Last Updated on November 27, 2025 by Bilal Hasdemir

Thinking about a complex medical procedure can be scary. But awake brain surgery, or awake craniotomy, is a special method. It lets patients stay awake and help during their surgery.
This surgery is key for safety and success, mainly for tumors or seizures near important areas. Being awake helps the team get the best results for the patient.
At Liv Hospital, we focus on the patient during awake brain surgery. It’s a big deal for our patients. Our team works hard to give each patient the best care.
Key Takeaways
- Awake brain surgery allows patients to remain conscious during part of their operation.
- This technique is vital for the surgery’s safety and success.
- Patients can help their team during the surgery, leading to better results.
- Liv Hospital puts patients first in awake brain surgery.
- Our team ensures each patient gets top-notch care.
Understanding Awake Brain Surgery: A Medical Marvel
Awake brain surgery might sound scary, but it’s a key part of modern neurosurgery. This complex surgery needs a team working together closely. We’ll look into what awake brain surgery is, why it’s done, and how it’s evolved to be safer and more effective.
Definition and Purpose of Awake Craniotomy
Awake craniotomy, or neurosurgery awake patient procedure, is a surgery where the patient stays awake. This lets surgeons watch brain functions live, keeping important areas safe. The main goal is to remove tumors or lesions near these areas without harming them.
Keeping the patient awake helps surgeons. They can talk to the patient and use special techniques to map brain functions. This feedback helps them remove tumors or lesions more accurately. A famous neurosurgeon once said,
“The awake craniotomy procedure represents a significant advancement in neurosurgery, enabling us to operate with greater precision and safety.”
Historical Development of the Procedure
The idea of conscious brain surgery started in the early 20th century. But it wasn’t until the 1960s and 1970s that awake craniotomy became a real option. New anesthesia and monitoring tools have helped it grow. Now, awake craniotomy is common in many places, making brain surgery safer for patients.
There have been big steps forward in awake brain surgery. Better ways to choose patients, new surgical methods, and better care after surgery have all helped. These changes have made awake brain tumor surgery a top choice for many doctors.
When Is Brain Surgery While Awake Necessary?
Brain surgery while awake is needed for certain medical conditions. This method, known as awake craniotomy, lets neurosurgeons work on the brain when the patient is awake. It’s a precise technique.
This method is key when dealing with conditions that impact important brain areas. These areas control speech, movement, and sensation. Keeping the patient awake helps surgeons avoid damaging these areas.
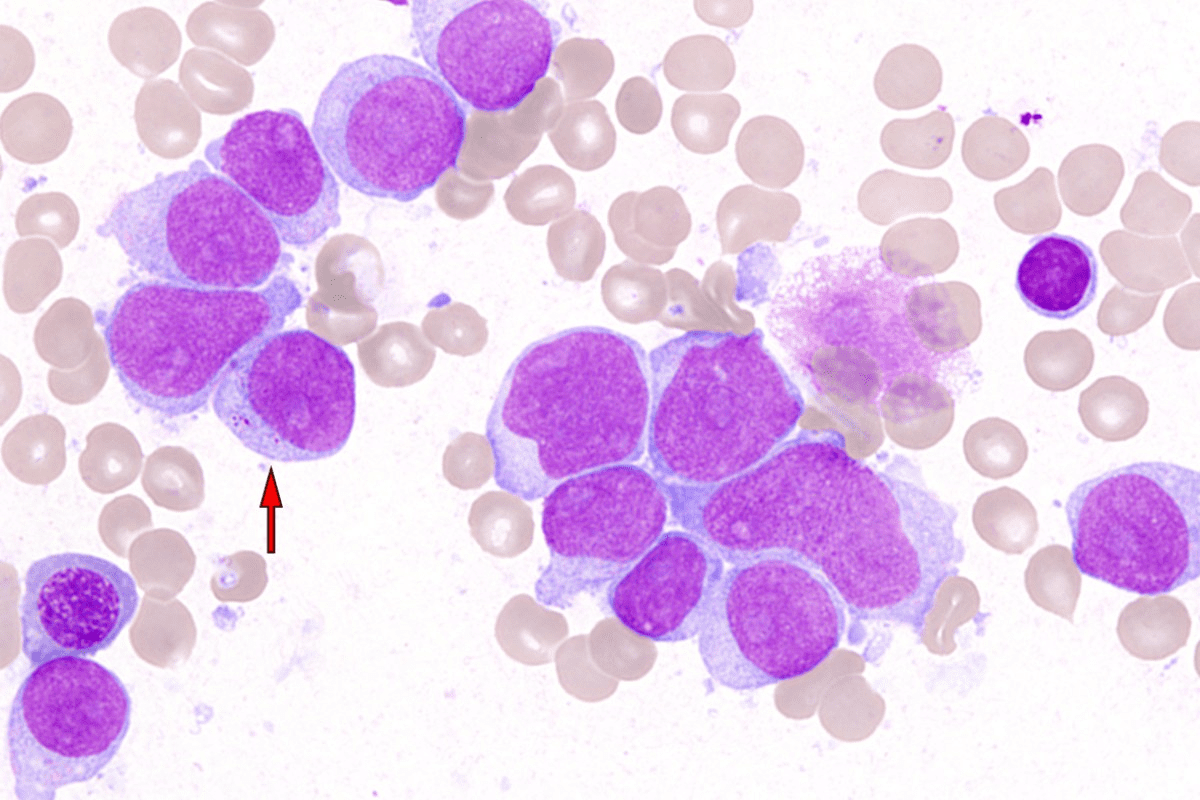
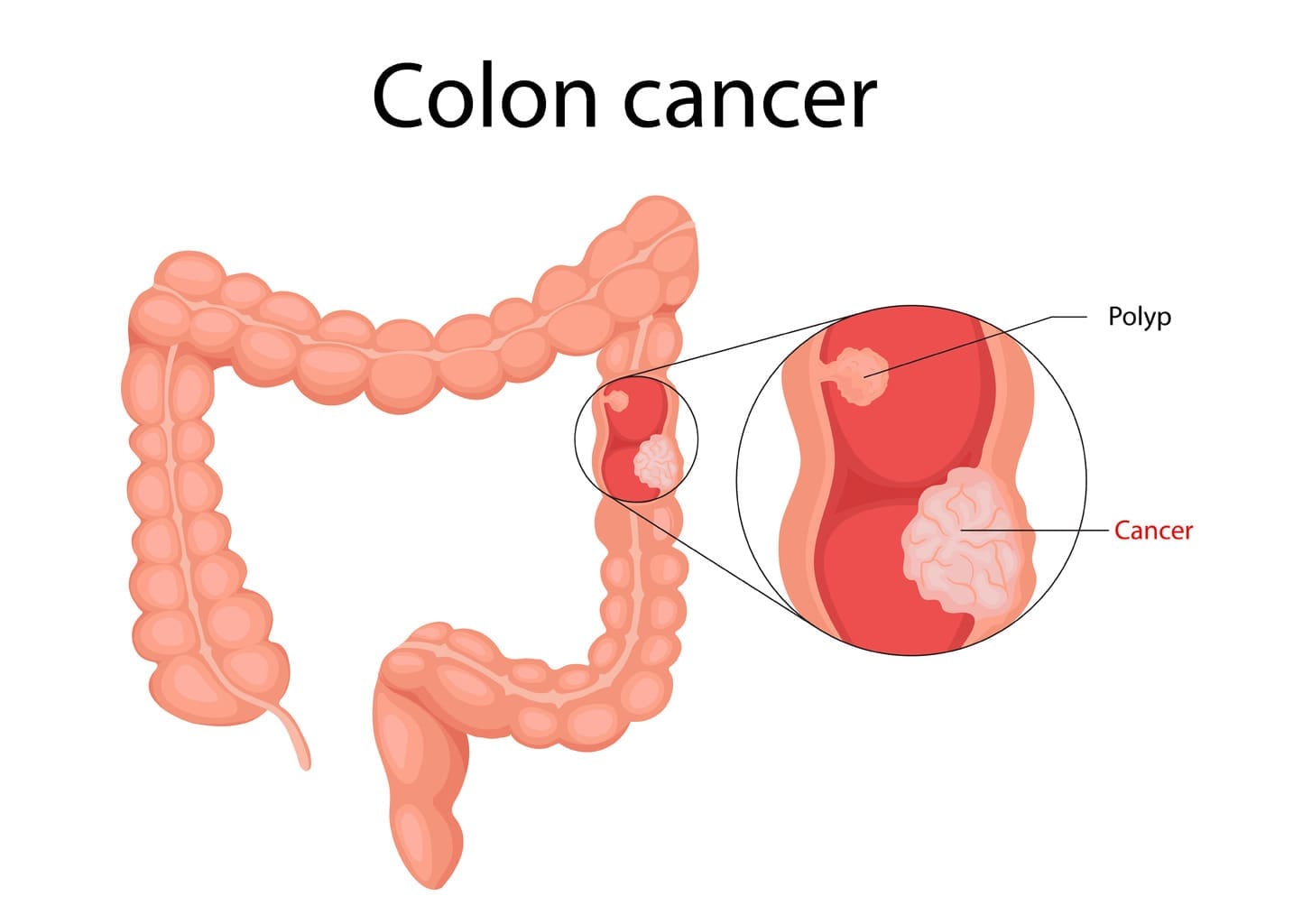
Tumors Near Critical Brain Regions
Tumors near vital brain areas often require awake brain surgery. These tumors can be benign or cancerous. They might affect language, motor functions, or other essential processes.
For example, tumors near areas for speech production and comprehension need careful surgery. Awake craniotomy helps surgeons map these areas. This way, they can remove the tumor without harming the patient’s language skills.
Epilepsy Treatment Considerations
Awake brain surgery is also vital for treating some types of epilepsy. It’s for patients with seizures that start in areas close to critical brain structures. This method helps locate and remove the seizure source without harming other brain areas.
During surgery, patients might do tasks to help the team find the seizure source. This helps in differentiating it from areas needed for normal brain function.
Other Medical Conditions Requiring Awake Neurosurgery
Other conditions like arteriovenous malformations (AVMs) and certain brain lesions also need awake brain surgery. These are located in areas of the brain that are important for various functions.
| Condition | Description | Role of Awake Surgery |
|---|---|---|
| Tumors | Benign or malignant growths near critical brain areas | Precise removal while preserving vital functions |
| Epilepsy | Seizures originating from areas near critical brain structures | Localization and removal of epileptogenic zone |
| AVMs | Abnormal connections between arteries and veins in the brain | Precise treatment to avoid damage to surrounding tissue |
Awake brain surgery is a major step forward in neurosurgery. It offers hope to those with complex brain conditions. Understanding when it’s needed helps us see its importance in treating these conditions effectively.
The Medical Team Behind Awake Craniotomies
Every awake craniotomy success story is thanks to a dedicated team. They all have their own special skills. The awake brain surgery needs a team effort from many experts.
Specialized Roles of Neurosurgeons
Neurosurgeons lead the awake craniotomy team. They remove tumors and treat other brain issues. They also map the brain’s key areas.
During surgery, neurosurgeons ask patients to speak, count, or move. This helps keep important brain functions safe.
Anesthesiologists and Their Critical Function
Anesthesiologists are key in neurosurgery awake patient procedures. They use local anesthesia to numb the scalp. They also give conscious sedation to keep the patient calm.
They must find the right balance. The patient needs to stay awake and alert at times.
Neuropsychologists and Language Specialists
Neuropsychologists and language specialists are vital. They check the patient’s thinking and language skills during surgery. They use tests to see how well the brain is working.
This info helps the neurosurgeon make better decisions. It helps reduce the risks of awake brain surgery.
The success of an awake craniotomy shows the power of teamwork. Neurosurgeons, anesthesiologists, neuropsychologists, and others work together. They make sure patients get the best care, with good results and fewer risks.
Pre-Surgical Preparation and Patient Selection
Not every brain surgery needs the patient to be awake. But for those that do, a detailed pre-surgical plan is key. Awake brain surgery, or awake craniotomy, is a complex procedure. It requires careful planning and patient evaluation for successful outcomes.
Comprehensive Evaluation Process
The pre-surgical evaluation for awake brain surgery is detailed. It involves a team of specialists like neurosurgeons, anesthesiologists, and neuropsychologists. This assessment includes:
- Detailed medical history and physical examination
- Advanced neuroimaging techniques such as MRI and fMRI
- Neurological and neuropsychological assessments
- Cardiovascular evaluation to assess the patient’s overall health
These evaluations help find the best candidates for awake brain surgery. They also let us tailor the procedure to each patient’s needs.
Psychological Preparation for Patients
Preparing patients psychologically for awake brain surgery is as important as the medical evaluation. We give patients detailed information about the procedure. This includes what to expect during surgery and recovery.
Patient education is a critical component of the pre-surgical process. It empowers patients to actively participate in their care and make informed decisions.
Mapping Critical Brain Functions
Mapping critical brain functions is a key part of pre-surgical preparation. This involves identifying areas of the brain responsible for vital functions. Techniques used for brain mapping include:
| Technique | Description | Application in Awake Surgery |
|---|---|---|
| fMRI | Functional MRI that maps brain activity | Pre-surgical planning and intraoperative guidance |
| Direct Cortical Stimulation | Stimulation of the brain’s surface during surgery | Intraoperative mapping of critical brain areas |
| Neuropsychological Testing | Assessment of cognitive functions | Pre-surgical evaluation and intraoperative monitoring |
The integration of these techniques allows for precise localization of critical brain areas. This minimizes the risk of neurological damage during surgery.
By combining a detailed evaluation process, psychological preparation, and advanced brain mapping techniques, we ensure patients are well-prepared for awake brain surgery. This multi-faceted approach is key to achieving the best outcomes in awake brain tumor surgery and other complex neurosurgical procedures.
Step-by-Step: The Awake Brain Surgery Procedure
The awake brain surgery technique is complex. It ensures patient safety and successful outcomes. A skilled medical team and advanced technology are needed.
Initial Anesthesia and Positioning
The process starts with local anesthetics to numb the scalp and skull. This keeps the patient comfortable. Sedation is carefully managed to keep the patient relaxed yet awake.
After the anesthesia takes effect, the patient is placed on the operating table. This position allows the surgical team to easily access the brain area being operated on.
The Awakening Process
As the surgery goes on, the sedation is slowly reduced. This allows the patient to wake up. This step is key because it lets the patient give feedback to the surgical team.
The patient is fully awake and can respond to commands. This helps the surgeons to map critical brain functions and avoid damaging important areas.
Intraoperative Brain Mapping
Brain mapping is a key part of awake brain surgery. Surgeons stimulate different brain areas to identify and preserve vital functions like speech and motor skills.
Advanced technology is used to monitor the brain’s activity in real-time. This ensures the surgical team can make precise adjustments as needed.
Tumor Removal or Treatment Phase
With the brain mapped and critical areas identified, the surgical team removes the tumor or treats the targeted area.
The patient’s feedback is very important during this phase. It helps the surgeons adjust their technique to avoid damage to surrounding brain tissue.
A notable example of awake brain surgery’s success is a Parkinson’s patient who played the clarinet during surgery. They experienced instant symptom relief.
| Step | Description | Key Elements |
|---|---|---|
| Initial Anesthesia | Administration of local anesthetics and sedation | Patient comfort, sedation management |
| Awakening Process | Gradual reduction of sedation to awaken the patient | Real-time patient feedback, responsiveness |
| Intraoperative Brain Mapping | Stimulation of brain areas to identify critical functions | Brain activity monitoring, precision |
| Tumor Removal/Treatment | Removal of tumor or treatment of targeted area | Patient feedback, surgical precision |
Pain Management During Awake Craniotomy
Awake brain surgery might sound scary, but it’s made more comfortable with new pain management methods. Patients worry about pain during the surgery. Our team works hard to keep them comfortable.
Local Anesthesia Techniques
Local anesthesia is key in managing pain during awake craniotomy. Scalp blocks are used to numb the scalp where surgery happens. This method helps block pain at the start of the surgery.
Using local anesthesia lets patients stay awake and alert. This is important for intraoperative brain mapping. It helps surgeons avoid damaging important brain areas.
Conscious Sedation Methods
Conscious sedation is also used to relax patients. It makes them calm without making them sleep. The sedation level can be changed to keep the patient comfortable.
- Common sedatives include propofol and dexmedetomidine.
- Anesthesiologists watch the patient’s vital signs and consciousness level.
- Conscious sedation reduces anxiety and discomfort.
What Patients Actually Feel During Surgery
Patients usually don’t feel much pain during awake craniotomy. The procedure is generally painless because of local anesthesia and conscious sedation. They might feel some pressure or sensations, but these are usually okay.
It’s important for patients to know they’re comfortable during surgery. We use local anesthesia and conscious sedation to keep them comfortable. This way, the surgery can be successful.
Our team is committed to the best care. We answer any questions about pain management during awake craniotomy. Knowing about these methods helps patients feel more at ease.
Patient Experiences: What It’s Like to Be Conscious During Brain Surgery
Patients who have awake brain tumor surgery share many feelings and experiences. This part talks about what they feel, how they talk to the doctors, and the mental side of being awake during surgery.
Common Sensations and Awareness
During awake brain surgery, patients might feel pressure or mild pain. They can be very alert or sometimes sleepy.
Some common feelings include:
- Mild pressure on the skull
- Slight discomfort during the initial incision
- A feeling of being “operated on” without pain
Doctors ask patients to do simple things like speak or move their limbs. This helps the doctors check how the brain is working.
Communication with the Surgical Team
Talking well with the surgical team is very important during awake brain surgery. Patients should tell the team about any feelings or pain they have. This helps the team make the right changes.
| Communication Aspect | Patient’s Role | Surgical Team’s Role |
|---|---|---|
| Pre-Surgical Briefing | Understand the procedure and ask questions | Explain the surgery and address concerns |
| During Surgery | Report sensations, perform tasks as instructed | Monitor brain function, adjust as necessary |
| Post-Surgical Feedback | Provide feedback on the experience | Use feedback for future patient care improvements |
Psychological Aspects of Being Awake
The mind’s impact during awake brain surgery is big. Patients go through a lot of emotional preparation for this.
Important mental aspects include:
- Fear of the unknown
- Anxiety about being awake during surgery
- Trust in the medical team
Knowing these mental factors helps doctors give better care to patients having awake brain surgery.
Technological Innovations in Awake Neurosurgery
Technological advancements have changed awake neurosurgery for the better. They make the procedure safer and more effective. We’re seeing big changes thanks to new neuroimaging and monitoring tools.
Advanced Neuroimaging Techniques
Advanced neuroimaging is key to awake neurosurgery’s success. These tools let surgeons see the brain live, helping them remove tumors safely. This way, they can avoid harming important brain areas.
Some important neuroimaging tools used in awake neurosurgery are:
- Functional MRI (fMRI) to map brain function
- Diffusion Tensor Imaging (DTI) to visualize white matter tracts
- Intraoperative MRI to update the surgical navigation system during the procedure
These technologies have made neurosurgery more accurate. For example, a British woman played the clarinet during her surgery. This showed how advanced neuroimaging helps keep brain functions safe.
| Neuroimaging Technique | Application in Awake Neurosurgery |
|---|---|
| Functional MRI (fMRI) | Mapping brain function to avoid critical areas |
| Diffusion Tensor Imaging (DTI) | Visualizing white matter tracts to preserve neural pathways |
| Intraoperative MRI | Updating surgical navigation during the procedure |
Intraoperative Monitoring Technologies
Intraoperative monitoring is vital for awake neurosurgery’s success. These tools let us watch the patient’s brain function in real-time during surgery.
Key intraoperative monitoring technologies include:
- Electroencephalography (EEG) to monitor brain activity
- Electrocorticography (ECoG) to monitor cortical activity directly
- Neurophysiological monitoring to assess the integrity of neural pathways
Future Directions in Awake Surgery
The future of awake neurosurgery looks bright. Ongoing research and new technologies will make the procedure even safer and more effective. Tools like augmented reality and artificial intelligence will be key in this progress.
We’re always looking to improve our techniques for better patient outcomes. By leading in technology, we ensure our patients get the best treatments available.
Recovery and Post-Operative Considerations
Knowing what to expect after an awake craniotomy can help reduce anxiety and improve recovery. The recovery process includes several important steps. These range from immediate care after surgery to long-term rehabilitation.
Immediate Post-Surgical Experience
After surgery, patients go to the recovery room. There, our medical team closely watches them. This period is key for managing any immediate issues and ensuring comfort.
Patients might feel a range of sensations, from mild discomfort to headaches. These are usually managed with the right care. We aim to make this transition as smooth as possible, using pain management strategies tailored to each patient.
Managing Post-Operative Pain
Managing pain well is essential after surgery. We use a mix of medications and other methods to keep patients comfortable. Our goal is to reduce pain without overmedicating.
Post-Operative Pain Management Strategies:
- Medication: A mix of painkillers tailored to each patient.
- Monitoring: We constantly check pain levels to adjust treatment as needed.
- Patient Education: We teach patients about pain management at home.
Long-Term Follow-Up and Rehabilitation
The recovery journey goes beyond the immediate post-surgery period. It includes long-term follow-up and rehabilitation. Our team helps develop a rehabilitation plan that meets each patient’s needs.
| Rehabilitation Aspect | Description | Timeline |
|---|---|---|
| Physical Therapy | To regain strength and mobility | Typically starts within weeks after surgery |
| Speech Therapy | To address any speech or language difficulties | May start during hospital stay or shortly after discharge |
| Follow-Up Appointments | To monitor recovery and address any concerns | Scheduled regularly for several months post-surgery |
Understanding the recovery process helps patients prepare for what’s ahead. Our team is dedicated to providing full care and support. We aim to ensure the best outcomes for our patients.
Conclusion: The Future of Awake Brain Surgery
Awake brain surgery is a big step forward in neurosurgery. It brings many benefits to patients with complex operations. As we move forward, we expect even more progress in this area.
Technological breakthroughs and a better understanding of the brain will drive these advancements. This means better outcomes for patients in the future.
We’re dedicated to top-notch healthcare for everyone, including international patients. By embracing new techniques in awake brain surgery, we aim to keep improving care. This will make a big difference in people’s lives all over the world.
FAQ
What is awake brain surgery?
Awake brain surgery, also known as awake craniotomy, is a type of surgery. The patient stays awake during part of it. This lets surgeons watch brain functions live, making the surgery safer and more effective.
Is awake brain surgery painful?
No, awake brain surgery isn’t painful. This is because local anesthetics numb the scalp and skull. Also, sedation is managed carefully to keep the patient comfortable.
Why is awake brain surgery necessary?
It’s key for tumors or areas causing seizures near important brain parts. Surgeons can watch these areas closely. This helps avoid damage during surgery.
Who is a candidate for awake brain surgery?
Not all surgeries need the patient to be awake. Doctors carefully check if someone is right for awake brain surgery. They look at the brain’s functions and prepare the patient mentally.
What is the role of the medical team during awake brain surgery?
A team of experts is vital for awake craniotomy success. This team includes neurosurgeons, anesthesiologists, and specialists in brain functions. Each plays a key role to make the surgery safe and effective.
How is pain managed during awake brain surgery?
Pain control uses local anesthesia and sedation. This keeps patients comfortable during the surgery.
What can patients expect during the recovery process?
Some patients might have headaches after surgery, but they’re usually manageable. A detailed follow-up and rehabilitation plan helps with recovery.
What are the benefits of awake brain surgery?
It has many benefits. It lets surgeons watch brain functions live, reducing damage risks. It can also lead to better outcomes for complex brain conditions.
Are there any risks associated with awake brain surgery?
Like any surgery, awake brain surgery has risks. But, these are lowered by the skill of the medical team and careful patient selection.
How is the future of awake brain surgery evolving?
Awake neurosurgery is getting better thanks to new tech. Advances in imaging and monitoring help make the surgery safer and more effective.