Last Updated on November 27, 2025 by Bilal Hasdemir
Imagine going through a surgery where you must stay awake and alert. This lets your medical team watch and protect your brain functions as they happen.
At Liv Hospital, safety and the newest medical tech are key in every awake craniotomy surgery. This makes recovery safer and more precise.
We’ll take you through the main points of awake brain surgery. You’ll learn about its definition, benefits, and risks. This will give you a full picture of this complex medical process.
Key Takeaways
- Understanding the concept of awake craniotomy and its significance in modern neurosurgery.
- The benefits of being awake during brain surgery, including improved outcomes and reduced risks.
- The role of advanced medical technology in improving patient safety and recovery.
- The expertise and care provided by medical teams at specialized hospitals like Liv Hospital.
- The importance of patient education and support throughout the surgical process.
What Is Brain Operation Awake: Definition and Medical Purpose
Awake brain surgery is a new way for doctors to work on the brain while the patient is awake. This method is used for serious brain issues, like problems with language or movement. It helps doctors avoid harming important brain parts.
This surgery has many benefits. It lets doctors see exactly what they’re doing and keep important brain areas safe. This is key when working on parts of the brain that control language or movement.
The Science Behind Awake Craniotomy
The magic of awake craniotomy is in its ability to give feedback during surgery. Patients can do tasks that help doctors understand the brain’s layout. This real-time brain mapping helps doctors avoid harming important brain spots.
Doctors use special tools to watch the brain’s activity during surgery. They might use ECoG to see electrical signals or fMRI to map brain functions. These tools, along with the patient’s responses, help create a detailed brain map.
Historical Development of the Procedure
Awake brain surgery has been around for a century. But, new tech and better techniques have made it more advanced and accepted.
It started in the 1930s with Wilder Penfield, who used brain stimulation to map brain functions. Over time, it has grown, using new tools and methods to help patients more. Now, awake craniotomy is a key part of neurosurgery, helping avoid brain damage and improve recovery.
As neurosurgery keeps getting better, awake brain surgery stays at the top of new methods. It combines precise surgery with feedback from the patient. This makes it a powerful tool for treating complex brain issues while keeping important brain functions safe.
Key Fact #1: Brain Operation Awake Protects Critical Brain Functions
Awake brain surgery has changed neurosurgery a lot. It lets surgeons keep important brain functions safe during surgery. This new way of surgery helps doctors do complex tasks without harming key brain areas.
Mapping Language and Motor Areas
One big plus of awake brain surgery is mapping language and motor areas live. Surgeons keep patients awake to check their brain functions right then. This is key to finding and keeping safe the brain parts for talking, moving, and more.
We use special brain mapping to find these important spots. We stimulate brain parts and see how the patient reacts. For example, if a patient names objects when a certain brain area is active, we know it’s important for language.
Real-Time Neurological Feedback Benefits
The feedback from awake brain surgery is very helpful. It lets surgeons adjust their plan right away to avoid harming key brain areas. This feedback is key for the best results for patients having brain surgery.
With this feedback, we can make the surgery fit the patient’s brain perfectly. This makes the surgery more precise, lowering the chance of problems after surgery. Patients can then heal faster and with fewer issues.
The benefits of awake brain surgery are many:
- It’s more precise in finding and keeping safe important brain areas.
- It lowers the chance of lasting brain damage.
- It leads to better results because of the feedback during surgery.
- It’s tailored to each patient’s brain, making the surgery more effective.
Thanks to these benefits, awake brain surgery is a safer and more effective way to treat complex brain surgeries.
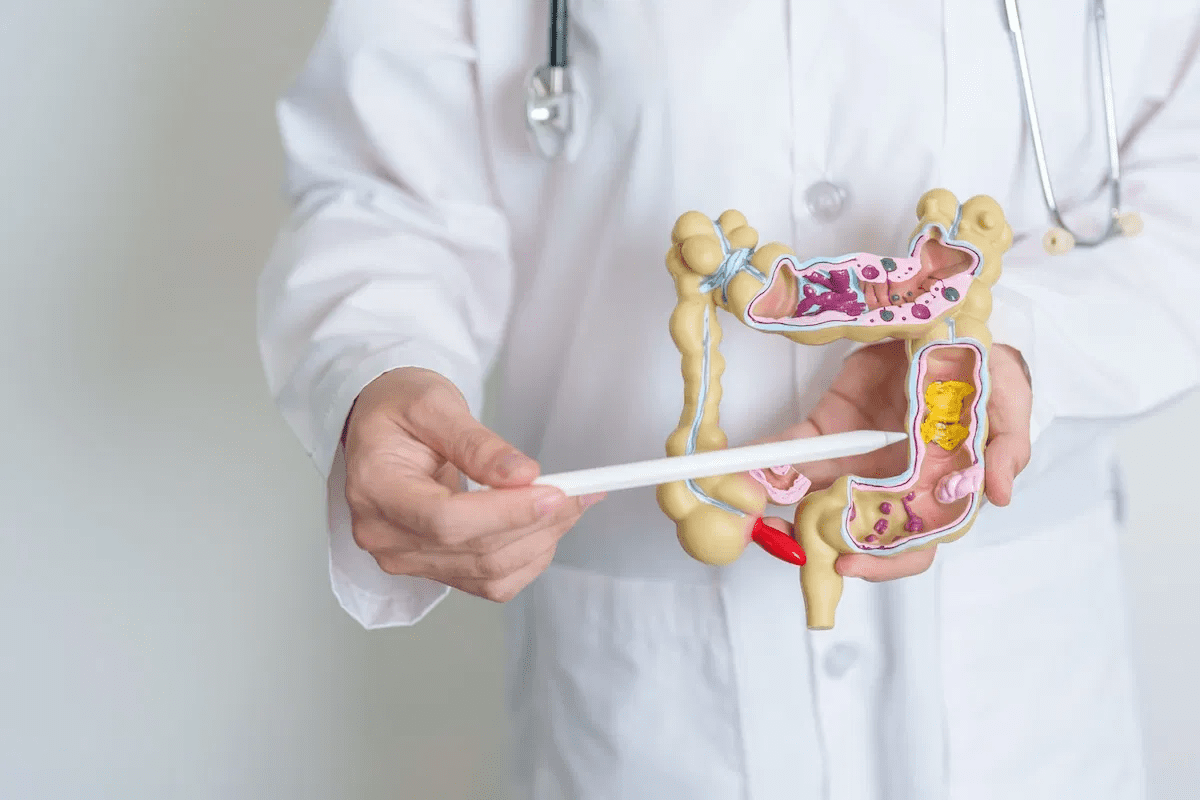
Key Fact #2: Medical Conditions That Require Awake Brain Surgery
Awake brain surgery is key for treating serious brain conditions. It lets doctors watch and protect important brain parts in real time. This makes it a vital tool for complex brain issues.
Brain Tumors in Functional Areas
Brain tumors in key brain areas need awake brain surgery. This method helps doctors remove tumors without harming nearby brain tissue. Awake brain tumor removal is now the top choice for tumors in important areas, lowering the chance of brain problems after surgery.
Awake brain surgery is very precise. It keeps the patient awake so doctors can check brain functions during surgery. This way, they avoid damaging important brain areas.
Epilepsy and Other Neurological Disorders
Awake brain surgery also helps with epilepsy and other brain disorders. For epilepsy, the goal is to find and remove the seizure source without harming other brain areas. This surgery lets doctors map brain activity in real time, helping them find and remove the seizure area.
The table below lists medical conditions that might need awake brain surgery and its benefits:
| Medical Condition | Benefits of Awake Brain Surgery |
|---|---|
| Brain Tumors in Functional Areas | Preservation of critical brain functions, precise tumor removal |
| Epilepsy | Real-time mapping of seizure focus, reduced risk of neurological damage |
| Other Neurological Disorders | Enhanced precision in identifying and treating affected brain areas |
Knowing when awake brain surgery is needed helps patients and doctors choose the best treatment. As technology improves, awake brain surgery will play an even bigger role in treating complex brain conditions.
Key Fact #3: Not Everyone Is a Suitable Candidate
Awake brain surgery is not for everyone. It depends on medical and psychological factors. We check each patient to see if they can have this surgery.
Medical Criteria for Patient Selection
The criteria for choosing patients are strict. We look at the type and location of the brain tumor or lesion. We also check the patient’s health and medical history.
For example, people with heart problems or those at risk for seizures might not qualify.
Psychological Requirements
Psychological tests are key in choosing patients. We see if they can stay calm and follow instructions during surgery. Those with severe anxiety or psychiatric conditions might need more checks or other treatments.
Contraindications for Awake Craniotomy
Some conditions make awake craniotomy not possible. These include severe claustrophobia, inability to cooperate due to mental or cognitive issues, and significant respiratory or cardiovascular instability.
We also look at where the tumor or lesion is. For example, those near the brainstem might not be good for awake surgery.
In summary, deciding if someone can have awake brain surgery involves a detailed check. We look at their health, mental state, and specific reasons why they might not be a good candidate. This way, we can make sure the surgery is safe and effective for those who need it.
Key Fact #4: Patients Are Not Awake for the Entire Surgery
Even though it’s called ‘awake brain surgery,’ patients aren’t awake the whole time. This surgery uses different levels of anesthesia to keep patients comfortable and ensure the surgery goes well.
The Three Phases of Anesthesia
Patients go through three main stages during awake brain surgery. First, they get sedated to relax before the surgery starts. Then, they’re awake for the most important parts, like brain mapping and removing tumors. Lastly, they’re sedated again for the surgery’s end.
The three phases are carefully managed to balance patient comfort with surgical requirements. The anesthesiologist controls the transition between these phases to make sure the surgery is smooth and safe.
Conscious Sedation Techniques
Conscious sedation is key in awake brain surgery. It uses sedatives to relax the patient without making them lose consciousness. The goal is to keep them comfortable and able to follow commands during the surgery. Different medications can be used, depending on the patient’s health and the surgery’s needs.
Pain Management During the Procedure
Managing pain is very important during awake brain surgery. The team uses local anesthesia to numb the scalp and other areas where pain might happen. The anesthesiologist also keeps an eye on the patient’s comfort and adjusts the sedation as needed. This mix of local anesthesia and conscious sedation helps reduce pain during the surgery.
| Anesthesia Phase | Patient State | Purpose |
|---|---|---|
| Initial Sedation | Sedated | Relaxation before surgery |
| Awake Phase | Conscious | Brain mapping and tumor removal |
| Final Sedation | Sedated | Closing stages of surgery |
Knowing about the different anesthesia phases and pain management in awake brain surgery helps patients prepare better. It also helps them know what to expect during the procedure.
The Step-by-Step Process of Brain Operation Awake
Learning about awake brain surgery can ease worries for patients and their families. This surgery, also known as awake craniotomy, is a complex procedure. It needs careful planning and precision.
Pre-Surgical Preparation and Planning
The first step is detailed pre-surgical preparation. We thoroughly evaluate the patient’s medical history, brain health, and imaging studies. This helps us find the best way to remove the tumor or lesion without harming the brain.
Next, we prepare the patient mentally. We explain the surgery, their role, and what to expect. This helps reduce anxiety and ensures the patient can cooperate during the surgery.
The Critical Mapping Phase
When the patient is ready, we start the critical mapping phase. We identify and map key brain areas for language, movement, and other important functions. The patient stays awake and responds, allowing us to check their brain functions live.
By stimulating brain areas and watching the patient’s reactions, we define the boundaries of critical brain regions. This is key to safely removing the tumor or lesion without harming the brain.
Tumor or Lesion Removal Techniques
With the brain areas mapped, we remove the tumor or lesion. We use the mapping data to remove the tissue carefully, avoiding damage to the brain.
The surgical team uses advanced tools and techniques for precision. The patient’s feedback is essential, helping us adjust our approach to remove the tumor while keeping brain functions intact.
Closing Stages of the Surgery
After removing the tumor or lesion, we close the surgery. We close the dura mater, replace the bone flap, and sew the scalp. The patient is then under general anesthesia for the rest of the closure.
We closely watch the patient after surgery, managing pain and any complications. The care in these final stages is vital for a smooth recovery and the best results.
Key Fact #5: What Patients Actually Experience During the Procedure
Going through awake brain surgery can be scary. But knowing what to expect can help ease worries. Being well-informed is key to getting ready for this complex surgery.
Physical Sensations During Surgery
Patients might feel different things during awake brain surgery. We make sure they’re comfortable and know what’s happening. They might feel pressure or vibrations during the craniotomy.
But, thanks to local anesthesia, pain is usually minimal. Some might feel numbness or tingling in certain areas. This depends on where in the brain the surgery is happening.
Communication Between Patient and Surgical Team
Good communication is very important during awake brain surgery. We keep talking to make sure patients are safe and comfortable. The team will often ask how the patient is doing.
This helps the team make any needed changes. Talking openly is key to a successful surgery.
Tasks Patients Perform During Brain Mapping
Patients do specific tasks during brain mapping. We help them understand what’s expected. These tasks might include naming objects or counting.
They might also be asked to move their limbs. These tasks help the team find important brain areas. By doing these tasks, patients help make their surgery a success.
Knowing about physical sensations, communication, and tasks helps patients prepare. We’re here to give full care and support every step of the way.
Key Fact #6: Improved Outcomes Compared to Traditional Surgery
Neurosurgeons are now choosing awake brain surgery more often. This is because it can lead to better results. Awake brain surgery has many benefits over traditional surgery, mainly in patient outcomes.
One big advantage is that it allows for higher rates of complete tumor removal. Surgeons can keep the patient awake. This lets them map brain functions and find the tumor’s edges more accurately.
Higher Rates of Complete Tumor Removal
Research shows awake brain surgery is better for removing tumors. The team can get feedback from the patient in real time. This helps them avoid damaging important brain areas.
The table below shows how awake brain surgery compares to traditional surgery in tumor removal rates.
| Study | Awake Brain Surgery | Traditional Surgery |
|---|---|---|
| Study 1 | 85% | 65% |
| Study 2 | 90% | 70% |
| Study 3 | 88% | 68% |
Reduced Risk of Permanent Neurological Damage
Awake brain surgery also lowers the risk of permanent brain damage. Surgeons can watch the patient’s brain functions live. This lets them make quick changes to avoid harming the brain.
This live monitoring helps avoid neurological problems after surgery. It’s a big plus for patients.
Evidence-Based Outcome Comparisons
Many studies have looked at awake brain surgery versus traditional surgery. They all show awake brain surgery leads to improved patient outcomes. This includes more complete tumor removal and less brain damage.
Choosing awake brain surgery means patients get the newest neurosurgical techniques. This can lead to a better recovery and a better life.
Potential Risks and Complications to Consider
It’s important to know the risks of awake brain surgery before making a decision. This procedure has many benefits, but it’s good to be aware of possible challenges.
Intraoperative Seizures and Management
Intraoperative seizures are a big risk during awake brain surgery. These seizures can happen during the mapping process or the surgery itself. To handle this, surgical teams use:
- Antiepileptic medications before and during surgery
- Continuous monitoring of the patient’s brain
- Techniques to cool the brain or apply specific medications
Managing seizures well is key to keeping patients safe and the surgery successful.
Neurological Complications
Neurological problems can happen during awake brain surgery. These include:
- Damage to brain tissue
- Swelling or bleeding in the brain
- Infection
To lower these risks, surgeons use advanced imaging and precise mapping. Good planning and execution help avoid neurological problems.
Psychological Effects and Emotional Challenges
Being awake during brain surgery can be tough on patients emotionally. Anxiety, fear, and the need to be involved can affect their mind. To help, many places offer:
- Pre-operative counseling to prepare patients
- Support during the surgery from psychologists
- Post-operative care to help patients deal with their experience
Offering full psychological support is a big part of caring for patients during awake brain surgery.
Anesthesia-Related Risks
Even though patients are awake, anesthesia is used at times. Risks include:
- Respiratory problems
- Allergic reactions to anesthetics
- Waking up at the wrong time during surgery
An experienced anesthesia team plans and monitors carefully. Good teamwork between surgeons and anesthesiologists is essential for safety.
Recovery Timeline After Awake Brain Surgery
Recovering from awake brain surgery takes time. It includes immediate care, a hospital stay, and long-term rehab. Knowing these steps helps patients prepare for what’s next.
Immediate Post-Operative Experience
The first days after surgery are key. Patients are watched closely for any changes or problems. They might feel tired, have headaches, or feel confused, but these feelings usually go away.
Here are some common things patients might feel right after surgery:
- Numbness or tingling in parts of the body
- Difficulty with speech or language processing
- Weakness in limbs
- Mild cognitive disturbances
Hospital Stay Duration and Care
How long a patient stays in the hospital varies. Most stay 2 to 7 days after surgery. Our team gives them the best care, including watching their brain, managing pain, and helping with physical therapy.
| Day | Care Focus |
|---|---|
| 1-2 | Neurological monitoring and pain management |
| 2-3 | Physical therapy and mobilization |
| 3-7 | Continued care and preparation for discharge |
Long-Term Recovery and Rehabilitation
Recovering from awake brain surgery can take weeks to months. Rehab is a big part of getting better. Our team helps patients get back to normal with a plan that includes physical, occupational, and speech therapy.
Many things can affect how long recovery takes. These include the patient’s health, how big the surgery was, and how well they follow their rehab plan. Seeing our team regularly is important to check on progress and solve any issues.
Knowing what to expect after awake brain surgery helps patients prepare. Our team is here to support them every step of the way, aiming for the best results.
Key Fact #7: Recent Advances Improving Awake Brain Surgery
The field of awake brain surgery is changing fast. New methods and tools are being added all the time. These changes make the awake brain surgery procedure safer and more effective, leading to better results for patients.
Technological Innovations in Surgical Techniques
New tech has changed awake brain surgery a lot. One big step is using MRI and CT scans during surgery. This lets surgeons see the brain clearly in real-time. It helps them remove tumors more accurately and avoid harming important brain areas.
Robotic-assisted surgery is another big leap. These robots give surgeons more control and precision. They also help see the brain better, which is key during awake craniotomies.
Advanced Brain Mapping Methods
New brain mapping methods have changed how surgeons plan and do awake brain surgeries. Tools like functional MRI, diffusion tensor imaging, and electrocorticography create detailed brain maps. These maps help surgeons know which areas to keep safe during surgery.
Intraoperative brain mapping also lets surgeons watch brain function live during surgery. This lets them make changes as needed to avoid brain damage.
| Mapping Technique | Description | Benefits |
|---|---|---|
| fMRI | Functional MRI maps brain activity | Identifies critical brain areas |
| DTI | Diffusion Tensor Imaging maps white matter tracts | Preserves neural pathways |
| ECoG | Electrocorticography records electrical activity | Monitors brain function in real-time |
Latest Research on Patient Outcomes
Recent studies show the benefits of awake brain surgery. They show better results and less risk of brain damage. Patients who have awake craniotomies often have tumors removed completely and have fewer lasting brain problems than those under general anesthesia.
Also, better pain management and anesthesia make the surgery more comfortable for patients. Research also points to the importance of a team approach to care. This includes neurologists, neurosurgeons, and rehab specialists to help patients recover best.
We are dedicated to using the latest medical tech and care for our patients. By keeping up with the latest research and innovations, we make sure our patients get the best care possible.
Conclusion: Making Informed Decisions About Awake Brain Surgery
Exploring the seven key facts about awake brain surgery shows it’s a complex but beneficial procedure. It helps patients with certain neurological conditions. Understanding its benefits, risks, and process helps patients make informed decisions.
Awake brain surgery protects important brain functions by giving real-time feedback during the surgery. This method has improved results for patients with brain tumors and other neurological disorders. New technologies and brain mapping methods are making awake brain surgery safer and more effective.
Patients thinking about awake brain surgery should talk to their healthcare provider. This way, they can decide if it’s right for them and know what to expect. We aim to provide top-notch healthcare and support for international patients, ensuring they get the best care.
FAQ
What is awake brain surgery?
Awake brain surgery, also known as awake craniotomy, is a surgical procedure. The patient stays awake during part of the operation. This allows surgeons to map and protect critical brain functions.
Why is awake brain surgery performed?
It’s used to treat brain tumors, epilepsy, and other neurological disorders. These are located in functional areas of the brain. It helps preserve critical brain functions.
What are the benefits of awake brain surgery?
The benefits include higher rates of complete tumor removal. It also reduces the risk of permanent neurological damage. Plus, outcomes are often better than traditional brain surgery.
Am I a suitable candidate for awake brain surgery?
Not everyone is right for awake brain surgery. The decision depends on medical criteria, psychological requirements, and the absence of contraindications.
Will I be awake for the entire surgery?
No, you won’t be awake the whole time. Awake brain surgery has three phases of anesthesia. Conscious sedation techniques manage pain and discomfort during the procedure.
What can I expect during awake brain surgery?
You might feel physical sensations during the surgery. You’ll also be asked to perform tasks. This helps the surgical team identify and preserve critical brain functions.
What are the possible risks and complications of awake brain surgery?
Risks include intraoperative seizures and neurological complications. There are also psychological effects, emotional challenges, and anesthesia-related risks.
How long is the recovery process after awake brain surgery?
Recovery involves an immediate post-operative experience and a hospital stay. It also includes a long-term recovery and rehabilitation process.
Are there any recent advances improving awake brain surgery?
Yes, there are. Technological innovations, advanced brain mapping methods, and research on patient outcomes are improving the surgery’s safety and efficacy.
How can I make informed decisions about awake brain surgery?
To make informed decisions, understand the benefits, risks, and process of awake brain surgery. Also, know the medical conditions that require this type of surgery.
References
Journal of the Medical Students’ Association (JMSMA): The Top 10 Facts You Need to Know About Awake Craniotomy