At Liv Hospital, we recognize the vital role of interventional radiology plays in modern healthcare. This specialized field of medicine employs advanced imaging methods to perform minimally invasive treatments, revolutionizing patient care. What is IR radiology? Discover 7 essential and powerful interventional radiology procedures in our simple, expert guide.
We utilize interventional radiology procedures to diagnose and treat a range of medical conditions, reducing the need for surgical interventions. Our team of skilled interventional radiologists works closely with patients to provide personalized care and support throughout the treatment process.
By leveraging the latest advancements in interventional radiology, we can offer patients effective, minimally invasive treatment options that promote faster recovery times and improved outcomes.
Key Takeaways
- Interventional radiology is a specialized field that uses advanced imaging for minimally invasive treatments.
- Liv Hospital offers expert interventional radiology services with a patient-centered approach.
- Interventional radiologists play a crucial role in diagnosing and treating various medical conditions.
- Minimally invasive treatments reduce the need for surgical interventions and promote faster recovery.
- Advanced interventional radiology procedures improve patient outcomes and quality of life.
The Growing Field of IR Radiology: An Overview
Interventional radiology (IR) has emerged as a crucial component of modern medicine. We are witnessing a significant shift in how medical procedures are performed, thanks to the advancements in IR radiology. This field combines imaging technologies with minimally invasive procedures to diagnose and treat various medical conditions.
What Is Interventional Radiology?
Interventional radiology involves using real-time imaging guidance to perform procedures that were once considered highly invasive. IR procedures utilize imaging technologies such as X-ray, ultrasound, CT scans, and MRI to guide instruments through the body. This approach allows for precise treatment with minimal damage to surrounding tissues.
The use of advanced imaging in IR radiology enables us to visualize the procedure in real-time, ensuring accuracy and safety. This is particularly beneficial for patients who may not be good candidates for traditional surgery due to age or health conditions.
Minimally Invasive Approach to Treatment
One of the key benefits of IR radiology is its minimally invasive nature. Procedures are performed through small incisions, reducing recovery time and the risk of complications. This approach not only improves patient outcomes but also enhances their overall experience.
| Benefits | Traditional Surgery | IR Radiology |
| Recovery Time | Longer | Shorter |
| Risk of Complications | Higher | Lower |
| Pain and Discomfort | More | Less |
By leveraging the latest advancements in imaging and instrumentation, IR radiology is revolutionizing the way we approach medical treatment. As technology continues to evolve, we can expect IR radiology to play an increasingly important role in patient care.
Who Performs These Procedures: The Interventional Radiology Doctor
Interventional radiology doctors play a vital role in diagnosing and treating various medical conditions using minimally invasive techniques. These medical specialists have undergone extensive training in both diagnostic imaging and interventional procedures, making them crucial in the healthcare team.
The role of an interventional radiologist is multifaceted, requiring a deep understanding of imaging technologies and clinical practices. Their expertise enables them to perform a wide range of procedures, from vascular interventions to biopsies, with precision and care.
Training and Expertise Required
To become an interventional radiologist, one must undergo rigorous training. This includes completing medical school, followed by a residency program in radiology, and often additional fellowship training in interventional radiology. This extensive education equips them with the necessary skills to operate complex imaging equipment and perform intricate procedures.
Their training also emphasizes the importance of patient care and safety, ensuring that they can manage potential complications and provide comprehensive care to their patients.
The Multidisciplinary Role of an Interventional Radiologist
Interventional radiologists work closely with other healthcare professionals to provide integrated care. They collaborate with surgeons, oncologists, and other specialists to develop treatment plans that are tailored to the individual needs of each patient.
This multidisciplinary approach ensures that patients receive the most appropriate and effective treatment, leveraging the strengths of various medical specialties to achieve the best possible outcomes.
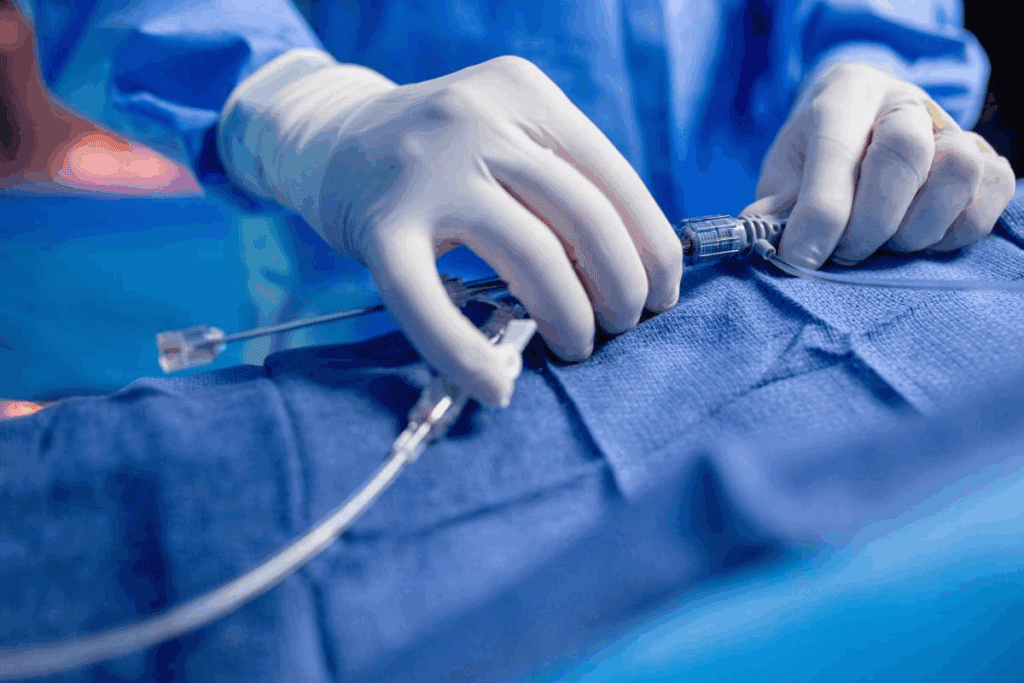
Essential Procedure #1: Angioplasty and Stent Placement
The combination of angioplasty and stent placement is a powerful tool in interventional radiology, offering a minimally invasive solution for vascular conditions. We utilize these procedures to restore blood flow in patients with narrowed or blocked arteries, significantly improving their quality of life.
How Angioplasty Restores Blood Flow
Angioplasty involves the use of a balloon to open narrowed or blocked blood vessels. During the procedure, a catheter is guided to the site of the blockage, and the balloon is inflated to restore normal blood flow. This minimally invasive technique is highly effective in treating conditions such as peripheral artery disease.
The benefits of angioplasty include reduced recovery time and less risk compared to traditional surgical methods. It’s a procedure that we perform with precision, ensuring that patients experience minimal discomfort and can quickly return to their daily activities.
Types of Stents and Their Applications
Following angioplasty, a stent is often placed to keep the artery open. There are different types of stents, including bare-metal stents and drug-eluting stents. Drug-eluting stents are particularly effective in reducing the risk of the artery re-narrowing by releasing medication that prevents cell proliferation.
The choice of stent depends on various factors, including the patient’s condition, the location of the blockage, and the size of the artery. We carefully evaluate these factors to determine the most appropriate stent for each patient.
Patient Recovery and Outcomes
Recovery from angioplasty and stent placement is generally quick, with most patients able to resume normal activities within a few days. We monitor patients closely after the procedure to ensure that they are recovering as expected and to address any concerns they may have.
The outcomes of these procedures are typically very positive, with significant improvements in blood flow and a reduction in symptoms related to vascular disease. By restoring normal blood flow, we help patients avoid more invasive surgical procedures and improve their overall health.
Essential Procedure #2: Embolization Techniques
Embolization, a key component of interventional radiology, involves blocking blood flow to specific areas, treating conditions like fibroids and tumors. This technique has become a cornerstone in modern medicine, offering minimally invasive alternatives to traditional surgical methods.
Uterine Fibroid Embolization (UFE)
Uterine Fibroid Embolization is a procedure that blocks the blood supply to fibroids, leading to their shrinkage. Performed under local anesthesia, UFE is an attractive option for women seeking to avoid hysterectomy. The procedure involves navigating a catheter to the uterine arteries and injecting embolic material to block the blood flow.
Tumor Embolization for Cancer Treatment
Tumor embolization is used to treat various types of cancers by cutting off the tumor’s blood supply. This can be particularly useful for tumors that are difficult to remove surgically or have a rich blood supply. The procedure can reduce tumor size, alleviate symptoms, and improve the patient’s quality of life.
Emergency Embolization for Trauma and Bleeding
In cases of severe trauma or life-threatening bleeding, emergency embolization can be a lifesaver. By quickly identifying and blocking the bleeding vessel, interventional radiologists can stabilize the patient and prevent further complications.
| Embolization Technique | Application | Benefits |
| Uterine Fibroid Embolization | Treatment of uterine fibroids | Minimally invasive, avoids surgery |
| Tumor Embolization | Cancer treatment | Reduces tumor size, alleviates symptoms |
| Emergency Embolization | Trauma and life-threatening bleeding | Lifesaving, rapid control of bleeding |
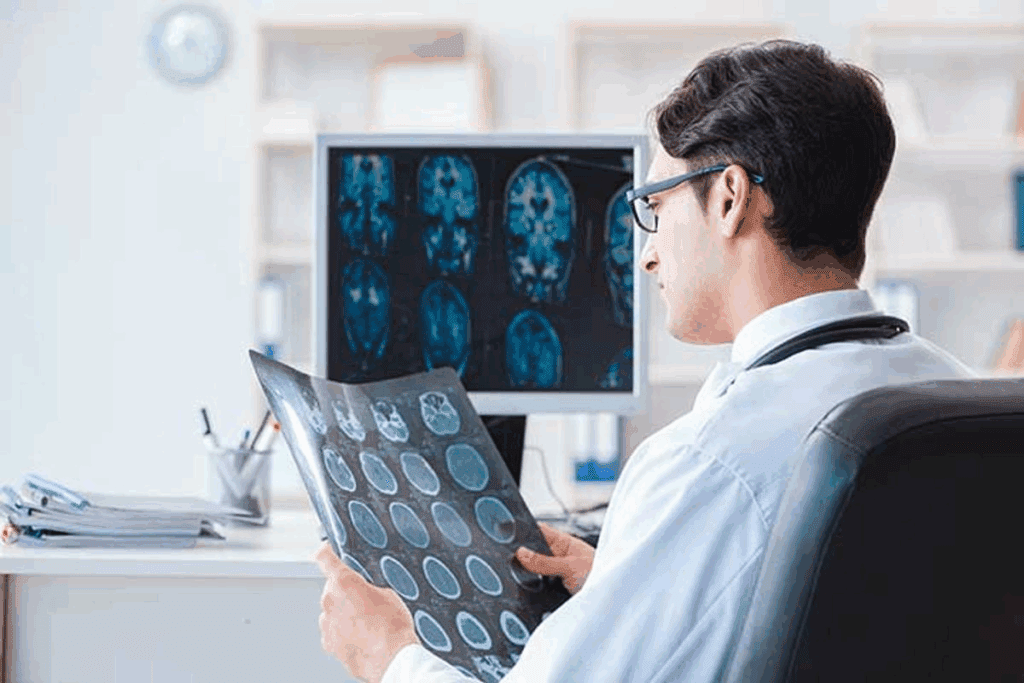
Essential Procedure #3: Image-Guided Biopsies
Image-guided biopsies have revolutionized the field of diagnostics by allowing for precise tissue sampling. We utilize advanced imaging technologies to guide the biopsy needle, ensuring accurate targeting of the tissue or organ of interest.
Types of IR-Guided Tissue Sampling
There are several types of tissue sampling techniques used in image-guided biopsies, including fine-needle aspiration, core needle biopsy, and vacuum-assisted biopsy. Each method has its specific indications and advantages, depending on the nature of the lesion and the required tissue sample.
| Biopsy Type | Indications | Advantages |
| Fine-needle aspiration | Cystic lesions, lymph nodes | Minimally invasive, quick recovery |
| Core needle biopsy | Solid tumors, suspicious masses | Provides tissue architecture, higher diagnostic yield |
| Vacuum-assisted biopsy | Breast lesions, large tissue samples | More tissue obtained, better for histological analysis |
The Procedure Process
The image-guided biopsy procedure involves several steps. First, we use imaging modalities such as ultrasound, CT, or MRI to locate the target area. Then, we administer local anesthesia to minimize discomfort. Using real-time imaging guidance, we advance the biopsy needle to the target site and obtain the tissue sample.
Advantages Over Surgical Biopsies
Image-guided biopsies offer several advantages over traditional surgical biopsies. They are minimally invasive, resulting in less tissue trauma and scarring. The recovery time is also significantly reduced, allowing patients to return to their normal activities sooner. Moreover, image-guided biopsies can be performed on an outpatient basis, reducing the need for hospitalization.
Overall, image-guided biopsies represent a significant advancement in diagnostic medicine, providing accurate tissue sampling with minimal risk and discomfort to the patient.
Essential Procedure #4: IV Radiology and Vascular Access
IV radiology plays a crucial role in vascular access, enabling healthcare providers to deliver various treatments effectively. Vascular access is a critical component of many medical treatments, including chemotherapy, dialysis, and nutritional support. IV radiology has transformed the way vascular access is achieved, making procedures safer and more efficient.
PICC Lines and Central Venous Catheters
PICC (Peripherally Inserted Central Catheter) lines and central venous catheters are essential for long-term vascular access. These catheters are used for administering medications, fluids, and nutrients directly into the bloodstream. IV radiology ensures precise placement of these catheters, reducing the risk of complications.
Port Placement for Chemotherapy
Port placement is a common procedure for patients undergoing chemotherapy. A port is a small device implanted under the skin, allowing easy access to a vein for chemotherapy administration. IV radiology guides the placement of these ports, ensuring accurate positioning and minimizing the risk of infection or other complications.
Dialysis Access Management
For patients requiring dialysis, IV radiology plays a vital role in managing dialysis access. This includes creating or maintaining arteriovenous fistulas or grafts, which are used for dialysis. IV radiology techniques help in diagnosing and treating issues related to dialysis access, ensuring that patients receive uninterrupted dialysis treatment.
In conclusion, IV radiology is indispensable in vascular access procedures, offering precise and safe methods for PICC lines, port placement, and dialysis access management. These procedures significantly improve patient outcomes by reducing complications and enhancing the effectiveness of treatments.
Essential Procedure #5: Vertebral Augmentation
We utilize vertebral augmentation to stabilize fractured vertebrae, significantly improving patient outcomes in terms of pain and mobility. Vertebral augmentation encompasses procedures like vertebroplasty and kyphoplasty, which are designed to treat vertebral compression fractures.
These fractures can result from osteoporosis, cancer, or other conditions that weaken bone structure, leading to severe back pain and reduced mobility. Vertebral augmentation offers a minimally invasive solution, providing immediate stability and pain relief.
Vertebroplasty Technique
Vertebroplasty involves injecting bone cement into the fractured vertebra to stabilize it. This procedure is performed under imaging guidance, ensuring precise placement of the cement. The goal is to restore vertebral strength, reduce pain, and improve the patient’s quality of life.
The technique is relatively quick, often taking less than an hour, and can be performed under local anesthesia or conscious sedation. Patients typically experience significant pain relief within a few days.
Kyphoplasty for Vertebral Compression Fractures
Kyphoplasty is a variation of vertebral augmentation that involves creating a cavity within the fractured vertebra before injecting bone cement. This is achieved using a balloon that is inflated to restore some of the vertebral height.
- Kyphoplasty can help restore vertebral body height.
- It reduces kyphotic deformity.
- It provides stabilization and pain relief.
By restoring vertebral height, kyphoplasty can improve spinal alignment and reduce the risk of further deformity.
Patient Selection and Outcomes
Patient selection is critical for the success of vertebral augmentation procedures. Ideal candidates are those with painful vertebral compression fractures that have not responded to conservative management.
Outcomes are generally favorable, with most patients experiencing significant pain reduction and improved mobility. However, as with any medical procedure, there are risks and potential complications, such as cement leakage or infection.
By carefully selecting patients and utilizing advanced imaging techniques, we can minimize risks and optimize outcomes. Vertebral augmentation has become a valuable tool in managing vertebral compression fractures, enhancing the quality of life for many patients.
Essential Procedure #6: Drainage Procedures
The realm of interventional radiology includes several drainage procedures that have revolutionized the treatment of infections and obstructions. Drainage procedures involve the removal of fluid collections, abscesses, or obstructions, significantly improving patient outcomes. These interventions are crucial in managing various medical conditions, offering minimally invasive solutions that reduce recovery time and complications.
Abscess Drainage Techniques
Abscess drainage is a critical procedure in interventional radiology, aimed at treating abscesses that are not responsive to antibiotic therapy. Using imaging guidance, a catheter is placed within the abscess to drain the infected fluid. This technique not only alleviates symptoms but also promotes healing by reducing the bacterial load.
Key Steps in Abscess Drainage:
- Imaging-guided needle placement
- Catheter insertion for drainage
- Monitoring and follow-up to ensure resolution
Biliary and Nephrostomy Tube Placement
Biliary drainage and nephrostomy tube placement are vital procedures for managing obstructions in the biliary and urinary systems, respectively. Biliary drainage is often used to relieve jaundice and prevent cholangitis in patients with bile duct obstruction. Similarly, nephrostomy tube placement is employed to decompress the urinary system in cases of obstruction, thereby preserving renal function.
| Procedure | Indications | Benefits |
| Biliary Drainage | Bile duct obstruction, cholangitis | Relieves jaundice, prevents infection |
| Nephrostomy Tube Placement | Urinary tract obstruction, hydronephrosis | Decompresses urinary system, preserves renal function |
Post-Procedure Care
Post-procedure care is essential for the success of drainage procedures. Patients are monitored for signs of infection or complications, and the drainage catheters are managed to ensure continued drainage. Follow-up imaging studies are performed to assess the resolution of the treated condition and to plan for catheter removal when appropriate.
By understanding the various drainage procedures and their applications, healthcare providers can offer optimal care for patients requiring these interventions. As interventional radiology continues to evolve, these procedures remain crucial in the management of complex medical conditions.
Essential Procedure #7: Thermal Ablation Therapies
The application of thermal ablation in medical treatments signifies a significant advancement in patient care, minimizing recovery times and maximizing outcomes. Thermal ablation involves the use of extreme temperatures, either heat or cold, to destroy abnormal or diseased tissue. This technique has gained prominence in treating various cancers and other conditions, offering a minimally invasive alternative to traditional surgical methods.
Radiofrequency Ablation (RFA)
Radiofrequency ablation is a widely used thermal ablation technique that employs electrical energy to heat targeted tissues. RFA is particularly effective in treating tumors in the liver, kidney, and bone. The procedure involves inserting a specialized needle electrode into the tumor under imaging guidance. Once in place, the electrode emits radiofrequency waves that generate heat, destroying the tumor cells.
The benefits of RFA include its minimally invasive nature, reduced risk of complications, and the ability to treat patients who may not be good candidates for surgery. RFA can be performed on an outpatient basis, allowing patients to return home the same day.
Microwave and Cryoablation Techniques
In addition to RFA, other thermal ablation techniques include microwave ablation and cryoablation. Microwave ablation uses microwave energy to heat and destroy cancer cells, offering a faster and more efficient treatment option for larger tumors. Cryoablation, on the other hand, involves freezing the targeted tissue using extremely cold temperatures, leading to cell death.
- Microwave ablation is advantageous for its ability to achieve higher temperatures more quickly than RFA.
- Cryoablation is beneficial for its precision in treating tumors near sensitive structures.
Applications in Oncology
Thermal ablation therapies have become a valuable tool in oncology, providing effective treatment options for various types of cancer. These techniques can be used alone or in combination with other treatments, such as chemotherapy or surgery, to achieve optimal outcomes. The precision and minimally invasive nature of thermal ablation make it an attractive option for patients seeking to minimize recovery time and maximize quality of life.
As we continue to advance in the field of interventional radiology, thermal ablation therapies are likely to play an increasingly important role in cancer treatment, offering new hope and improved outcomes for patients worldwide.
Conclusion: The Future of Interventional Radiology
As we have explored the various essential interventional radiology procedures, it is clear that this field is revolutionizing the way we approach medical treatment. Interventional radiology continues to evolve, offering innovative, minimally invasive solutions for a range of medical conditions.
The future of IR is bright, with advancements in technology and technique expanding its applications. We anticipate that interventional radiology will play an increasingly important role in international radiology, providing effective treatments for complex conditions and improving patient outcomes.
By embracing the latest developments in intervention radiology, healthcare providers can offer patients more options and better care. As the field continues to grow, we look forward to the new possibilities that will emerge, further enhancing the role of interventional radiology in modern medicine.
FAQ
What is interventional radiology?
Interventional radiology (IR) is a medical specialty that uses minimally invasive image-guided procedures to diagnose and treat various diseases. We utilize advanced imaging technologies like X-ray, ultrasound, and MRI to perform procedures that were previously done through open surgery.
What kind of training does an interventional radiologist have?
Interventional radiologists undergo extensive training, including medical school, a radiology residency, and often additional fellowship training in interventional radiology. This comprehensive education equips them with the expertise to perform complex procedures and provide high-quality patient care.
What is the role of an interventional radiologist in patient care?
Interventional radiologists play a multidisciplinary role, collaborating with other healthcare professionals to provide comprehensive care. We work closely with referring physicians to determine the best treatment options for patients and often serve as primary caregivers for patients undergoing IR procedures.
What is angioplasty and stent placement?
Angioplasty is a procedure that uses a balloon to widen narrowed or blocked blood vessels. Stent placement involves deploying a small, mesh-like device to keep the vessel open. We often combine these procedures to restore blood flow to critical areas of the body.
What are the benefits of embolization techniques?
Embolization techniques, such as uterine fibroid embolization (UFE) and tumor embolization, offer several benefits, including reduced symptoms, minimized bleeding, and improved quality of life. These procedures can be effective alternatives to surgery for certain conditions.
What is an image-guided biopsy?
An image-guided biopsy is a procedure that uses imaging technologies like ultrasound, CT, or MRI to guide the collection of tissue samples. This minimally invasive approach reduces the risk of complications and allows for more accurate diagnoses.
What is the role of IV radiology in vascular access?
IV radiology plays a crucial role in vascular access procedures, such as PICC line placement, port placement, and dialysis access management. We use imaging guidance to ensure safe and effective placement of these devices, which are essential for patient care.
What are vertebroplasty and kyphoplasty?
Vertebroplasty and kyphoplasty are minimally invasive procedures used to treat vertebral compression fractures. We inject bone cement into the affected vertebra to stabilize and strengthen it, reducing pain and improving mobility.
What are drainage procedures used for?
Drainage procedures, such as abscess drainage and biliary drainage, are used to manage infections and obstructions. We use imaging guidance to place drainage catheters, which help to remove infected fluid or debris and promote healing.
What is thermal ablation therapy?
Thermal ablation therapy involves using heat or cold to destroy cancer cells or damaged tissue. Techniques like radiofrequency ablation (RFA), microwave ablation, and cryoablation offer minimally invasive alternatives to surgery for certain conditions.
What are the benefits of interventional radiology procedures?
Interventional radiology procedures offer several benefits, including reduced recovery time, less pain, and lower risk of complications compared to traditional surgery. We strive to provide high-quality, patient-centered care that improves outcomes and enhances quality of life.
Are interventional radiology procedures safe?
Interventional radiology procedures are generally safe when performed by experienced professionals in a suitable environment. We take necessary precautions to minimize risks and ensure optimal outcomes for our patients.
References:
- Mukund, A., et al. (2018). Basic Interventional Procedures: Practice Essentials. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC6639855/