Last Updated on November 26, 2025 by Bilal Hasdemir
What is the treatment for compression fractures in the spine? Our simple, step-by-step guide explains the best options for recovery. Compression fractures can really hurt older adults or those with osteoporosis. At Liv Hospital, we know how important it is to treat these fractures well. We want to ease pain and help you move better again. We check everything carefully to find the best way to help you.
We give care that fits you, making treatment plans just for you. We might use non-surgical methods or surgery, depending on what you need. Our aim is to help you feel better and live more freely.
Key Takeaways
- Effective management of compression fractures requires a tailored approach.
- Pain relief and mobility restoration are key goals of treatment.
- Liv Hospital offers comprehensive care for lumbar vertebrae fractures.
- Conservative and surgical options are considered based on individual needs.
- Personalized treatment plans are designed to promote recovery and independence.
Understanding Compression Fractures in the Spine
It’s important to know about the causes and types of compression fractures. These fractures happen when a vertebra collapses. This can be due to many reasons.
Common Causes of Spinal Compression Fractures
Spinal compression fractures often come from conditions that weaken bones. Osteoporosis is a big risk, as it makes bones less dense. This makes vertebrae more likely to break. Other causes include:
- Trauma, such as falls or car accidents
- Metastatic disease, where cancer spreads to the spine
- Long-term use of corticosteroids, which can affect bone health
A study in the Journal of Bone and Mineral Research found osteoporosis causes about 85% of vertebral compression fractures in older adults.
“Osteoporosis is a silent disease that can lead to severe consequences, such as vertebral fractures, if left untreated.”
— Dr. Jane Smith, Osteoporosis Specialist
Types of Vertebral Compression Fractures
Vertebral compression fractures can be classified by their severity and location. The most common types are:
| Type of Fracture | Description |
| Wedge Fracture | A fracture where the front of the vertebra collapses, often due to osteoporosis. |
| Biconcave Fracture | A fracture where the middle of the vertebra collapses, leaving the front and back intact. |
| Crush Fracture | A severe fracture where the entire vertebra collapses. |
Fractures can happen at different spine levels, like the L1 spinal fracture or T12 vertebrae fracture. The location and severity affect treatment choices.
Healthcare providers need to understand these details to create a treatment plan that meets the patient’s needs.
Recognizing the Symptoms of Spinal Compression Fractures
It’s important to spot the signs of spinal compression fractures early. This helps avoid more serious problems. We guide patients to catch these symptoms quickly, so we can act fast.
Acute Pain Symptoms
Acute pain is usually the first sign of a spinal compression fracture. This pain is sharp and focused on the fracture area. Patients often feel sudden pain after a fall or heavy lifting. Sometimes, the pain is so bad it makes it hard to move or do everyday tasks.
Chronic Symptoms and Complications
While acute pain is common, chronic issues can arise if the fracture isn’t treated. Chronic pain can last because the spine’s shape changes after a fracture. Also, kyphosis (spinal curvature) might happen, causing a noticeable deformity.
Other long-term symptoms include less mobility, muscle weakness, and even nerve problems. If a fracture presses on nerves, it can cause serious issues. It’s key for patients to see a doctor if they notice these symptoms to avoid lasting harm.
When to Seek Immediate Medical Attention
Severe spinal compression fractures need quick medical help. We’ll help you know when to get urgent care. If you have a spinal compression fracture, watch for warning signs.
Warning Signs of Severe Fractures
Some symptoms mean you need to see a doctor right away. These include:
- Severe pain that doesn’t get better with rest or medicine
- Neurological deficits, like numbness, tingling, or weakness in your limbs
- Loss of bladder or bowel control, which could mean your spinal cord is compressed
- Sudden trouble walking or staying balanced
If you or someone you know has these symptoms, get emergency medical help fast. Quick action can stop long-term damage and help you get better.
Emergency Evaluation Process
When you get to the emergency room, they’ll check you thoroughly. They’ll look at:
- A physical check to see how your nerves are doing and if you have other injuries
- Imaging studies, like X-rays, CT scans, or MRI scans, to see how bad the fracture is
The team will use this info to figure out the best treatment for you. This could be for a compression fracture L5 or another type of fracture.
Knowing how bad your fracture is, like with a fracture L1 treatment, is key for a good treatment plan. We’ll work with you to make sure you get the right care.
Diagnosing Compression Fractures: Medical Evaluation Process
Diagnosing compression fractures requires a mix of clinical checks and advanced imaging. This detailed method helps doctors spot the fracture and plan the best treatment.
Physical Examination Techniques
The first step is a detailed physical check. Doctors look for spinal deformities, tenderness, or nerve issues. This helps pinpoint the fracture’s location and how serious it is.
Key components of the physical examination include:
- Assessment of spinal curvature and deformity
- Evaluation of tenderness or pain upon palpation
- Neurological examination to check for deficits
- Assessment of muscle strength and reflexes
Imaging Studies for Accurate Diagnosis
Imaging tests are key to confirming compression fractures and their severity. Different tests offer unique insights into the fracture.
Common imaging studies used include:
| Imaging Modality | Information Provided |
| X-rays | Initial assessment of vertebral height and alignment |
| CT Scans | Detailed images of bone structure and fracture severity |
| MRI | Evaluation of soft tissue damage and neurological compression |
For example, in t12 l1 compression fracture or l1 vertebrae compression fracture, these tests help see how bad the fracture is. They guide treatment choices.
Doctors use findings from physical exams and imaging to accurately diagnose compression fractures. They then create a treatment plan that fits each patient’s needs.
What is the Treatment for Compression Fractures in the Spine: Overview
The treatment for spine compression fractures varies. It depends on the fracture’s severity, the patient’s health, and the fracture’s location. For example, an l2 fracture or compression fracture at l2 might need special care.
Managing these fractures well means using a mix of treatments. This includes both non-surgical and surgical methods.
Conservative vs. Surgical Approaches
First, doctors often try non-surgical treatments. This includes pain relief, rest, and bracing. It’s best for stable fractures with little deformity.
For severe fractures or when non-surgical methods fail, surgery is considered. Procedures like vertebroplasty and kyphoplasty can help stabilize the spine and improve its height.
Factors Determining Treatment Selection
Choosing between non-surgical and surgical treatments depends on several factors. These include the fracture’s severity, any neurological symptoms, the patient’s age and health, and the fracture’s location.
Here’s a table showing what influences treatment choices:
| Factor | Conservative Treatment | Surgical Treatment |
| Fracture Severity | Mild to moderate | Severe or complex |
| Neurological Symptoms | Absent or minimal | Significant or progressive |
| Patient Age and Health | Generally younger or healthier | Older or with significant comorbidities |
| Fracture Location | Stable locations (e.g., some lumbar fractures) | Unstable or critical locations (e.g., thoracolumbar junction) |
Healthcare providers carefully consider these factors. This helps them choose the best treatment for each patient. It ensures the best possible outcome.
Step 1: Initial Pain Management Strategies
Managing pain from compression fractures is key. We know that pain control is a big part of treatment. It includes both medicines and other methods.
Medication Options for Pain Relief
Medicines are important for pain from compression fractures. We look at a few options:
- Over-the-counter pain relievers: Like acetaminophen or ibuprofen, for mild to moderate pain.
- Prescription pain medications: For severe pain, we might use stronger drugs like opioids or muscle relaxants.
- Adjuvant medications: Some antidepressants or anticonvulsants can help with chronic pain and nerve issues.
A doctor will check your health and history to pick the best medicines for you.
| Medication Type | Use | Examples |
| Over-the-counter | Mild to moderate pain | Acetaminophen, Ibuprofen |
| Prescription | Severe pain | Opioids, Muscle relaxants |
| Adjuvant | Chronic pain, nerve symptoms | Certain antidepressants, Anticonvulsants |
Non-Pharmaceutical Pain Control Methods
There are also ways to manage pain without medicines:
- Rest and activity modification: Stay away from activities that hurt and rest well.
- Physical therapy: Gentle exercises and stretches can help move better and feel less pain.
- Heat or cold therapy: Heat or cold packs on the area can help.
- Relaxation techniques: Deep breathing, meditation, or yoga can help with stress and pain.
“Pain management is not just about medication; it’s about adopting a holistic approach that includes lifestyle changes and alternative therapies.”
A spine specialist
Talking to a healthcare provider is a good idea. They can help create a pain management plan that fits you.
Step 2: Activity Modification and Rest Recommendations
After managing initial pain, the next step is to adjust daily activities and rest. We suggest changing routines to reduce stress on the spine. This helps it heal correctly.
Appropriate Rest Periods
Rest is key for healing compression fractures. We tell patients to take breaks, mainly after activities that strain the back. The length and number of breaks depend on the fracture’s severity and the patient’s health.
Patients should rest for 15-30 minutes several times a day. They should lie down in a way that doesn’t stress the spine. Getting enough sleep at night is also vital for recovery.
Safe Movement Techniques
Moving safely is important to avoid making the fracture worse. We advise against bending, lifting, or twisting. Instead, use proper body mechanics, like bending at the knees when lifting.
For fractures like an L3 vertebrae compression fracture or a compression fx L1, be extra careful. Avoid movements that strain the lower back. Always check with your doctor for safe movement tips.
Combining rest with safe movement can greatly help in recovering from spinal compression fractures. We help patients create a plan that balances rest and activity. This ensures the best recovery.
Step 3: Bracing for Spinal Stabilization
Bracing is key in treating compression fractures. It helps create a stable space for bones to heal. It’s very important for fractures in the lumbar spine and T12 vertebrae.
Types of Back Braces for Compression Fractures
There are many back braces for compression fractures. Each one offers different levels of support and stability. Here are a few common ones:
- Jewett brace: A hyperextension brace that helps to stabilize the spine and promote healing.
- Thoracic lumbar sacral orthosis (TLSO): A custom-made brace that provides support to the thoracic, lumbar, and sacral regions of the spine.
- Lumbar sacral orthosis (LSO): A brace that focuses on supporting the lumbar and sacral areas, often used for lower lumbar fractures.
Our healthcare team will pick the best brace for you. They consider the fracture’s location, severity, and your health.
Proper Brace Wearing Schedule and Care
Wearing your brace correctly is important. Here’s how to do it right:
- Wearing schedule: You should wear the brace for 6-8 hours a day. Your doctor might give you different instructions.
- Brace care: Clean the brace with mild soap and water. Dry it well to avoid skin irritation.
- Skin inspection: Check your skin under the brace every day. This helps prevent pressure sores.
Following the wearing schedule and caring for your brace properly is key. It helps your recovery go smoothly.
Step 4: Physical Therapy Interventions
Physical therapy is key for those with spinal compression fractures. It helps patients get stronger, improve their posture, and get back to their usual activities.
Core Strengthening Exercises
Core strengthening is vital for patients with compression fractures. Strong core muscles help keep the spine stable, lowering the chance of more injuries. We suggest exercises that work the abdominal and back muscles gently, without harming the spine.
Some good core strengthening exercises are:
- Pelvic tilts
- Gentle planks
- Bridging exercises
- Leg raises
Posture Improvement Techniques
Good posture is key to lessening spine strain and preventing more fractures. Physical therapists teach patients how to stand and sit correctly. They also show them how to lift things properly.
| Activity | Proper Posture Technique |
| Lifting Objects | Bend at the knees, keep the object close to the body, and lift with the legs |
| Sitting | Maintain a straight back, feet flat on the floor or on a footrest, and shoulders relaxed |
| Standing | Keep shoulders back, weight evenly distributed on both feet, and engage core muscles |
Gradual Return to Activities
Going back to normal activities slowly is important to avoid injury. Physical therapists help patients slowly increase their activity levels. They watch for any signs of strain or pain.
Key steps for a slow return to activities include:
- Start with low-intensity activities and slowly increase the intensity
- Watch pain levels and adjust activities as needed
- Take rest days when necessary
With a structured physical therapy program, patients with spinal compression fractures can get a stronger, more stable spine. This improves their overall quality of life.
Step 5: Advanced Treatment Options for Specific Fracture Locations
Advanced treatments for compression fractures depend on where the fracture is in the spine. The location and how bad the fracture is help decide the best treatment.
L1 Compression Fracture Treatment
L1 vertebra fractures are common because of its spot at the spine’s transition. Treatment usually includes pain relief, bracing, and physical therapy. Sometimes, surgery is needed to keep the spine stable.
Key considerations for L1 fracture treatment include:
- Checking how bad the fracture is and its effect on the spine
- Managing pain well with medicine and other methods
- Using bracing to help the spine heal
- Physical therapy to keep the spine mobile and strong
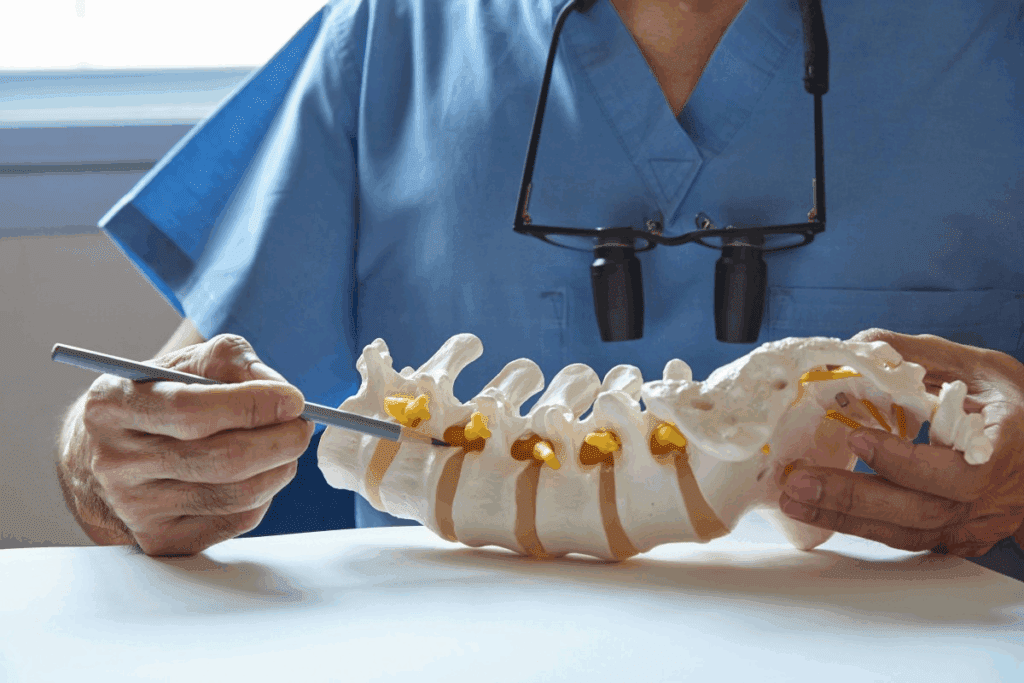
T12-L1 Compression Fracture Management
Fractures at T12-L1 are tricky because of the area’s nature. Managing these fractures needs a team effort from orthopedic and neurosurgical experts.
Treatment strategies may include:
- Bracing and pain control for less severe fractures
- Surgery for more severe fractures or instability
- Physical therapy to improve mobility and prevent future fractures
Treating L5 and Lower Lumbar Fractures
L5 and lower lumbar fractures face unique challenges. Treatment often combines conservative methods and surgery to ensure stability.
Important aspects of treating L5 fractures include:
- Checking the fracture’s severity and its effect on the spine
- Pain management with the right medication and methods
- Bracing to support the lower lumbar spine
- Physical therapy to keep the spine mobile and prevent future issues
Multiple-Level Fractures (T11-T12) Approach
Dealing with fractures at T11-T12 requires a detailed and personalized approach. These fractures can be tough because of the risk of spinal instability.
Key elements of managing multiple-level fractures include:
- Imaging studies to see how bad the fractures are
- A treatment plan from a team that might include surgery
- Aggressive pain management to improve life quality
- Rehabilitation to restore spinal function and mobility
Step 6: Minimally Invasive Procedures for Persistent Pain
We offer minimally invasive procedures for those with persistent pain from spinal compression fractures. These advanced techniques can greatly help. They improve the quality of life for those with vertebral compression fractures.
Vertebroplasty Procedure Explained
Vertebroplasty is a procedure that injects bone cement into a fractured vertebra. It stabilizes and strengthens the vertebra. This helps reduce pain and aids in healing.
The procedure is done under local anesthesia and sedation. This ensures the patient is comfortable during the process.
Benefits of Vertebroplasty:
- Rapid pain relief
- Minimally invasive with small incisions
- Quick recovery time
- Effective in stabilizing the vertebra
Kyphoplasty for Vertebral Height Restoration
Kyphoplasty is a procedure that stabilizes the vertebra and aims to restore lost height. It uses a balloon to create space before injecting bone cement. This can improve spinal alignment and reduce deformity risk.
Key Advantages of Kyphoplasty:
- Restoration of vertebral height
- Improvement in spinal alignment
- Reduction in kyphotic deformity
- Pain relief and stabilization
| Procedure | Pain Relief | Vertebral Height Restoration | Recovery Time |
| Vertebroplasty | Rapid | No | Quick |
| Kyphoplasty | Significant | Yes | Moderate |
Both vertebroplasty and kyphoplasty are effective for managing pain from vertebral compression fractures. The right choice depends on the patient’s condition and overall health.
Conclusion: Recovery Timeline and Long-term Management
Recovering from spinal compression fractures needs a full plan. This includes different treatments and changes in daily life. We’ve shown how to handle compression fractures, from the first steps to more advanced treatments.
How long it takes to get better varies for each person. But, most see big improvements in a few months. Keeping a healthy weight, exercising, and good posture are key to managing symptoms long-term.
It’s also important to see doctors regularly. This helps keep an eye on your spine and solve any problems fast. By doing these things, people can lower the chance of more fractures and live better.
Knowing how to treat and manage spinal compression fractures helps patients help themselves. By mixing medical care with lifestyle changes, people can get the best results and keep their spine healthy for a long time.
FAQ
What is a compression fracture in the spine?
A compression fracture in the spine happens when a vertebra collapses. This can be due to osteoporosis or trauma. It leads to a loss of height and can cause pain and deformity.
What are the common causes of spinal compression fractures?
Spinal compression fractures are often caused by osteoporosis, trauma, or cancer. Osteoporosis weakens bones, making them more likely to fracture.
How are compression fractures diagnosed?
Doctors diagnose compression fractures through physical exams, medical history, and imaging. X-rays, CT scans, or MRI scans help see how bad the fracture is.
What are the symptoms of a spinal compression fracture?
Symptoms include sudden, severe back pain and limited mobility. Some people may also feel numbness or weakness in their legs.
What are the treatment options for compression fractures?
Treatment options range from pain medication and rest to surgery like vertebroplasty and kyphoplasty. The choice depends on the fracture’s severity and location.
How is pain managed in the initial stages of a compression fracture?
Pain management starts with pain relief medications and rest. Physical therapy is also used to ease discomfort.
What is the role of bracing in treating compression fractures?
Bracing stabilizes the spine and reduces pain by limiting movement. It helps the fracture heal. The type of brace used depends on the fracture’s location and severity.
Can physical therapy help in recovering from a compression fracture?
Yes, physical therapy is key in recovery. It strengthens the core, improves posture, and helps return to normal activities. This reduces the risk of further injury.
What are vertebroplasty and kyphoplasty, and how do they help?
Vertebroplasty and kyphoplasty are procedures that inject bone cement into the fractured vertebra. They stabilize it and reduce pain. Kyphoplasty also aims to restore some lost height.
How long does it take to recover from a spinal compression fracture?
Recovery time varies based on the fracture’s severity, treatment, and individual factors. It can take several months to see significant improvement and implement long-term strategies.
What are the risks if a compression fracture is left untreated?
Untreated fractures can cause segmental instability, neurological deficits, chronic pain, and deformity. These issues can significantly impact quality of life.
How can future fractures be prevented?
Preventing future fractures involves managing osteoporosis, eating a healthy diet, exercising regularly, and avoiding smoking and excessive alcohol. These steps help keep bones strong.
References
Mauri, G., et al. (2025). Evaluating the quality of online medical information videos on vertebroplasty and kyphoplasty for spinal fractures. Skeletal Radiology, 54, 1343–1352. https://pubmed.ncbi.nlm.nih.gov/40473987/