Learn what causes plaque in arteries and how it contributes to hardening and atherosclerosis.
Atherosclerosis is a common condition where plaque builds up in the arteries. This reduces the supply of oxygen-rich blood to vital organs. At Liv Hospital, we focus on understanding this buildup to prevent and treat it well.
Plaque formation is a complex process. Early detection is very important. By knowing what causes plaque buildup, people can make better lifestyle choices and seek medical help to lower their risk.
At Liv Hospital, we aim to offer top-notch healthcare. We provide full support for international patients. Our team is ready to help you understand and manage atherosclerosis.
Key Takeaways
- Plaque buildup in arteries can lead to hardening and reduce blood flow.
- Understanding the causes of plaque formation is key for prevention.
- Lifestyle changes and medical interventions can help reduce the risk.
- Early detection is vital for managing atherosclerosis effectively.
- Liv Hospital offers complete care for international patients.
Understanding Arterial Plaque and Arterial Hardening

It’s key to know how arterial plaque and hardening work to understand heart health. These two issues affect the arteries, causing heart diseases.
Defining Atherosclerosis and Arteriosclerosis
Atherosclerosis and arteriosclerosis are often mixed up, but they’re different. Atherosclerosis is when plaque, made of fat and cholesterol, builds up in arteries. This can block blood flow. Arteriosclerosis is when arteries get hard and stiff, often because of plaque buildup or aging.
Here’s what sets them apart:
- Atherosclerosis is mainly about plaque buildup.
- Arteriosclerosis is about arteries getting hard.
- Atherosclerosis is a type of arteriosclerosis.
The Relationship Between Plaque Formation and Arterial Hardening
Plaque buildup is a big part of why arteries harden. As plaque grows, it can damage the artery’s lining. This damage can make the artery stiff and less flexible over time.
The link between plaque and hardening goes like this:
- First, plaque starts to build up due to lipids and inflammation.
- Then, the plaque grows, causing more inflammation and damage.
- Next, the artery walls start to harden and calcify.
- Lastly, the artery becomes less flexible, raising the risk of heart problems.
Understanding these steps helps us see why keeping our hearts healthy is so important. We can do this through good lifestyle choices and sometimes, medical help.
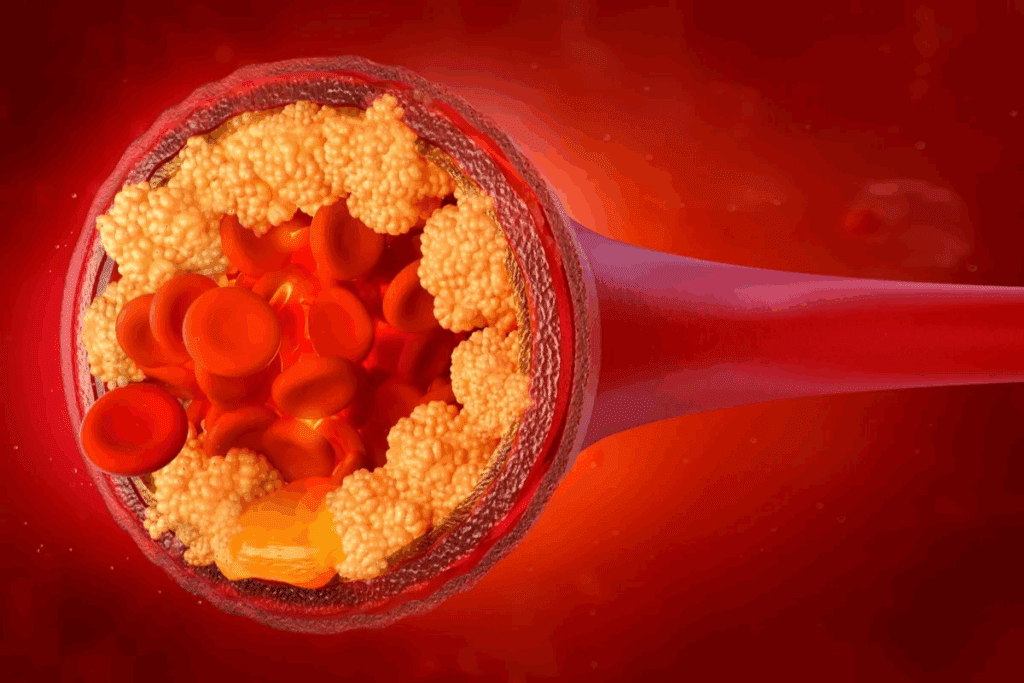
The Composition of Arterial Plaque
Understanding what makes up arterial plaque is key to knowing its impact on heart health. Arterial plaque is a mix of substances that build up inside arteries, causing atherosclerosis.
Lipids and Cholesterol
Lipids, like cholesterol, are important in forming arterial plaque. Low-density lipoprotein (LDL) cholesterol, or “bad” cholesterol, is a big player in plaque formation. LDL cholesterol can get into the artery wall, where it gets oxidized and starts inflammation.
Inflammatory Cells
Inflammatory cells, like macrophages and T lymphocytes, play a big role in plaque formation. These cells are drawn to lipid buildup and add to the inflammation in the plaque. Their presence can make the plaque unstable, increasing the risk of rupture.
Calcium Deposits
Calcium deposits are a key part of arterial plaque. The calcification process involves calcium phosphate crystals forming in the plaque. Arterial calcification is a sign of advanced atherosclerosis and raises the risk of heart disease.
Fibrous Tissue
Fibrous tissue, made of collagen and smooth muscle cells, is also part of arterial plaque. The fibrous cap on the plaque helps keep it stable. But if this cap gets thin or breaks, it can cause sudden heart problems.
In summary, arterial plaque is made up of lipids, inflammatory cells, calcium deposits, and fibrous tissue. Knowing about these parts is vital for finding ways to stop and treat atherosclerosis.
What Causes Plaque in Arteries: The Initial Stages
The journey to plaque in arteries starts with damage to the endothelium. This is the innermost layer of blood vessels. It’s vital for keeping blood vessels healthy. Damage to this layer triggers a series of events leading to plaque formation.
Endothelial Dysfunction
Endothelial dysfunction is the first step towards atherosclerosis. It happens when the endothelium can’t do its job right. This includes controlling blood flow and immune responses. High blood pressure, diabetes, smoking, and high LDL cholesterol levels can cause this dysfunction.
When the endothelium is not working well, it lets lipids and inflammatory cells into the arterial wall.
Lipid Infiltration
Lipid infiltration is a key early step in plaque formation. LDL cholesterol is a major player here. When LDL cholesterol gets into the arterial wall, it can oxidize and start an inflammatory response. This lipid buildup leads to fatty streaks, which are the first signs of atherosclerosis.
We’ll look at how these streaks turn into more serious plaques later.
Inflammatory Response
The inflammatory response is a big part of atherosclerosis. Lipids in the arterial wall attract inflammatory cells like macrophages and T lymphocytes. These cells release substances that make inflammation worse and help the plaque grow. This ongoing inflammation is what makes a plaque more dangerous over time.
Understanding this process is key to finding ways to prevent and treat atherosclerosis.
The Progression from Fatty Streaks to Advanced Plaques
As we get older, plaque in our arteries can grow from simple fatty streaks to complex lesions. This change is key to understanding atherosclerosis and its serious risks.
Formation of Fatty Streaks
The first step in plaque formation is the fatty streak. These yellowish deposits start on the inner artery lining. They are made of lipid-laden macrophages, or foam cells. Fatty streaks can start in childhood and are the first sign of atherosclerosis.
Factors influencing the formation of fatty streaks include:
- Lipid infiltration into the arterial wall
- Endothelial dysfunction
- Inflammatory response
Development of Fibrous Plaques
Over time, fatty streaks turn into fibrous plaques. These plaques have a fibrous cap over a lipid-rich core. The cap is made of smooth muscle cells and extracellular matrix, making the plaque stable.
Advanced Lesions and Complicated Plaques
As atherosclerosis gets worse, fibrous plaques become more complex. They are called advanced lesions or complicated plaques. These can calcify, ulcerate, or hemorrhage, raising the risk of heart attacks or strokes.
| Stage of Plaque Progression | Characteristics | Clinical Implications |
| Fatty Streaks | Lipid-laden macrophages, early sign of atherosclerosis | Often asymptomatic, can regress |
| Fibrous Plaques | Fibrous cap over lipid-rich core, stable plaque | May stay stable or become advanced lesions |
| Advanced Lesions/Complicated Plaques | Calcification, ulceration, or hemorrhage | High risk of heart attacks or strokes |
Knowing how plaque progresses from fatty streaks to advanced plaques is vital. It helps us create better prevention and treatment plans for atherosclerosis. By understanding what affects plaque growth, we can manage heart disease risk better and improve patient care.
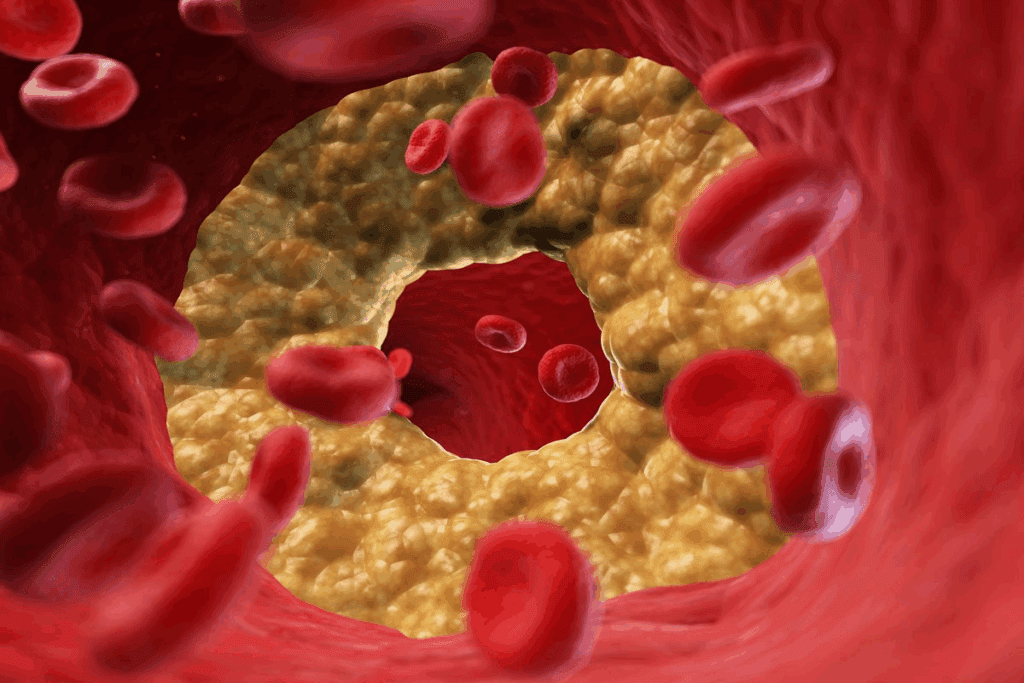
How Plaque Leads to Arterial Hardening
Plaque buildup in arteries starts a series of changes that harden them. This process is complex. It involves several mechanisms that lead to the loss of elasticity and hardening of the arterial walls.
The Calcification Process
Calcification is a key factor in arterial hardening. As plaque builds up, it attracts calcium deposits. This forms hard, calcified plaques that make the arterial walls rigid.
Calcification is a critical step in the progression from plaque buildup to arterial hardening. It not only makes the arteries more rigid but also complicates the treatment of arterial disease.
Loss of Arterial Elasticity
The loss of arterial elasticity is another significant consequence of plaque buildup. As the arteries become more clogged with plaque, their walls become less flexible. This loss of elasticity impairs the arteries’ ability to accommodate the normal fluctuations in blood pressure, leading to increased strain on the cardiovascular system.
We observe that the loss of elasticity is not just a passive consequence of plaque buildup; it’s an active process that involves changes in the arterial wall structure and function.
Arterial Remodeling
Arterial remodeling refers to the changes that occur in the arterial walls in response to plaque buildup. While some remodeling can be compensatory, attempting to maintain luminal diameter despite plaque accumulation, excessive remodeling can lead to further complications, including arterial hardening.
The process of arterial remodeling is complex and involves various cellular and molecular mechanisms. Understanding these mechanisms is critical for developing effective treatments for arterial hardening.
In conclusion, the progression from plaque buildup to arterial hardening involves a complex interplay of calcification, loss of elasticity, and arterial remodeling. By understanding these mechanisms, we can better appreciate the importance of early intervention and prevention in maintaining cardiovascular health.
Major Risk Factors for Atherosclerosis
Atherosclerosis is a complex condition influenced by various risk factors. These can be changed or are fixed. Knowing these factors is key to preventing and treating the condition.
Modifiable Risk Factors
Modifiable risk factors are things we can change. They include:
- High Blood Cholesterol: Too much LDL cholesterol and not enough HDL cholesterol can cause plaque.
- Hypertension: High blood pressure damages arterial walls, making them more prone to plaque buildup.
- Smoking: Smoking damages blood vessel linings and reduces blood flow.
- Diabetes: Diabetes mellitus increases atherosclerosis risk due to high blood sugar damaging blood vessels.
- Obesity and Physical Inactivity: Being overweight and inactive can lead to hypertension and diabetes.
- Unhealthy Diet: Eating too much saturated fats, trans fats, and cholesterol can cause atherosclerosis.
Non-Modifiable Risk Factors
Non-modifiable risk factors are things we can’t change. These include:
- Age: The risk of atherosclerosis grows with age.
- Family History: A family history of early heart disease is a big risk factor.
- Genetics: Some genetic conditions can lead to high cholesterol or other risks.
- Gender: Men are generally at higher risk, but women’s risk increases after menopause.
Knowing both modifiable and non-modifiable risk factors helps us manage and prevent atherosclerosis. By focusing on what we can change and understanding what we can’t, we can lower our risk of getting this condition.
The Silent Progression: How Early Does Plaque Buildup Begin?
Atherosclerosis, a condition where plaque builds up, starts quietly in childhood. This is both surprising and worrying. It shows we need to be aware and take steps early.
Studies reveal atherosclerosis can start in young children. Let’s dive into this.
Childhood Origins of Atherosclerosis
Atherosclerosis starts in childhood. Research finds fatty streaks, early plaque signs, in kids as young as 10. These changes are influenced by genetics, diet, and lifestyle.
Risk factors like high cholesterol, obesity, and smoking speed up plaque buildup. It’s key for parents and caregivers to know these risks and act early for a healthy start.
Decades of Silent Progression
The change from fatty streaks to advanced plaques takes decades. Over time, the plaque grows and gets more complex. This can lead to narrowed or blocked arteries.
This silent growth is dangerous because it often doesn’t show symptoms until it’s too late. Knowing what influences this progression helps us spot risks early and act fast.
When Symptoms First Appear
Symptoms of atherosclerosis show up later, often when plaque buildup is severe. This can be after a heart attack or stroke. By then, the disease is often advanced, making early detection and prevention critical.
Knowing the risk factors and acting early can lessen atherosclerosis’s impact. Early action helps reduce the disease’s burden.
Clinical Consequences of Arterial Hardening
Arterial hardening has serious effects on heart health. It can greatly impact a patient’s health and life quality.
Coronary Artery Disease
Coronary artery disease (CAD) is a major issue caused by arterial hardening. It happens when arteries to the heart get blocked. This can cause heart pain, heart attacks, and other serious problems.
CAD often starts silently, showing symptoms only when it’s severe. Knowing the risk factors like high blood pressure and smoking is key to preventing it.
Cerebrovascular Disease
Cerebrovascular disease affects blood vessels in the brain. It can cause strokes or TIAs, leading to disability or death.
Hardened arteries in the brain can reduce blood flow. This can lead to brain damage and increase dementia risk. Keeping risk factors under control is vital.
Peripheral Artery Disease
Peripheral artery disease (PAD) narrows arteries in the legs. It causes pain when walking and can lead to more serious problems.
PAD is a sign of widespread artery disease. It greatly affects daily life. Early treatment can help manage symptoms and prevent further damage.
Aneurysms
Arterial hardening can cause aneurysms, which are bulges in arteries. Aneurysms can be life-threatening if they burst.
Aneurysms can cause severe bleeding and organ damage. Monitoring and treating them is essential to prevent these dangers.
In summary, arterial hardening has many serious effects on heart health. Understanding these effects is important for preventing and managing them.
Diagnosing Plaque Buildup and Arterial Hardening
Doctors use different tests to find out if you have plaque buildup and hardening in your arteries. These tests help them figure out the best treatment for you. They are key to keeping your heart healthy.
Non-Invasive Diagnostic Methods
First, doctors often use safe and easy tests to start checking your heart. These tests include:
- Ankle-Brachial Index (ABI): This test compares blood pressure in your ankle and arm to spot artery disease.
- Carotid Ultrasound: It uses sound waves to see the carotid arteries and find plaque.
- Computed Tomography (CT) Scan: This scan gives clear pictures of your heart and arteries, showing plaque and hardening.
These tests are great for finding out who might be at risk for heart problems. They also help track how plaque and hardening change over time.
| Diagnostic Method | Description | Primary Use |
| Ankle-Brachial Index (ABI) | Compares blood pressure in the ankle and arm | Diagnosing Peripheral Artery Disease |
| Carotid Ultrasound | Creates images of the carotid arteries using sound waves | Detecting Plaque Buildup in Carotid Arteries |
| Computed Tomography (CT) Scan | Provides detailed images of the heart and arteries | Assessing Plaque Buildup and Arterial Hardening |
Invasive Diagnostic Procedures
When simple tests don’t give enough information, doctors might use more detailed tests. These include:
- Angiography: This involves putting dye into your arteries to see plaque and narrowings on X-rays.
- Intravascular Ultrasound (IVUS): It uses a special catheter with an ultrasound probe to see inside your arteries.
These tests give doctors a clear picture of plaque and hardening. This helps them make better treatment plans for you.
By using both simple and detailed tests, doctors can accurately find and treat plaque buildup and hardening. This helps manage heart diseases well.
Arteriosclerosis Prevention: Lifestyle Modifications
Lifestyle changes are key to preventing arteriosclerosis and keeping your heart healthy. By making certain changes, you can lower your risk of getting this condition.
Heart-Healthy Diet
Eating right is the first step in preventing arteriosclerosis. Focus on fruits, veggies, whole grains, and lean proteins. Try to cut down on saturated fats, trans fats, and cholesterol. Adding foods rich in omega-3s, like salmon and walnuts, is a great choice.
Regular Physical Activity
Regular exercise is also essential. It helps keep your weight in check, lowers blood pressure, and boosts heart health. Try to do at least 150 minutes of moderate exercise or 75 minutes of vigorous exercise each week.
Smoking Cessation
Quitting smoking is a must to avoid arteriosclerosis. Smoking harms blood vessel linings, making them more prone to blockages. Stopping smoking greatly lowers your risk of heart disease. There are many resources, like counseling and meds, to help you quit.
Stress Management
Managing stress is also important. Chronic stress can lead to arteriosclerosis by increasing blood pressure and unhealthy habits. Meditation, yoga, and deep breathing can help manage stress.
By making these lifestyle changes, you can prevent arteriosclerosis and keep your heart in top shape.
Medical Interventions for Plaque and Arterial Hardening
Managing plaque and arterial hardening often requires lifestyle changes and medical treatments. If lifestyle changes aren’t enough, medical treatments become key.
Pharmacological Treatments
Medications play a big role in treating plaque buildup and hardening arteries. These drugs aim to lower the risk of heart problems by tackling different parts of the disease.
- Statins: These drugs lower cholesterol and have anti-inflammatory effects. They help keep plaques stable and lower the risk of rupture.
- Antiplatelet Agents: Drugs like aspirin and clopidogrel prevent blood clots on plaques. This reduces the chance of heart attacks and strokes.
- Blood Pressure Medications: Keeping blood pressure in check is vital to slow artery hardening. Various drugs, such as ACE inhibitors and beta-blockers, are used to control blood pressure.
Surgical and Interventional Procedures
Surgical and interventional procedures are also used to treat plaque buildup. These methods aim to improve blood flow in arteries narrowed by plaque.
Angioplasty and Stenting: This procedure uses a balloon to widen narrowed arteries. A stent is then placed to keep the artery open.
Endarterectomy: This surgery removes plaque from the artery’s inner lining. It’s often done on carotid arteries to lower stroke risk.
These treatments, whether through medication or surgery, are vital for managing plaque and hardening arteries. They are essential for those at high risk of heart problems. Understanding these options helps patients and doctors make the best decisions.
Conclusion: Taking Control of Arterial Health
Understanding plaque buildup and taking steps to prevent it can greatly lower the risk of heart disease. We’ve looked into how plaque forms and hardens in arteries. This process has a big impact on our health.
To manage arterial health, we need to make lifestyle changes and sometimes seek medical help. Eating right, staying active, and managing stress can help prevent plaque buildup. These actions can also stop arteries from hardening.
Prevention is key, and acting early can greatly improve treatment results. We urge you to take steps to keep your arteries healthy. Work closely with your doctor to watch your health and address any issues.
By taking these steps, we can lower the risk of heart problems and improve our overall health. Taking control of our arterial health is a big step towards a healthier life. We’re here to support you every step of the way.
FAQ
What is the hardening of the arteries?
The hardening of the arteries, also known as arteriosclerosis, is when arteries become stiff and more likely to get damaged. This happens because of plaque buildup.
What is plaque buildup in arteries?
Plaque buildup in arteries means lipids, cholesterol, and other materials gather in the artery walls. This leads to a condition called atherosclerosis.
How does plaque build up in the arteries?
It starts with the arteries not working right. Then, lipids and other substances get in, causing inflammation. This leads to the formation of atherosclerotic plaques.
What is the difference between atherosclerosis and arteriosclerosis?
Atherosclerosis is when plaque builds up in the artery walls. Arteriosclerosis is when the arteries get hard. Atherosclerosis is a type of arteriosclerosis.
What are the major risk factors for atherosclerosis?
Risk factors include high blood pressure, high cholesterol, smoking, and diabetes. Non-modifiable factors are age, family history, and genetics.
Can atherosclerosis be prevented?
Yes, it can be prevented or slowed. This is done through a healthy diet, exercise, quitting smoking, and managing stress.
How is plaque buildup and arterial hardening diagnosed?
Doctors use imaging tests and procedures like angiography to diagnose it.
What are the clinical consequences of arterial hardening?
It can cause serious problems like coronary artery disease and aneurysms. It also affects the brain and peripheral arteries.
How early does plaque buildup in the coronary arteries start?
It can start in childhood. It grows silently for years. So, it’s important to be healthy from a young age.
What are the treatment options for plaque buildup and arterial hardening?
Treatments include medicines, surgeries, and lifestyle changes. These help manage risk factors and slow the disease.
What causes plaque buildup in your arteries?
It’s caused by high lipids and cholesterol, inflammatory cells, calcium, and fibrous tissue.
What is artery plaque made of?
It’s made of lipids, cholesterol, inflammatory cells, calcium, and fibrous tissue.
Why does plaque build up in arteries?
It’s due to a mix of factors. These include endothelial dysfunction, lipid infiltration, and inflammation.
References
Schmidt-Trucksäss, A., Jabbour, G., Kappenstein, J., & Mitáš, J. (2024). Lifestyle factors as determinants of atherosclerotic cardiovascular disease: An update. Atherosclerosis, 380, 73-84. https://doi.org/10.1016/j.atherosclerosis.2024.01.020





