
At Liv Hospital, we know patients with atrial fibrillation (AFib) are curious about pacemakers as a treatment. AFib is often found during routine health checks. Our doctors listen to your heartbeat and look for other heart issues.
A pacemaker doesn’t cure AFib, but it can help manage symptoms. It’s very helpful for those with bradycardia or heart block. We help every step of the way, making sure you get care that fits your needs.
Learn how an atrial fibrillation pacemaker helps control heart rhythm, reduce symptoms, and improve heart function.
Key Takeaways
- Pacemakers can help manage AFib symptoms in certain patients.
- AFib diagnosis involves examining the patient’s heartbeat and checking for underlying conditions.
- A pacemaker is not a cure for AFib but can improve quality of life.
- Patients with bradycardia or heart block may benefit from a pacemaker.
- Comprehensive care is essential for managing AFib effectively.
Understanding Atrial Fibrillation and Its Challenges
Atrial fibrillation (AFib) is a heart condition that affects millions. It makes the heart beat irregularly and quickly. This can cause serious problems if not treated right.
What Happens During Atrial Fibrillation?
In AFib, the heart’s upper chambers beat chaotically. This is different from the lower chambers. Symptoms include palpitations, shortness of breath, and fatigue.
The irregular heartbeat can also cause blood to pool. This increases the risk of stroke and heart problems.
Common Symptoms and Complications
AFib symptoms vary. Some common ones are:
- Heart palpitations or fluttering
- Shortness of breath
- Fatigue or weakness
- Dizziness or lightheadedness
- Chest discomfort or pain
AFib complications can be serious. They include a higher risk of stroke, heart failure, and other heart problems. Managing AFib well is key to reducing these risks and improving life quality.
Traditional Treatment Approaches
Treatment for AFib aims to restore a normal heart rhythm. It also controls the heart rate and prevents blood clots. Traditional methods include:
- Medications to control heart rate or rhythm
- Anticoagulants to prevent blood clots
- Cardioversion, a procedure that uses electrical shocks to restore a normal heart rhythm
- Catheter ablation, a minimally invasive procedure to destroy the abnormal electrical pathways in the heart
Pacemakers can also help manage AFib. They are important for patients with certain heart rhythm problems.
The Role of Pacemakers in Cardiac Rhythm Management
Pacemakers are key in managing heart rhythm disorders. They ensure the heart beats at a steady and correct rate. These small devices have changed how we treat heart issues, like irregular heartbeats.
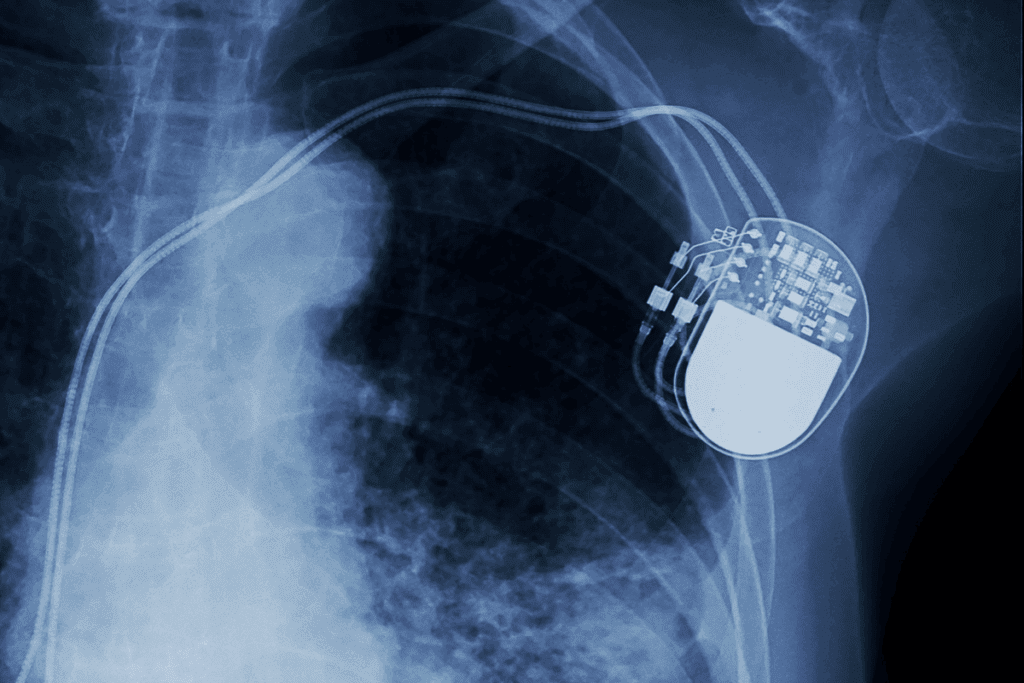
How Pacemakers Function
A pacemaker helps control or boost the heartbeat. It sends signals to the heart to keep it beating right. It has two main parts: the pulse generator and the leads.
The pulse generator is a small metal box with a battery and circuitry. The leads are insulated wires that connect the pulse generator to the heart.
The pacemaker works in several steps:
- Sensing the heart’s natural rhythm
- Determining if a heartbeat is needed
- Generating and delivering an electrical impulse to the heart
- Adjusting the pacing rate according to the body’s needs
Different Types of Pacemakers
There are many types of pacemakers, each for different heart issues. The main types are:
- Single Chamber Pacemakers: These have one lead and pace either the right atrium or the right ventricle.
- Dual Chamber Pacemakers: With two leads, these pacemakers pace both the right atrium and the right ventricle, mimicking a natural heartbeat.
- Biventricular Pacemakers: Used in cardiac resynchronization therapy, these devices have three leads and help synchronize the left and right ventricles.
Primary Indications for Pacemaker Implantation
Pacemakers are used for many reasons, mainly to treat slow or irregular heartbeats. Common reasons include:
- Bradycardia (slow heart rate)
- Heart block
- Certain types of heart failure
- Syncope (fainting) due to heart rhythm disturbances
Knowing about pacemakers helps us see their importance in managing heart rhythm disorders. They offer great benefits for patients with atrial fibrillation.
Can a Pacemaker Cure Atrial Fibrillation?
Pacemakers can help manage some parts of atrial fibrillation (AFib). But they can’t solve the whole problem. AFib makes the heart beat irregularly and too fast, leading to serious issues if not treated right.
Limitations of Pacemakers for AFib Treatment
Pacemakers help control heart rhythm but have limits with AFib. They don’t fix the root cause of AFib; they just manage symptoms. They’re often used with other treatments like medicines or ablation to control AFib well.
Pacemakers are mainly for AFib patients with slow heart rates or after AV node ablation. AV node ablation uses heat to destroy a heart area, needing a pacemaker to keep the rhythm right.
Realistic Expectations for AFib Management
A pacemaker doesn’t cure AFib. It helps manage some parts of it, like slow heart rates or when medicines slow the heart too much. Patients should know what a pacemaker can and can’t do for AFib.
Important things to remember include:
- A pacemaker helps with rhythm but doesn’t stop AFib episodes.
- Pacemakers are often used with other treatments to manage AFib well.
- Regular check-ups and care are key for the best results.
The Concept of “AFib with Pacemaker”
“AFib with pacemaker” means managing atrial fibrillation with a pacemaker. This helps control the heart rhythm, mainly when AFib causes slow heart rates or heart block.
Living with “AFib with a pacemaker” means ongoing care. This includes sticking to medicines, regular check-ups, and making lifestyle changes. Patients should team up with their doctors to get the best treatment and improve their life quality.
In summary, pacemakers are helpful in managing AFib but not a cure. Knowing what pacemakers can and can’t do helps patients make better choices for their treatment. This way, they can manage their AFib better.
When Is an Atrial Fibrillation Pacemaker Recommended?
Doctors decide to put a pacemaker in AFib patients based on several factors. A pacemaker isn’t a cure for AFib. But, it can help manage some parts of the condition.
AFib with Bradycardia or Heart Block
Bradycardia or heart block are main reasons for a pacemaker in AFib patients. Bradycardia means a heart beats too slow. This can happen in some AFib patients, mainly when they take certain medicines. A pacemaker keeps the heart rate right, ensuring blood flows well and lessening symptoms like dizziness or tiredness.
Rate Control Challenges with Medications
Some AFib patients face issues with controlling their heart rate with medicines. In these cases, a pacemaker can help along with other treatments. This is helpful when medicines don’t work well or have bad side effects.
Post-Ablation Rhythm Support
After an ablation for AFib, some patients need a pacemaker for rhythm support. Ablation might make the heart beat too slow. A pacemaker is needed to keep the heart rhythm right.
The “Pace and Ablate” Strategy
The “pace and ablate” strategy combines a pacemaker with AV node ablation. This involves removing the AV node to control the heart rhythm and then implanting a pacemaker. It’s for patients with AFib who don’t get better with medicines or other treatments.
Key considerations for the “pace and ablate” strategy include:
- Careful patient selection based on individual clinical profiles
- Potential benefits, such as improved symptom control and quality of life
- Ongoing monitoring and follow-up care to adjust pacemaker settings as needed
Understanding these scenarios helps us see how pacemakers help with AFib. We can see when they are recommended.
Clinical Evidence: Effectiveness of Pacemakers for AFib
Pacemakers are a key treatment for AFib, backed by clinical research. They help reduce symptoms and improve life quality. Let’s look at how pacemakers work for AFib and their benefits.
Research on Atrial Pacing Techniques
Research on atrial pacing for AFib is ongoing. Techniques like atrial overdrive pacing and atrial antitachycardia pacing (ATP) show promise. Atrial overdrive pacing aims to prevent AFib by pacing the atrium faster. Atrial antitachycardia pacing (ATP) stops atrial tachycardia before it turns into AFib.
These methods are most helpful for patients with heart rate issues. They help keep the heart rate steady, reducing AFib episodes.
Symptom Reduction and Quality of Life Improvements
Pacemakers aim to reduce symptoms and improve life quality for AFib patients. Studies show they can control heart rate and lessen AFib episodes. This helps with symptoms like palpitations and shortness of breath.
With better symptom control, patients can live more comfortably. They can do daily tasks with more confidence. Many patients report a big improvement in their well-being after getting a pacemaker.
Patient Selection Factors for Optimal Outcomes
The success of pacemakers for AFib depends on patient selection. Finding the right candidates is key for the best results. The heart condition, presence of bradycardia, and response to other treatments matter a lot.
Choosing the right patient involves a detailed look at their medical history and current health. Tailoring pacemaker therapy to each patient’s needs can lead to better outcomes.
Specialized Pacing Techniques for AFib Management
Advanced pacing techniques offer new hope for managing atrial fibrillation. These methods are part of our growing arsenal against AFib.
Atrial Overdrive Pacing
Atrial overdrive pacing prevents atrial fibrillation by pacing the atrium faster than the heart naturally beats. It’s very effective for patients with paroxysmal AFib, reducing arrhythmic episodes.
Studies show it can greatly reduce AFib burden in some patients. By pacing the atrium faster, we can stop AFib episodes from starting.
Atrial Antitachycardia Pacing (ATP)
Atrial antitachycardia pacing (ATP) is another advanced technique for managing AFib. It involves sending a burst of pacing pulses to the atrium to end tachycardia or AFib episodes.
ATP’s success varies among patients. But for those who benefit, it can greatly improve their quality of life by cutting down on AFib episodes.
| Pacing Technique | Mechanism | Potential Benefits |
| Atrial Overdrive Pacing | Pacing atrium at a higher rate than intrinsic heart rate | Reduces AFib episodes, improves heart rate control |
| Atrial Antitachycardia Pacing (ATP) | Delivering burst pacing to terminate tachycardia/AFib | Terminates AFib episodes, improves quality of life |
Cardiac Resynchronization Therapy Considerations
Cardiac resynchronization therapy (CRT) is mainly for patients with heart failure and left ventricular dysfunction. It’s not a direct treatment for AFib but can help those with both conditions.
CRT synchronizes the left and right ventricles’ contractions, boosting heart efficiency. For patients with AFib and heart failure, CRT can improve symptoms, exercise ability, and overall quality of life.
“Cardiac resynchronization therapy has emerged as an important treatment option for patients with heart failure, including those with atrial fibrillation.”
— European Heart Journal
By using these specialized pacing techniques, we can better manage atrial fibrillation. This improves patients’ cardiac health and quality of life.
The Pacemaker Implantation Procedure for AFib Patients
The pacemaker implantation procedure is a big step for AFib patients. It has several stages from getting ready to aftercare. We’ll walk you through what to expect, easing your worries and getting you ready for the treatment.
Pre-Procedure Preparation
Before the pacemaker implantation, patients go through a lot of prep work. Comprehensive pre-procedure preparation is key to reduce risks and get the best results.
- Medical history review and physical examination
- Lab tests, including blood work and ECG
- Imaging tests, such as chest X-rays or echocardiogram
- Medication review and adjustment as necessary
- Informed consent and discussion of possible risks and benefits
We also tell patients to get someone to drive them home after the procedure. They should plan to rest for a few days after.
What Happens During Implantation
The pacemaker implantation procedure has several steps. It’s done under local anesthesia and sedation to make it as comfortable as possible.
- Insertion of a venous catheter to guide the pacemaker leads
- Placement of the pacemaker leads in the right heart chamber(s)
- Positioning of the pacemaker generator under the skin
- Testing of the pacemaker to ensure it’s working right
- Closure of the incision site
The whole procedure usually takes a few hours. Patients are watched closely the whole time.
Immediate Post-Procedure Care
After the procedure, patients go to a recovery area for monitoring. Immediate post-procedure care focuses on making sure the patient is comfortable and safe. It also checks if the pacemaker is working right.
- Monitoring of vital signs and pacemaker function
- Rest and limited activity for the rest of the day
- Follow-up checks on the incision site for signs of infection or complications
- Patient education on pacemaker care and follow-up appointments
We stress the importance of following post-procedure instructions carefully. This helps avoid complications and ensures a smooth recovery.
Recovery and Adaptation After Pacemaker Placement
Recovering from pacemaker placement involves several steps and precautions. It’s important to know about the recovery timeline, activity limits, and adjusting to life with a pacemaker.
Short-Term Recovery Timeline
The first few weeks are the main recovery period. Patients might feel some discomfort, swelling, or bruising at the pacemaker site. A gradual recovery plan is recommended, which includes:
- Resting adequately to allow the body to heal
- Monitoring the pacemaker site for signs of infection or complications
- Attending follow-up appointments with your healthcare provider
Activity Restrictions and Precautions
Some activities should be avoided or modified in the short term. Key precautions include:
- Avoiding heavy lifting, bending, or strenuous activities for a few weeks
- Being cautious with the arm on the side of the pacemaker implantation to prevent dislodging the leads
- Informing your healthcare provider about any unusual symptoms or device alerts
Adjusting to Life with a Pacemaker
As patients recover, they must also adjust to life with a pacemaker. This means understanding how the device works, recognizing its signals, and making lifestyle changes. It’s a process that requires patience and support from healthcare providers. We encourage patients to:
- Keep a device diary to track any irregularities or concerns
- Stay informed about their pacemaker’s settings and any necessary adjustments
- Gradually resume normal activities under the guidance of their healthcare team
By following these guidelines and maintaining open communication with their healthcare providers, patients can navigate the recovery and adaptation process successfully. This ensures the optimal functioning of their pacemaker and an improved quality of life.
Living with Both AFib and a Pacemaker
Living with AFib and a pacemaker is challenging. It requires careful management. Understanding the ongoing needs and adjustments is key to staying healthy.
Ongoing Medication Requirements
Even with a pacemaker, AFib patients might need medicines. Anticoagulants help prevent stroke. Rate-control medications manage heart rate during AFib. We tailor medication plans to each patient’s needs.
Managing medicines is vital for AFib and pacemaker patients. Regular checks help adjust doses and ensure medicines work well.
Monitoring and Follow-Up Care
Regular visits with our team are essential. These visits help us check the pacemaker and adjust settings. Remote monitoring tracks the pacemaker’s performance and catches issues early.
- Regular check-ups to monitor pacemaker function
- Adjustments to medication and pacemaker settings
- Ongoing assessment of AFib symptoms and management
Managing AFib Episodes with a Pacemaker
A pacemaker helps with AFib but doesn’t cure it. Patients may have AFib episodes. Techniques like vagal maneuvers or anti-arrhythmic medications can help manage these episodes.
Lifestyle Considerations and Adjustments
AFib and a pacemaker require lifestyle changes. Eating less caffeine and alcohol helps. Regular physical activity improves heart health. Stress management techniques like meditation or yoga can also help.
| Lifestyle Adjustment | Benefit |
| Dietary Changes | Reduces AFib symptoms |
| Regular Physical Activity | Improves heart health |
| Stress Management | Reduces frequency and severity of AFib episodes |
By making the right adjustments, patients with AFib and a pacemaker can live well. Our team is here to support and guide you through this complex condition.
Conclusion: Making Informed Decisions About Pacemakers for AFib
We’ve looked into how pacemakers help with atrial fibrillation (AFib). A pacemaker isn’t a cure but can help manage symptoms. It can improve life quality for some patients.
Studies show that certain pacing methods might lower AFib in some patients. But, they don’t always stop AFib. The ‘pace and ablate’ method is often used. It involves removing part of the heart and using a pacemaker to control rhythm.
To make good choices about pacemakers for AFib, patients need to know the pros and cons. They should understand how pacing fits into their treatment plan. This way, patients and doctors can work together to better outcomes and life quality. Knowing all the treatment options, including pacemakers, is key.
FAQ
Can a pacemaker cure atrial fibrillation?
No, a pacemaker can’t cure atrial fibrillation. But, it can help manage symptoms and improve life quality for patients.
What is the role of a pacemaker in managing atrial fibrillation?
A pacemaker controls the heartbeat. It’s a valuable tool for managing atrial fibrillation symptoms, mainly in patients with bradycardia or heart block.
Can you stil have atrial fibrillation with a pacemaker?
Yes, having a pacemaker doesn’t stop atrial fibrillation episodes. Patients can have AFib with a pacemaker, but the device can manage symptoms.
When is a pacemaker recommended for atrial fibrillation?
A pacemaker is recommended for atrial fibrillation in specific cases. This includes AFib with bradycardia or heart block, challenges with rate control meds, post-ablation rhythm support, and the “pace and ablate” strategy.
Can a pacemaker help with AFib and fast heart rate?
A pacemaker can manage some aspects of atrial fibrillation. But, it’s not used to directly treat a fast heart rate from AFib. Some pacing techniques, like atrial overdrive pacing, can help.
What are the benefits of a pacemaker for atrial fibrillation treatment?
Pacemakers for AFib treatment reduce symptoms and improve life quality. They support certain AFib management strategies, like rate control and rhythm control.
What are the limitations of pacemakers for AFib treatment?
Pacemakers can’t cure atrial fibrillation. They may not stop AFib episodes. Pacemakers might not work for all AFib patients, and their success varies by patient.
How does a pacemaker work in managing atrial fibrillation?
A pacemaker sends electrical impulses to the heart to control the heartbeat. In AFib patients, it can regulate the heart rhythm and improve symptoms.
What are the different types of pacemakers available for AFib management?
There are single-chamber, dual-chamber, and biventricular pacemakers. The right pacemaker depends on the patient’s needs and AFib characteristics.
What is the “pace and ablate” strategy for AFib management?
The “pace and ablate” strategy uses a pacemaker with an ablation procedure for AFib management. It’s effective for some patients, mainly those with symptomatic bradycardia or heart block.
How do I adjust to living with a pacemaker and AFib?
Living with a pacemaker and AFib requires ongoing management. This includes sticking to medication, monitoring, and follow-up care. Patients should also make lifestyle changes to manage their condition well.
References
- Kreimer, F., et al. (2024). Pacemaker-induced atrial fibrillation reconsidered: mechanisms, associations and prevention. [Article].https://www.ncbi.nlm.nih.gov/articles/PMC11217490/
- Parkkari, E., et al. (2023). The incidence of atrial fibrillation, new oral anticoagulation, and outcomes in patients with dual-chamber pacemakers. [Article]. https://www.sciencedirect.com/science/article/pii/S2352906723001380









