Last Updated on November 26, 2025 by Bilal Hasdemir

Colonoscopy is the top choice for finding and treating colon cancer. But, Do I Need a Colonoscopy? Key Facts
Liv Hospital puts patients first, making sure every colonoscopy is really needed. They focus on keeping patients safe and following the latest medical rules. Some health issues might make a colonoscopy unnecessary or unsafe. It’s important to know about these issues.
This article will explain when a colonoscopy might not be needed or should be canceled. It’s meant to help both patients and doctors understand better.
Key Takeaways
- Colonoscopy is a vital tool for colorectal cancer screening.
- Specific contraindications may make a colonoscopy unnecessary.
- Patient-centered approaches prioritize safety and medical standards.
- Understanding when to cancel a colonoscopy is important.
- Certain conditions may make a colonoscopy unsafe.
The Purpose and Role of Colonoscopy in Modern Medicine
Colonoscopy is a key tool in the battle against colorectal cancer. It offers both diagnosis and treatment benefits. This method has changed gastroenterology, allowing doctors to see inside the colon, find issues, and remove harmful polyps.
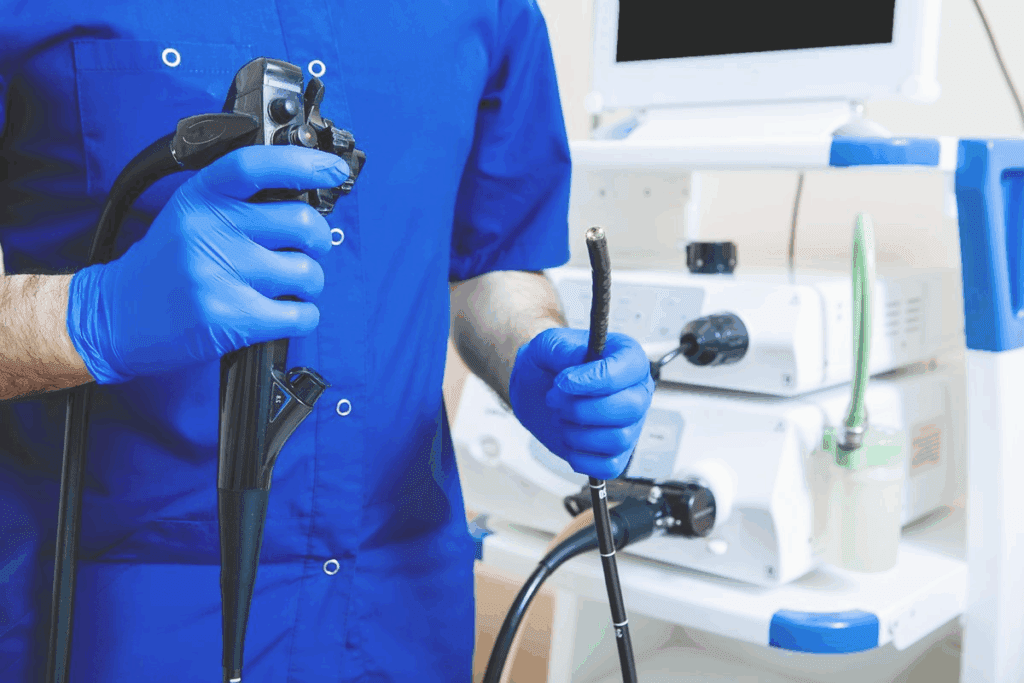
What is a Colonoscopy and How is it Performed?
A colonoscopy uses a long, flexible tube with a camera to look at the colon. It’s done under sedation to make the process easier. Doctors can spot polyps, cancer, and other problems. They can also remove polyps and take biopsies for more checks.
The steps for a colonoscopy include:
- Preparation: Patients follow a special diet and bowel prep to clean the colon.
- Sedation: The procedure is done with conscious sedation to keep patients comfortable.
- Insertion of the colonoscope: The tube is gently put into the rectum and moved through the colon.
- Examination: The doctor looks for any issues in the colon.
- Interventions: If problems are found, they can be treated during the procedure.
Standard Recommendations for Colorectal Cancer Screening
The United States Preventive Services Task Force suggests colonoscopy every 10 years for those 50 to 75 with average risk. Guidelines can change based on risk, family history, and health. Regular screenings help catch cancer early and prevent it.
It’s important to talk to your doctor about the right screening schedule for you.
Do I Need a Colonoscopy? Understanding Appropriate Indications

Deciding on a colonoscopy depends on age, medical history, and risk factors. This ensures the screening helps those who need it most.
Age-Based Screening Guidelines
Age plays a big role in colonoscopy needs. People with average risk should start screening at 45. Screening guidelines suggest a colonoscopy every 10 years for those with no risk factors or family history of colorectal cancer.
Those with a family history or other risk factors might need different schedules. It’s key to talk to a healthcare provider for the right screening plan.
- Average risk individuals: Start screening at age 45
- Screening interval for average risk: Every 10 years
- Individuals with family history or risk factors: Consult healthcare provider for personalized schedule
High-Risk Factors That Warrant Earlier Screening
Some factors mean you might need to get screened sooner or more often. These include a family history of colorectal cancer, personal history of the disease or polyps, and certain genetic syndromes.
High-risk factors that might need earlier screening include:
- A family history of colorectal cancer, specially in first-degree relatives
- A personal history of colorectal cancer or adenomatous polyps
- Known or suspected genetic syndromes like Lynch syndrome or Familial Adenomatous Polyposis (FAP)
- Inflammatory bowel disease (IBD), including ulcerative colitis or Crohn’s disease
People with these risk factors might need to start screening before 45 and have it more often. The exact timing and frequency depend on individual risk assessment by a healthcare provider.
Knowing these guidelines and risk factors is key to making smart choices about colonoscopy. By focusing on those at higher risk, healthcare providers can catch and prevent colorectal cancer early.
Medical Conditions That Necessitate Colonoscopy
Colonoscopy is key for people with certain health issues that raise their risk of colorectal cancer. These include alarm symptoms and chronic conditions that need regular checks.
Alarm Symptoms That Should Not Be Ignored
Alarm symptoms point to serious health problems. They often mean a colonoscopy is needed to find out why.
- Rectal Bleeding: Bleeding from the rectum can be a sign of colorectal cancer or other significant issues.
- Unexplained Weight Loss: Unintentional weight loss, when paired with other stomach problems, needs to be checked.
- Changes in Bowel Habits: Persistent changes in bowel habits, such as diarrhea or constipation, can indicate a need for colonoscopy.
- Abdominal Pain: Persistent or severe abdominal pain may require a colonoscopy to rule out colorectal pathology.
Chronic Conditions Requiring Regular Surveillance
Certain chronic conditions raise the risk of colorectal cancer. They need regular checks with colonoscopy.
- History of Colorectal Cancer or Adenomatous Polyps: Those with a history of colorectal cancer or adenomatous polyps need regular colonoscopies.
- Inflammatory Bowel Disease (IBD): Patients with IBD, including Crohn’s disease and ulcerative colitis, are at increased risk and may require more frequent colonoscopies.
- Family History of Colorectal Cancer: Those with a significant family history of colorectal cancer may benefit from earlier and more frequent screening.
For example, those with a history of colorectal cancer need colonoscopies at 1, 3, and 5-year intervals. Then, they get routine screenings. This approach helps keep high-risk people closely monitored.
Who Should Not Have a Colonoscopy? Absolute Contraindications
Colonoscopy is a key tool for diagnosing health issues. Yet, there are times when it’s not safe. Knowing when not to have a colonoscopy is key for safety and good health.
Severe Active Colonic Inflammation
Severe active colonic inflammation is a big no-no for colonoscopy. This is common in severe ulcerative colitis or Crohn’s disease. It raises the risk of serious problems like perforation.
Doing a colonoscopy on someone with severe inflammation can cause more harm. This could lead to serious issues.
Fulminant colitis is another dangerous condition. It’s when the colon gets very inflamed. In such cases, colonoscopy is usually avoided because of the high risk of perforation.
Other Absolute Contraindications
There are other conditions where colonoscopy is not safe. These include:
- Complete large bowel obstruction caused by tumors or strictures. This makes the procedure risky and hard to do.
- Acute diverticulitis or diverticular perforation with abscess formation. Colonoscopy could make things worse or lead to more problems.
- Active inflammatory bowel disease with a high risk of injury and perforation during the exam.
In these cases, other tests like CT scans or MRI might be better. They can check the condition without the risks of colonoscopy.
Doctors must look at a patient’s medical history and current health. They need to talk about the risks and benefits of colonoscopy with their patients.
Medical Reasons to Cancel a Scheduled Colonoscopy
Deciding to cancel a colonoscopy often comes down to acute medical conditions or recent surgeries. A patient’s health is key to the procedure’s success and safety.
Acute Medical Conditions
Some acute medical issues make colonoscopies risky. These include:
- Recent myocardial infarction
- Acute renal failure
- Decompensated hepatic disease
- Coagulopathies and bleeding disorders
- Hemodynamic instability
- Peritonitis
For example, someone with recent myocardial infarction faces higher risks of heart problems during the procedure.
| Acute Medical Condition | Risks Associated with Colonoscopy |
| Recent Myocardial Infarction | Cardiac complications, hemodynamic instability |
| Acute Renal Failure | Electrolyte imbalance, fluid overload |
| Decompensated Hepatic Disease | Coagulopathy, hepatic encephalopathy |
Recent Surgical Procedures
Recent surgeries, like colorectal anastomoses, can also lead to canceling a colonoscopy. The worry is about disrupting healing or causing problems at the surgery site.
For instance, someone who had colorectal surgery might have to wait until their doctor says it’s safe to have a colonoscopy.
Healthcare providers can make better decisions about canceling colonoscopies. This ensures patient safety and the right timing for the procedure.
When Colonoscopies Are Unnecessary: Avoiding Overtesting
In recent years, there’s been a growing awareness about overtesting with colonoscopies. This is true, mainly for younger people or those at lower risk for colorectal cancer. It’s important to find a balance between the benefits of colonoscopy and its risks and costs.
Low-Risk Individuals Under Age 45
For those under 45, the risk of colorectal cancer is lower. The benefits of a colonoscopy might not be worth the risks and discomforts. The United States Preventive Services Task Force (USPSTF) suggests starting routine screening at age 45 for those with average risk.
So, for low-risk individuals under 45, a colonoscopy is usually not needed unless there are specific risk factors or symptoms.
Inappropriate Use of Colonoscopy
Colonoscopy is sometimes used inappropriately. This can happen when it’s done too often or in people with a low risk of colorectal cancer. It’s also seen as inappropriate when it’s used as a routine follow-up for patients with non-neoplastic polyps without looking at other risk factors.
The following table summarizes scenarios where colonoscopy might be considered unnecessary or inappropriate:
| Scenario | Rationale |
| Patients under 45 without risk factors | Low risk of colorectal cancer |
| Patients over 85 with limited life expectancy | Limited benefit due to age and health status |
| Frequent colonoscopies without new symptoms or risk factors | Overtesting and unnecessary risk |
By avoiding unnecessary colonoscopies, healthcare providers can lower the risk of complications and cut healthcare costs. It’s key for both patients and healthcare providers to have open discussions about the need for colonoscopy. This should be based on individual risk factors and health status.
Addressing Concerns: Are Colonoscopies Really Necessary?
The debate on colonoscopies is ongoing. It’s key to look at the evidence of their benefits. Colonoscopies are seen as the top choice for finding colorectal cancer early.
Examining the Evidence for Colonoscopy Benefits
Colonoscopies are better at finding problems than other tests like barium enemas or CT scans. The proof of their benefits includes:
- Early Detection: They help find colorectal cancer early, which can lead to better treatment.
- Prevention: By removing polyps, they can stop cancer from happening.
- Diagnostic Accuracy: They let doctors see the colon directly, making diagnosis more accurate.
Common Misconceptions About Colonoscopies
There are myths about colonoscopies that need clearing up. Some of these are:
- It’s too invasive: Though it’s invasive, it’s usually okay with the right sedation.
- It’s not necessary for everyone: Only people at risk or over 45 should get screened, based on guidelines.
- Alternative tests are just as good: While other tests are useful, colonoscopies are the best because they’re so accurate.
Knowing the truth about colonoscopy benefits and myths helps both patients and doctors make better choices for screening.
Alternative Screening Methods for Colorectal Cancer
Screening for colorectal cancer has changed, giving patients more choices than just colonoscopy. Now, there are non-invasive tests that can find cancer or polyps before they become serious. These options are great for those who can’t or don’t want to have a colonoscopy.
Non-Invasive Testing Options
There are several non-invasive tests for colorectal cancer screening. These include:
- Fecal Immunochemical Test (FIT): This test finds hidden blood in the stool, which could mean cancer or big polyps.
- Stool DNA Test: This test looks for DNA changes in the stool that might show cancer or big polyps.
These tests are done at home, making them easier and less scary for many. But, it’s key to follow the test instructions well to get good results.
When to Consider Alternatives to Colonoscopy
Think about alternatives to colonoscopy based on your risk, what you prefer, and your health history. For example:
- People with a low risk of colorectal cancer might start with non-invasive tests.
- Those who had a colonoscopy with no issues might choose less often or different tests.
- Those who are nervous about colonoscopy or had a bad experience might like other options better.
Talking to your doctor is important to find the best screening for you.
Conclusion: Making Informed Decisions About Colonoscopy
Doctors need to think carefully about when to do a colonoscopy. They must balance the good it can do against the risks. It’s important to know when a colonoscopy isn’t needed.
Deciding on a colonoscopy means knowing when it’s right and when it’s not. It also means looking at other ways to check for cancer. Patients and doctors should work together to find the best screening method.
Patients can make smart choices by looking at their own risks and health history. They should also follow the latest guidelines. This way, they get care that’s right for them.
FAQ
What is a colonoscopy and why is it performed?
A colonoscopy lets a doctor see inside the whole colon. It helps find polyps, cancer, and other issues. It’s often used to screen for colorectal cancer.
Who should not have a colonoscopy?
People with severe colonic inflammation, certain health issues, or at risk of complications should avoid it. Always talk to a doctor first.
Are colonoscopies really necessary for everyone?
No, not everyone needs a colonoscopy. It depends on age, health history, and risk for colorectal cancer. Young, low-risk people might not need it.
What are the risks associated with colonoscopy?
Colonoscopies are mostly safe but can cause bleeding, colon perforation, or sedation reactions. Certain health conditions may raise these risks.
Can I cancel a scheduled colonoscopy?
Yes, you can cancel if there’s a valid medical reason, like a sudden illness or recent surgery. Always check with your doctor.
Are there alternative screening methods for colorectal cancer?
Yes, there are other tests like stool tests and CT colonography. The choice depends on your risk and preferences.
How often should I have a colonoscopy?
The timing of colonoscopies varies based on your risk, health history, and past results. Usually, a normal result means waiting 10 years for the next one.
Is a colonoscopy necessary if I have no symptoms?
Yes, even without symptoms, colonoscopies can find polyps and cancer early. Guidelines suggest starting at age 45 for those at average risk.
Can I refuse a colonoscopy?
Yes, you can refuse. But, it’s important to talk to your doctor about the risks and benefits to make an informed choice.
Are colonoscopies a scam?
No, colonoscopies are not a scam. They are a proven way to prevent and detect colorectal cancer. While there are risks, the benefits are clear
References
Khalil, H. M., et al. (2021). Biliary leakage following cholecystectomy: A prospective population study. Journal of Research in Medical and Dental Science, 9(5), 289-296. Retrieved from https://www.jrmds.in/articles/biliary-leakage-following-cholecystectomy-a-prospective-population-study-84919.html