Last Updated on November 27, 2025 by Ugurkan Demir

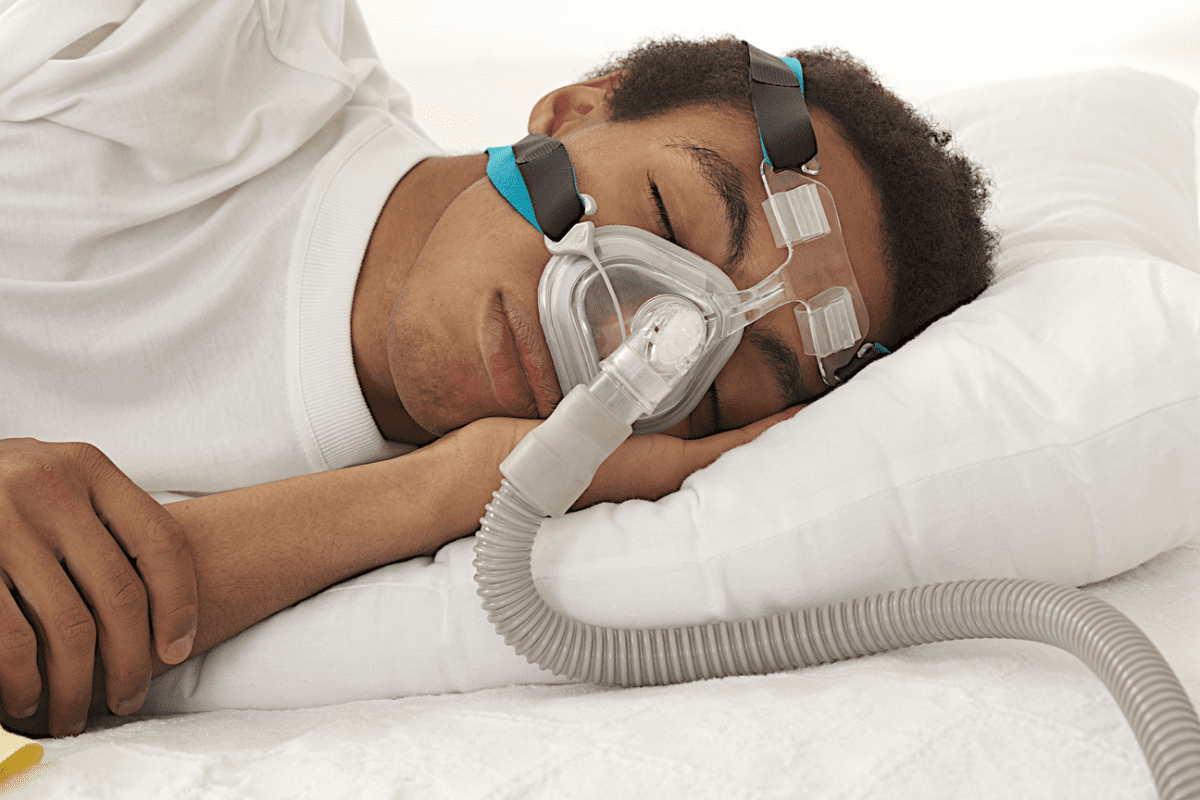
For those with obstructive sleep apnea (OSA), CPAP therapy can be a hassle. Hypoglossal nerve stimulation is a new way to help. It’s a transformative solution for OSA relief.
The Inspire device is a implantable medical device. It treats OSA by stimulating the hypoglossal nerve. This nerve controls tongue movement. It helps you breathe naturally while you sleep, making treatment more comfortable and effective.
At Liv Hospital, we offer this cutting-edge procedure. It’s a great alternative to CPAP therapy for OSA patients. Our team is committed to top-notch healthcare. We also offer full support for international patients.
How to qualify for and receive a surgical implant for sleep apnea (e.g., Inspire hypoglossal nerve stimulation).
Key Takeaways
- Hypoglossal nerve stimulation is a revolutionary treatment for obstructive sleep apnea.
- The Inspire device is an implantable medical device that stimulates the hypoglossal nerve.
- This technology helps restore natural breathing during sleep.
- Liv Hospital offers this innovative procedure with international standards of excellence.
- Our team provides full support for international patients.
Understanding Sleep Apnea and Its Impact
Obstructive sleep apnea (OSA) is a common condition where the airway blocks during sleep. It affects millions, disrupting their sleep and life quality.
Types of Sleep Apnea and Prevalence
Sleep apnea includes several disorders, with OSA being the most common. It happens when the throat muscles relax, blocking the airway. This is why OSA affects about 84% of those with sleep apnea.
Central sleep apnea (CSA) is when the brain fails to control breathing muscles. Complex sleep apnea is a mix of OSA and CSA. Knowing the type is key to finding the right treatment.
Health Consequences of Untreated OSA
Untreated OSA can harm your heart and increase blood pressure. It also leads to daytime tiredness. These sleep breaks can lower blood oxygen, stressing the heart.
Cardiovascular risks from untreated OSA include heart attacks and strokes. It can also worsen diabetes and depression. Getting diagnosed and treated is vital to avoid these risks.
Limitations of Traditional Treatments
CPAP therapy is a common OSA treatment. But, many find it hard to use because of discomfort or claustrophobia. Alternative treatments are needed for those who can’t use CPAP.
Oral appliances and lifestyle changes are other options. But, they might not work for everyone, like those with severe OSA. Surgical implants, like the Inspire device, offer a better solution for some.
Exploring Surgical Implant for Sleep Apnea Options

For those with obstructive sleep apnea (OSA), surgical implants offer hope. One promising treatment is hypoglossal nerve stimulation. It has shown great promise in managing sleep apnea.
Hypoglossal Nerve Stimulation Technology
This technology uses a device to stimulate the hypoglossal nerve. This nerve controls the tongue’s movement. It’s based on the fact that in many OSA patients, the tongue blocks the airway during sleep.
By stimulating the nerve, the device keeps the tongue forward. This keeps the airway open.
The Inspire Device: Components and Mechanism
The Inspire device is a type of hypoglossal nerve stimulator for sleep apnea. It has three parts: a pulse generator, a stimulation lead, and a breathing sensor. The pulse generator is under the skin below the collarbone.
The stimulation lead is near the hypoglossal nerve. The breathing sensor is between the ribs, monitoring breathing.
The device detects when you start to breathe in during sleep. It then stimulates the nerve to move the tongue forward. This prevents the airway from collapsing.
How Tongue Stimulation Prevents Airway Collapse
Tongue stimulation is key in stopping airway collapse. During sleep, the tongue can fall back and block the airway. The Inspire device moves the tongue forward, keeping the airway open.
This not only reduces sleep apnea but also improves sleep quality. Studies have shown the Inspire device’s effectiveness in reducing apnea-hypopnea index (AHI) scores. This means a big improvement in sleep apnea symptoms.
Determining If You’re a Candidate
To see if HGNS is for you, you need to look at your health and medical history. You must meet certain criteria to qualify for HGNS therapy. These criteria show if you could really benefit from this treatment.
Ideal Patient Profile for HGNS
The best fit for HGNS has moderate to severe sleep apnea. They should have tried and failed with CPAP therapy or can’t use it. They’re usually not very overweight and have certain body features that make HGNS a good choice.
Medical Requirements and BMI Considerations
To qualify for HGNS, your health and sleep apnea level must be checked carefully. Your Body Mass Index (BMI) is also key. If your BMI is too high, HGNS might not work as well for you.
Criteria | Ideal Range | Comments |
BMI | Less than 32 | Higher BMI may reduce effectiveness |
AHI (Apnea-Hypopnea Index) | 15-65 | Moderate to severe OSA |
CPAP History | Failed or intolerant | Documented failure or intolerance |
CPAP Failure or Intolerance Documentation
You need proof that CPAP didn’t work for you. This proof is important for insurance and to see if HGNS is a good alternative.
Contraindications for Hypoglossal Nerve Stimulation
Some health issues or body features might make HGNS not suitable. This includes being very overweight, having other devices that could mess with HGNS, or certain brain conditions.
Key Contraindications:
- Significant obesity (BMI ≥ 40)
- Presence of other implanted devices (e.g., pacemakers)
- Neurological conditions affecting the hypoglossal nerve
The Pre-Surgical Evaluation Process
A detailed pre-surgical evaluation is key to finding the right candidates for HGNS therapy. It makes sure patients are a good fit for the treatment. It also helps predict how well the treatment will work.
Initial Consultation with Sleep Specialist
The first step is a meeting with a sleep specialist. We talk about the patient’s health history, sleep issues, and past treatments. This meeting helps us see if HGNS is a good choice for the patient.
Sleep Studies and Severity Assessment
Sleep studies are very important in this process. They show how bad the sleep apnea is and what the patient’s sleep patterns are like. We use this info to see if HGNS is needed.
Drug-Induced Sleep Endoscopy (DISE)
DISE lets us see the airway during sleep. It’s key for figuring out where blockages might be. This helps us decide if HGNS will work well.
Airway Anatomy Evaluation
We also look at the airway’s structure. This helps us understand how HGNS might affect the patient. It lets us make the treatment fit the patient’s needs better.
The pre-surgical evaluation includes several steps:
- Looking at the patient’s medical history
- Doing sleep studies to check OSA severity
- Using DISE to study airway movement
- Examining the airway’s structure
- Reviewing past treatments and their results
By carefully checking each patient’s situation, we can see if HGNS is the best choice. We then create a plan for the best results.
Navigating Insurance and Costs
It’s important to understand insurance coverage for HGNS sleep apnea treatment. The cost can be complex, with many factors affecting the total price and what insurance covers.
Insurance Coverage Requirements
To get insurance, patients must meet certain criteria. They need a diagnosis of moderate to severe sleep apnea. They also must have tried and failed with CPAP therapy and have a sleep study.
Key requirements often include:
- A sleep study to assess the severity of sleep apnea
- Documentation of CPAP failure or intolerance
- A consultation with a sleep specialist
Medicare and Private Insurance Policies
Medicare and many private insurance plans cover HGNS therapy. But, the amount of coverage can differ. Medicare, for example, covers the Inspire device for those who meet certain criteria.
Private insurance policies may have different requirements and coverage levels.
Insurance Provider | Coverage for HGNS | Typical Requirements |
Medicare | Covers Inspire device | Moderate to severe OSA, CPAP failure |
Private Insurers | Varies by policy | Comprehensive sleep study, CPAP intolerance |
Out-of-Pocket Expenses
Even with insurance, patients may face out-of-pocket costs. These can include deductibles, copays, and costs for pre-surgical evaluations.
Patients should be prepared for expenses such as:
- Deductibles and copays for doctor visits and procedures
- Costs for sleep studies and other diagnostic tests
- Potential costs for device adjustments and follow-up care
Financial Assistance Programs
For those struggling financially, there are help programs available. These can make HGNS therapy more affordable.
Patients should ask about financial help with their healthcare provider or insurance company.
Preparing for Your Hypoglossal Nerve Stimulator Surgery
Getting ready for your hypoglossal nerve stimulator implant is a big step. Your healthcare team will guide you through important steps. This ensures a smooth and successful surgery.
Pre-Surgical Consultations and Testing
You’ll have many consultations and tests before surgery. These help check your health and if you’re right for the implant. Your team will look at your medical history and do exams.
They might also do sleep studies or airway checks. It’s key to talk about any worries or questions you have. Your team will explain the risks, benefits, and what to expect after.
Medical Clearance Requirements
Getting medical clearance is a big step before HGNS surgery. Your team will check your health to spot any risks. This might include:
- Looking at your current meds and health issues
- Doing blood tests or other exams
- Checking your heart health
This ensures you’re safe and have the best chance for success.
Medication Adjustments Before Surgery
Some meds might need to change or stop before surgery. Your doctor will look at your meds, like:
- Blood thinners
- Anti-inflammatory drugs
- Medicines that could affect bleeding or healing
It’s important to follow your doctor’s advice on meds. This keeps you safe during and after surgery.
Day-of-Surgery Instructions
Following your healthcare team’s instructions on the day of surgery is key. They might tell you to:
Instruction | Description |
Fasting Requirements | Avoid eating or drinking for a set time before surgery |
Medication Timing | Take some meds with a little water as told |
Arrival Time | Get to the hospital or surgical center on time |
By following these instructions, you help make your surgery and recovery go well.
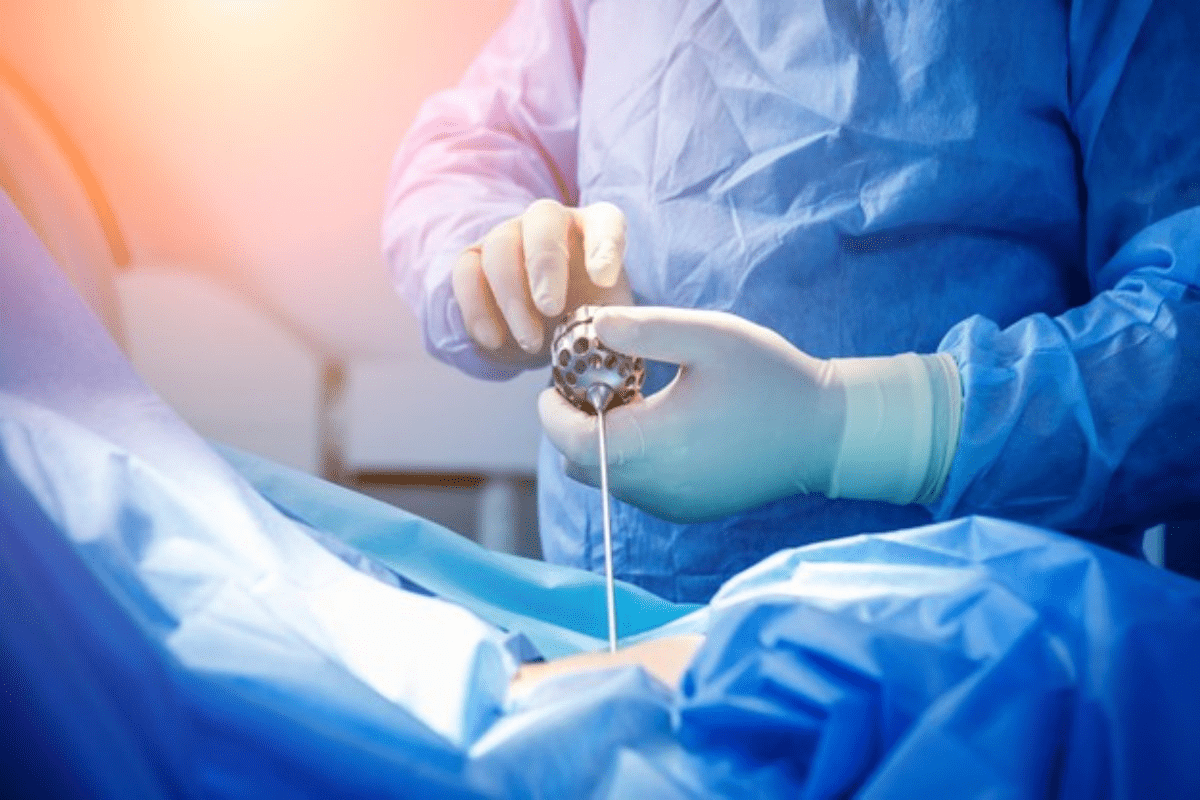
The Surgical Implantation Procedure
Getting the Inspire device implanted is a surgery done under general anesthesia. This keeps the patient comfortable during the operation.
Anesthesia and Surgical Approach
An experienced anesthesiologist and skilled surgeon perform the surgery. They work together to make sure it’s safe and effective. Small incisions are made to put in the device’s parts.
Key aspects of the surgical approach include:
- Minimally invasive techniques to reduce recovery time
- Precise placement of device components for optimal functionality
- Careful consideration of the patient’s anatomy to ensure compatibility with the device
Placement of the Three Main Components
The Inspire device has three main parts: the neurostimulator, the breathing detection lead, and the stimulation lead. Each part is placed carefully during surgery.
Component | Placement | Function |
Neurostimulator | Upper chest area | Generates the stimulation signal |
Breathing Detection Lead | Near the diaphragm | Monitors breathing patterns |
Stimulation Lead | Under the tongue | Stimulates the hypoglossal nerve to keep the airway open |
Typical Duration and Hospital Stay
The surgery usually takes about 90 minutes. After, patients often stay overnight in the hospital for recovery and observation.
“The surgical implantation of the Inspire device is a procedure that has been refined over years to ensure the highest level of safety and efficacy for patients with sleep apnea.”
Understanding Surgical Scars and Placement
Like any surgery, the Inspire device implantation leaves scars. But the incisions are small and in less noticeable areas.
Scarring worries are normal. Our surgical team works hard to make scars as small as possible. They also make sure scars don’t affect the device’s work or the patient’s comfort.
Recovery and Device Activation Timeline
Overcoming sleep apnea with HGNS surgery takes a journey. It includes a recovery process and a timeline for device activation. Knowing what to expect can make your experience better and lead to good results.
Immediate Post-Operative Care
Right after surgery, patients might feel a bit sore. This is managed with pain meds. We focus on post-operative care to help you recover well. This means watching for infection signs, managing pain, and following wound care steps.
Key aspects of immediate post-operative care include:
- Resting well to heal
- Eating soft foods to avoid discomfort
- Staying away from hard activities
Healing Process and Activity Restrictions
Healing times differ for everyone, but most can get back to normal in a few weeks. Yet, some activities might be off-limits for longer to help the device heal right.
Activity | Recommended Restriction Period |
Strenuous Exercise | 4-6 weeks |
Heavy Lifting | 4-6 weeks |
Contact Sports | 8-12 weeks |
One-Month Activation Appointment
About a month after surgery, you’ll come back for device activation. We turn on the HGNS device and start adjusting it to the right levels.
Titration and Adjustment Period
After activation, there’s a titration and adjustment phase. We tweak the device settings to find the best therapy with the least side effects.
Titration process includes:
- Watching sleep patterns and device performance
- Changing stimulation levels as needed
- Dealing with any side effects or concerns
Knowing the recovery and device activation timeline helps you prepare. It ensures a successful HGNS therapy journey.
Clinical Outcomes and Effectiveness Data
Hypoglossal Nerve Stimulation is a promising treatment for Obstructive Sleep Apnea. It has strong clinical data backing it. Studies show it improves sleep apnea severity and quality of life.
Short-Term Results
In the first 12 months, HGNS therapy shows big improvements. About 47% of patients have AHI values below 5 events per hour. This means a big drop in sleep apnea severity.
Long-Term Effectiveness
After three years, HGNS keeps showing its worth. It keeps managing sleep apnea well. There are few reports of serious side effects.
AHI Reduction Statistics
Reducing AHI is key to HGNS’s success. Studies show HGNS cuts AHI, improving sleep quality. It also lowers the risk of sleep apnea problems.
Timeframe | Mean AHI Reduction | Percentage of Patients with AHI |
12 Months | Significant reduction | 47% |
3 Years | Sustained reduction | Maintained improvement |
Quality of Life and Symptom Improvements
HGNS therapy also boosts quality of life and symptom reduction. Patients see better sleep, less daytime fatigue, and better overall health.
The evidence for HGNS in treating Obstructive Sleep Apnea is strong. It shows benefits both short-term and long-term. HGNS is a valuable treatment option for those who qualify.
Conclusion: Making an Informed Decision About Sleep Apnea Surgery
Thinking about sleep apnea surgery, like Hypoglossal Nerve Stimulation (HGNS), is a big step. It’s important to make an informed decision that fits your situation and how bad your Obstructive Sleep Apnea (OSA) is.
Patients need to think about their past treatments, what HGNS can do for them, and the risks. Talking to doctors is key to finding the right treatment for you.
Knowing about HGNS and sleep apnea surgery helps you choose the best option. This way, you can make a choice you’re sure about.
Choosing HGNS surgery means looking at your health needs and listening to your doctors. It’s a careful decision that should be made with the right information.
FAQ
What is a hypoglossal nerve stimulator, and how does it work?
A hypoglossal nerve stimulator, like the Inspire device, is a device implanted to treat sleep apnea. It works by stimulating the hypoglossal nerve. This nerve controls the tongue. The stimulation helps keep the airway open during sleep.
How is the Inspire device implanted, and what are the components?
The Inspire device is implanted through surgery. It has three main parts. A stimulation lead is placed near the hypoglossal nerve. A sensing lead is put between the ribs to monitor breathing. The generator is placed in the upper chest. Together, they help keep the airway open.
What are the benefits of hypoglossal nerve stimulation (HGNS) compared to CPAP therapy?
HGNS offers better comfort and less sleep disruption than CPAP therapy. It also lets you sleep in any position. It’s more effective for those who can’t tolerate CPAP or have complex sleep apnea.
Who is a suitable candidate for hypoglossal nerve stimulation?
Good candidates for HGNS have moderate to severe sleep apnea. They should have trouble with CPAP or failed CPAP therapy. They must also meet certain medical requirements, like a specific BMI and no certain medical conditions.
What is the pre-surgical evaluation process for HGNS?
The pre-surgical process starts with a consultation with a sleep specialist. You’ll have sleep studies to check your sleep apnea. You’ll also have a drug-induced sleep endoscopy (DISE) to look at your airway. Other tests will check if you’re a good candidate for HGNS.
How do I navigate insurance coverage and costs associated with HGNS?
To understand insurance coverage, learn what your policy requires. Check if Medicare or private insurance covers HGNS. You can also estimate costs and look for financial help.
What are the steps involved in preparing for HGNS surgery?
Preparing for surgery includes pre-surgical tests and consultations. You’ll get medical clearance and adjust your medications. Follow the instructions for the day of surgery.
What can I expect during the surgical implantation procedure for the Inspire device?
During surgery, you’ll get anesthesia. The surgeon will implant the device’s parts. The procedure takes a few hours. You might stay in the hospital overnight.
What is the recovery process like after HGNS surgery?
The recovery involves immediate care and a healing period of several weeks. You’ll need to follow activity restrictions. You’ll also have a one-month appointment to turn on the device.
How effective is HGNS in treating obstructive sleep apnea?
Studies show HGNS reduces apnea-hypopnea index (AHI) scores. It improves quality of life and symptoms in sleep apnea patients. Clinical data support HGNS as a treatment option.
Are there any potentially risks or complications associated with HGNS?
Like any surgery, HGNS has risks, such as infection and device malfunction. Tongue weakness is also a risk. But, the benefits often outweigh the risks for suitable candidates.
Can I use CPAP therapy if I have HGNS surgery?
While HGNS is an alternative to CPAP, some might use CPAP too. The goal of HGNS is to reduce or eliminate CPAP use.
How do I know if I’m a good candidate for the Inspire device?
To see if you’re a good candidate, talk to a healthcare professional. They’ll assess your situation and medical history. They can determine if HGNS is right for you.
References
National Center for Biotechnology Information. (2025). How to Get a Surgical Implant for Sleep. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29758185/