Last Updated on November 25, 2025 by Ugurkan Demir
Understanding male fertility can be complex and sensitive. At Liv Hospital, we combine internationally competitive expertise with exceptional patient care to help individuals evaluate their fertility spermiogram results.
A seminal analysis, or semen analysis, is key for checking male fertility. It gives insights into important fertility factors like volume, sperm count, motility, morphology, and vitality.
The World Health Organization sets standards for a normal semen analysis. A normal report shows a volume of 1.5 mL or more. It also requires a sperm concentration above 15 million per mL and a total sperm count of at least 39 million per ejaculate. We will look at these key points and what they mean for male fertility.
Key Takeaways
- Seminal analysis is the primary test for evaluating male fertility.
- Normal seminal fluid volume is 1.5 mL or more.
- A healthy sperm concentration is above 15 million per mL.
- Total sperm count should be at least 39 million per ejaculate.
- Other key parameters include sperm motility, morphology, and vitality.
The Significance of Male Fertility Testing
Semen analysis is key in checking male fertility. It gives a detailed look at sperm health. For couples trying to conceive, knowing about male fertility is important. Semen analysis is a major tool in this area.
The Role of Semen Analysis in Fertility Assessment
Semen analysis checks sperm count, motility, morphology, and vitality. It gives a full picture of male fertility. This test is vital for spotting sperm health problems that might make it hard to conceive.
Healthcare providers use this test to understand fertility issues. For example, a good semen analysis report shows a certain sperm count, good motility, and normal shape.
When a Spermiogram Is Recommended
A spermiogram, or semen analysis, is suggested when couples can’t conceive. It helps find sperm health issues that might cause infertility.
Doctors usually suggest a spermiogram after a couple tries to conceive without success. This test is very helpful in figuring out male fertility problems.
| Parameter | Normal Value | Significance |
| Sperm Count | Above 15 million/mL | Indicates the number of sperm per milliliter of semen |
| Motility | 40-50% or greater | Reflects the percentage of moving sperm |
| Morphology | 4% or more normal forms | Assesses the shape and structure of sperm |
Knowing about these parameters helps couples understand their fertility. It guides them on what steps to take for a successful pregnancy.
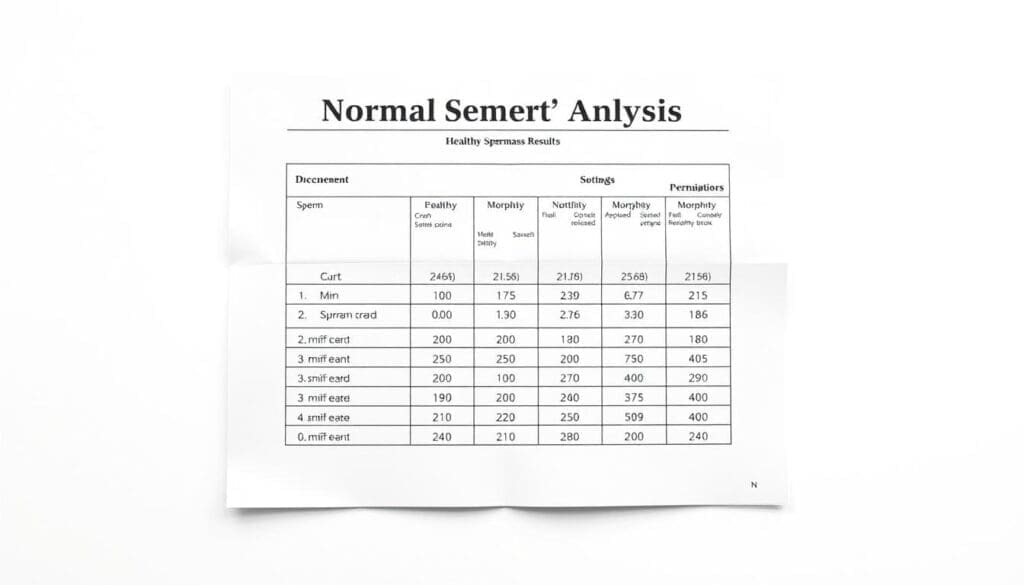
Understanding Spermiogram Results: The Gold Standard Test

Spermiogram analysis is a key test for male fertility. It uses World Health Organization guidelines to understand its results. This test looks at different parts of semen to check fertility.
World Health Organization Reference Values
The World Health Organization has set up detailed reference values for semen analysis. These values come from studies of men who are fertile. They check semen volume, sperm count, total sperm count, motility, and shape.
According to WHO, a good semen analysis has a volume of 1.5 mL or more. It should have a sperm concentration of 15 million per mL or more. The total sperm count should be 39 million or more per ejaculate.
Progressive motility should be 32% or more. Total motility should be 40% or more. For sperm shape, 4% or more should be normal.
How to Interpret Your Seminal Analysis Report
When you get your spermiogram results, compare them to WHO values. If they match, it means you likely have normal sperm in hand and good fertility. But if they don’t match, it might mean you need more tests or to make lifestyle changes.
Look at all parts of your report. A low sperm count or poor motility might mean you need medical help or to change your lifestyle. But if everything looks normal, it’s a good sign, showing a normal sperm test report.
Talking to a healthcare professional is key to understanding your results. They can guide you based on your health and fertility goals.
Seminal Fluid Volume: First Key Parameter
Seminal fluid volume is a key indicator in semen analysis, providing insights into male reproductive health. A normal seminal fluid volume is considered to be 1.5 mL or more. This parameter is very important because it can affect the overall fertility assessment.
Normal Volume Range
A seminal fluid volume of 1.5 mL or more is generally considered within the normal range. This is based on the World Health Organization’s reference values for semen analysis. A volume below 1.5 mL may indicate a condition known as low semen volume or hypospermia, which can be associated with various underlying issues, including hormonal imbalances or blockages in the reproductive tract.
Factors Affecting Ejaculate Volume
Several factors can influence ejaculate volume, including:
- Abstinence period: A longer abstinence period can result in a higher ejaculate volume.
- Age: Ejaculate volume can decrease with age.
- Certain medical conditions: Conditions such as hormonal imbalances or reproductive tract obstructions can affect ejaculate volume.
Understanding these factors is essential for interpreting seminal fluid analysis results accurately. For instance, a man with a low ejaculate volume may be advised to revisit the semen analysis after adjusting his abstinence period.
When evaluating seminal fluid volume, it’s also important to consider it in the context of other semen analysis parameters, such as sperm count and motility, to get a complete picture of male fertility.
Sperm Count and Concentration: Critical Fertility Indicators
Knowing about sperm count and concentration is key to understanding fertility. These numbers tell us how likely it is to get pregnant. We’ll explore what’s considered normal and how these numbers are checked.
Normal Sperm Concentration (Above 15 Million/mL)
Sperm concentration is a big deal in male fertility. It’s measured in millions per milliliter (mL) of semen. A normal count is over 15 million sperm per mL.
Significance of Sperm Concentration: More sperm means better chances of getting pregnant. But, other factors also matter for fertility.
Total Sperm Count (Minimum 39 Million per Ejaculate)
The total sperm count is another important number. It shows the total number of sperm in one ejaculate. A normal count is at least 39 million sperm.
| Parameter | Normal Value |
| Sperm Concentration | >15 million/mL |
| Total Sperm Count | >39 million/ejaculate |
What a Normal Sperm Count Report Means for Fertility
A normal sperm count report is good news for fertility. But, remember, fertility is more than just sperm count. Sperm motility, shape, and health also matter.
It’s reassuring to know that a normal sperm count, along with other healthy factors, boosts chances of getting pregnant. Yet, a full check-up is wise to catch any fertility issues.
Sperm Motility: Assessing Swimming Capability
Sperm motility is key in male fertility. It shows how well sperm can swim to the egg. This helps us see if sperm can fertilize an egg.
Progressive and Non-Progressive Movement
Sperm motility has two types: progressive and non-progressive. Progressive motility means sperm moving straight or in big circles. This is important for reaching the egg. Non-progressive motility includes sperm that move but not straight, or those that don’t move at all.
Normal Motility Percentages (40-50% or Greater)
A good sperm motility report shows 40-50% of sperm moving well. This is key for fertilizing an egg. We check motility to understand a man’s fertility.
| Motility Category | Description | Normal Values |
| Progressive Motility | Sperm moving in a straight line or large circle | ≥ 40-50% |
| Non-Progressive Motility | Sperm moving but not in a straight line | Variable |
| Immotility | Sperm that are not moving | Minimal |
Knowing about sperm motility is important for checking male fertility. A normal report means sperm can swim well, boosting fertilization chances. But, abnormal results might need more tests or treatment.
Sperm Morphology: Evaluating Shape and Structure
Sperm morphology is key in semen analysis, looking at sperm shape and structure. It’s vital because normal morphology is essential for fertilization. Issues with sperm shape can greatly affect fertility.
Understanding the morphology section in a semen analysis report is important. Normal morphology means at least 4% of sperm have the right shape and structure. This percentage shows sperm health.
Normal Morphology Criteria (4% or More)
A semen analysis report shows at least 4% of sperm are normal. This follows the World Health Organization’s semen analysis guidelines. Having 4% or more normal morphology is a good sign of fertility.
Kruger Strict Criteria for Assessment
The Kruger strict criteria evaluate sperm morphology in detail. It checks the head, midpiece, and tail of the sperm. The Kruger criteria offer a thorough look at sperm morphology, spotting fertility issues.
Knowing your sperm morphology results is key to understanding your fertility. If you’re worried, talk to a healthcare professional. They can offer advice and support. Usually, sperm test results are ready in 24 to 72 hours, helping you make quick decisions.
Additional Parameters in Seminal Fluid Analysis Normal Results
To fully understand male fertility, we must look beyond basic tests. Other important factors in seminal fluid analysis offer deeper insights. They help spot issues not seen in standard tests.
Sperm Vitality Assessment
Sperm vitality shows how fertile a man is by counting live sperm. A high count means healthy sperm. But a low count might point to health problems or oxidative stress. We use eosin-nigrosin staining to tell live from dead sperm.
pH and Liquefaction Time
The pH of seminal fluid is key for sperm health. It should be between 7.2 and 8.0. If it’s off, sperm might not work well, causing fertility problems. Liquefaction time, when semen turns from gel to liquid, is also important. It should take 20-30 minutes. If it takes longer, it could mean prostate issues.
White Blood Cell Count and Infection Markers
White blood cells in seminal fluid suggest infection or inflammation. High counts, or leukocytospermia, harm sperm quality and fertility. We check white blood cell counts to find infections or inflammation affecting fertility.
Looking at these extra factors helps us understand male fertility better. It lets us find and fix problems that standard tests miss. This detailed approach is key for accurate diagnoses and effective treatments.
From Sample to Results: The Testing Process
To understand your spermiogram, knowing the testing process is key. It covers from collecting the sample to analyzing it in the lab. This knowledge helps you make sense of your sperm test results.
Proper Sample Collection Techniques
The first step is collecting the sample. Using the right technique is vital for accurate results. The sample should be collected through masturbation after 2-3 days without sex. It’s important to use a sterile container given by the lab.
Keep the sample at body temperature during transport. Then, deliver it to the lab within an hour of collection.
The World Health Organization stresses the importance of proper sample collection. “The quality of the semen analysis is dependent on the quality of the sample collection.”
This highlights the need to follow the correct procedure for sample collection.
Laboratory Analysis Methods
After the sample arrives, the lab starts analyzing it. They check sperm count, motility, morphology, and more. Advanced tools and techniques are used to get accurate results.
| Parameter | Method of Analysis | Normal Values |
| Sperm Count | Using a hemocytometer | Above 15 million/mL |
| Sperm Motility | Computer-assisted sperm analysis (CASA) | 40-50% or greater |
| Sperm Morphology | Kruger Strict Criteria | 4% or more |
Timeline for Receiving Sperm Test Results
You usually get your sperm test results in 24 to 72 hours after the lab gets the sample. The exact time depends on the tests done and the lab’s workload.
Getting your spermiogram results is the end of the testing process. It’s important to understand these results to assess your fertility and plan next steps. We’re here to help you interpret your results and address any questions or concerns.
Conclusion: Beyond the Numbers in Spermiogram Analysis
Understanding spermiogram results means looking at the bigger picture. These results are important but must be seen in the context of your overall health and fertility. A healthcare professional’s evaluation is key for accurate interpretation and guidance.
Sperm test results can take 24 to 72 hours to process. This time frame varies based on the lab and the tests needed. Knowing this can help you plan your next steps in your fertility journey.
We at our institution value timely and accurate sperm analysis. Our team is dedicated to top-notch healthcare and support for international patients. By considering your overall health and fertility, we can offer personalized guidance and treatment options.
FAQ
What is a spermiogram, and why is it important for male fertility testing?
A spermiogram, or seminal analysis, is a key test for male fertility. It looks at semen parameters like sperm count, motility, and shape. It’s vital for couples trying to conceive.
What are the World Health Organization reference values for a normal seminal analysis report?
The World Health Organization sets standards for seminal analysis. These include a semen volume of 1.5 mL or more. Also, a sperm concentration of 15 million/mL or more is needed. A total sperm count of 39 million or more per ejaculate is also a benchmark.
How long does it take to receive sperm test results?
Typically, sperm test results are ready in 24 to 72 hours. This depends on the lab and testing methods.
What does a normal sperm count report indicate?
A normal sperm count report suggests good fertility chances. But, sperm motility and morphology are also key for conception.
What is the significance of sperm motility in assessing male fertility?
Sperm motility is vital for fertilization. It lets sperm reach the egg. Normal motility percentages, 40-50% or more, show good fertility.
How is sperm morphology evaluated, and what are the normal criteria?
Sperm morphology is checked using the Kruger strict criteria. It looks at sperm shape and structure. Normal morphology is 4% or more of sperm with a normal shape.
What additional parameters are assessed in a seminal fluid analysis?
Other parameters like sperm vitality, pH, liquefaction time, and white blood cell count are checked. They give insights into semen quality and possible issues like infection or inflammation.
How is a semen sample collected for analysis?
For sample collection, a man masturbates into a sterile container. It’s important to avoid lubricants or substances that could contaminate the sample.
What does a normal seminal fluid analysis report mean for fertility?
A normal seminal fluid analysis report means semen parameters are within normal ranges. This suggests good fertility. Yet, a healthcare professional’s evaluation is needed for accurate interpretation and guidance.
References
World Health Organization. (2025). 7 Key Spermiogram Results What Normal Seminal Analysis. Retrieved from https://www.who.int/publications/i/item/9789240030787