel
Managing gangrene of the bowel needs a detailed emergency plan. It starts with initial resuscitation. This condition is very serious and needs quick action.
Initial Resuscitation and Stabilization
The first step is to stabilize the patient. This includes giving fluids, fixing electrolyte levels, and antibiotics to stop sepsis.
“Prompt resuscitation is critical in managing bowel gangrene, as it helps stabilize the patient and prepares them for further treatment,” as emphasized by medical professionals.
Surgical Interventions and Techniques
Surgery is key in treating gangrene of the bowel. The main goal is to remove the dead bowel part to stop more damage and sepsis.
- Resection of the affected bowel segment
- Restoration of intestinal continuity when possible
- Creation of a stoma if necessary
Antimicrobial Therapy for Sepsis Management
Antimicrobial therapy is vital for sepsis management in gangrene of the bowel. Broad-spectrum antibiotics are given first, then targeted therapy based on test results.
Effective antimicrobial therapy is key to lowering sepsis risk and better patient outcomes.
“The use of appropriate antimicrobial agents is vital in the management of bowel gangrene, as it helps control infection and prevent further complications.”
– Medical Expert
Complications and Outcomes of Colonic Infarction
The outcomes of colonic infarction depend on several factors. These include the extent of the infarction, how quickly and effectively treatment is given, and the patient’s overall health.
Short-term Complications and Management
Colonic infarction can cause serious short-term problems. Sepsis is a big concern because bacteria can spread from the infarcted bowel into the blood. Prompt surgical intervention is often needed to remove the infarcted segment and prevent further issues.
Other short-term problems include perforation of the infarcted bowel, leading to peritonitis, and hemorrhage due to erosion of blood vessels. Managing these complications usually involves surgery, antibiotics, and supportive care.
Long-term Health Implications
Survivors of colonic infarction may face long-term health issues. Malabsorption and nutritional deficiencies can happen if a big part of the colon is removed or doesn’t work right. Patients might need ongoing nutritional support and monitoring.
There’s also a chance of adhesions and bowel obstruction after surgery. Long-term follow-up with a healthcare provider is key to manage these risks and improve the patient’s quality of life.
Mortality Rates and Prognostic Factors
The mortality rate for colonic infarction is high, mainly if diagnosis and treatment are delayed. Prognostic factors that affect mortality include the extent of the infarction, the patient’s age, and any underlying health conditions.
A study on colonic infarction outcomes showed the following mortality rates:
- 30-day mortality: 20-30%
- 1-year mortality: 40-50%
Knowing these prognostic factors helps tailor treatment approaches to improve patient outcomes.
Preventive Strategies for High-Risk Individuals
Preventive strategies are key in managing the risk of gangrenous bowel for vulnerable groups. By focusing on managing underlying conditions and using surveillance protocols, healthcare providers can lower the risk. They also explore new ways to prevent gangrenous bowel in high-risk individuals.
Management of Underlying Conditions
Managing underlying conditions is vital to prevent gangrenous bowel. Conditions like cardiovascular disease, diabetes, and chronic gastrointestinal disorders raise the risk. By managing these conditions well, through medication and lifestyle changes, the risk can be lowered.
For example, managing cardiovascular disease means controlling blood pressure and cholesterol levels. It also means ensuring the right amount of blood thinners. For diabetic patients, keeping blood sugar levels in check can prevent vascular problems.
Surveillance Protocols for At-Risk Patients
Surveillance protocols are another important preventive strategy. Regular checks can catch signs of gangrenous bowel early. This allows for quick action. These checks include imaging studies, monitoring for bowel obstruction signs, and looking for symptoms of bowel ischemia.
| Surveillance Method | Description | Frequency |
| Imaging Studies | CT scans or MRI to assess bowel viability and detect early signs of ischemia | As clinically indicated, typically every 6-12 months |
| Symptom Monitoring | Patient education on recognizing symptoms of bowel obstruction or ischemia | Ongoing, with regular follow-up visits |
| Laboratory Tests | Monitoring for markers of inflammation or ischemia | Every 3-6 months or as clinically indicated |
Emerging Preventive Approaches
New research offers hope in preventing gangrenous bowel. It includes new medicines, better surgery techniques, and regenerative medicine to improve bowel health.
By using a mix of managing conditions, surveillance, and new strategies, healthcare providers can lower gangrenous bowel risk in high-risk groups.
Conclusion: Advancing Care for Intestinal Gangrene
Improving care for intestinal gangrene is key to better patient results. This condition, where tissue dies due to poor blood flow, needs quick diagnosis and treatment.
Managing intestinal gangrene well means spotting symptoms early, acting fast with surgery, and using the right antibiotics. We also need more research to understand and treat this condition better.
By improving care for intestinal gangrene, doctors can lower the risks and deaths from it. Looking ahead, we aim to find new ways to diagnose and treat it. This will help improve patient care and results.
FAQ
What is a dying bowel?
A dying bowel, also known as intestinal gangrene or bowel infarction, happens when the intestine’s blood supply is severely cut off. This leads to tissue death and can be very dangerous.
What are the primary causes of bowel infarction and gangrene?
The main causes are arterial embolism, thrombosis, bowel strangulation, and mesenteric venous thrombosis. These can all cut off the intestine’s blood supply, causing tissue death.
Who is at high risk for gangrenous intestine?
People with heart conditions, blood clotting disorders, chronic gut problems, and older age are more likely to get gangrenous intestine.
What are the warning signs of gangrenous bowel?
Early signs include severe stomach pain, nausea, vomiting, and fever. These can grow into signs of infection spreading, like fast heart rate, low blood pressure, and confusion.
How is infarcted bowel diagnosed?
To diagnose, doctors use clinical checks, lab tests, and imaging like CT scans and angiography. They also do exploratory surgery to see the bowel and check damage.
What is the emergency treatment for gangrene of the bowel?
First, they stabilize the patient. Then, they do surgery to remove dead tissue. They also use antibiotics to fight infection and prevent more problems.
What are the complications and outcomes of colonic infarction?
Short-term problems include sepsis and organ failure. Long-term, there can be malabsorption and chronic gut issues. How well someone does depends on quick treatment and their overall health.
Can gangrenous bowel be prevented?
Yes, by managing health conditions and watching at-risk patients closely. New ways to prevent bowel infarction and gangrene are also being explored.
What is the role of antimicrobial therapy in managing gangrenous bowel?
Antibiotics are key in fighting sepsis and preventing more problems. They target the bacteria from dead bowel tissue.
How does bowel strangulation lead to gangrene?
Bowel strangulation happens when a part of the intestine gets cut off. This stops blood flow, leading to ischemia, necrosis, and gangrene if not treated quickly.
What are the signs of systemic involvement in gangrenous bowel?
Signs include fast heart rate, low blood pressure, fever, and confusion. These show the infection has spread and is affecting the whole body.