Chronic kidney disease (CKD) affects millions globally. Stage 2 kidney disease shows a kidney function rate between 60 and 89. This means your kidneys are working a bit less than they should.
In this stage, your kidneys have some damage. You might also see signs like albuminuria, high creatinine levels, or other issues. It’s important to know about CKD stage 2 to keep your kidneys healthy.
We’ll look into what Stage 2 CKD is, its early signs, and how to treat it. Knowing about this condition helps you take steps to slow down or stop it from getting worse.
When someone is diagnosed with Stage 2 chronic kidney disease (CKD), it’s key to know what it means for their kidneys. This stage shows mildly decreased kidney function, with an estimated glomerular filtration rate (eGFR) between 60-89 mL/min. It’s a critical point where kidney damage is present but symptoms may not be obvious.
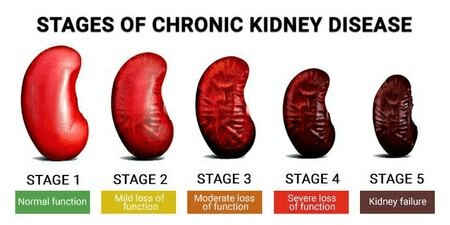
CKD is divided into five stages, with Stage 1 being the least severe and Stage 5 indicating kidney failure. This system helps doctors understand the extent of kidney damage and plan the right treatment.
The stages are defined as follows:
CKD Stage | eGFR Range (mL/min) | Kidney Function Level |
Stage 1 | 90 or above | Normal kidney function |
Stage 2 | 60-89 | Mildly decreased kidney function |
Stage 3 | 30-59 | Moderately decreased kidney function |
Stage 4 | 15-29 | Severely decreased kidney function |
Stage 5 | Less than 15 | Kidney failure |
An eGFR between 60-89 mL/min shows that the kidneys are not working at their best. This range means there’s mild kidney damage, and more tests and monitoring are needed.
Early signs of kidney damage include albuminuria (protein in the urine) and other subtle signs. Regular check-ups and screenings are vital for catching these signs early.
Some early signs of kidney problems include:
Knowing these signs can help manage CKD better and slow its progression.
To diagnose Stage 2 CKD, doctors use blood tests, urine analyses, and imaging studies. These tools help doctors check how well the kidneys work and spot any damage.
The estimated Glomerular Filtration Rate (eGFR) is key in diagnosing CKD. It shows how well the kidneys filter waste from the blood. If the eGFR is between 60-89 mL/min, it means the kidneys are not working as well as they should.
eGFR Calculation: Doctors use a formula to figure out the eGFR. This formula looks at the patient’s age, sex, and serum creatinine levels. It gives a better idea of kidney function than just serum creatinine.
Albuminuria, or albumin in the urine, is a sign of kidney damage. Urine tests can find albuminuria, helping doctors diagnose CKD.
Imaging tests like ultrasound, CT scans, or MRI scans help find problems in the kidneys. They can spot issues like kidney stones, cysts, or tumors.
The table below shows the main ways doctors diagnose Stage 2 CKD:
Diagnostic Method | Purpose | Key Findings |
eGFR Blood Test | Measures kidney function | eGFR between 60-89 mL/min |
Urine Albumin-to-Creatinine Ratio (ACR) | Detects albuminuria | Presence of albumin in urine |
Imaging Tests (Ultrasound, CT, MRI) | Identifies structural abnormalities | Kidney damage or disease |
Stage 2 Kidney Disease can be caused by diabetes and hypertension. These conditions harm the kidneys if not managed well.
Diabetes is a top cause of kidney disease. High blood sugar damages kidney blood vessels, making them less effective. Managing diabetes well can lower this risk.
Those with diabetes face a higher risk of kidney disease. It’s important to keep blood sugar and kidney function in check.
Hypertension, or high blood pressure, also causes Stage 2 Kidney Disease. It strains kidney blood vessels, reducing function. Controlling hypertension is key to avoiding kidney damage.
High blood pressure damages kidney blood vessels, impairing function. Managing hypertension is essential to stop kidney disease from getting worse.
While diabetes and hypertension are common causes, other conditions can also harm kidneys. These include glomerulonephritis, polycystic kidney disease (PKD), and genetic disorders. Knowing about these conditions is important for good care.
Other factors like certain medications, toxins, and infections can also harm kidneys. Being aware of these risks helps protect kidney health.
Stage 2 Kidney Disease often goes unnoticed because it progresses quietly. Many people with Stage 2 CKD don’t know they have it. This is because symptoms usually show up later.
Stage 2 CKD means a moderate drop in kidney function. But, it usually doesn’t cause obvious symptoms. The kidneys can handle a lot before problems show up.
Even though many with Stage 2 CKD don’t show symptoms, some might notice small signs. These include:
These signs can also mean other health issues. So, getting a proper diagnosis is key.
Telling kidney disease symptoms from others can be tricky. For example, swelling can happen for many reasons, not just kidney problems. Always see a doctor for a correct diagnosis.
If you notice unusual symptoms or have risk factors like diabetes or high blood pressure, see a doctor. Early treatment can help slow CKD’s progress.
Key indicators that warrant medical evaluation include:
Knowing these signs and getting medical help early can help manage kidney health. This might slow Stage 2 CKD’s progress.
CKD progression is a complex process. It is influenced by many risk factors, some of which can be changed. Knowing these factors is key to managing the disease effectively.
Genetics play a big role in CKD progression. People with a family history of kidney disease are at higher risk. Family history suggests a genetic link, making early screening and monitoring vital.
Certain medical conditions can speed up kidney damage. These include diabetes, hypertension, and heart diseases. It’s important to manage these conditions well to slow CKD progression.
Medical Condition | Impact on CKD | Management Strategy |
Diabetes | High blood sugar damages kidney filters | Blood sugar control, regular monitoring |
Hypertension | High blood pressure strains kidneys | Blood pressure management, lifestyle changes |
Cardiovascular Disease | Increased risk of kidney damage | Heart health management, lifestyle modifications |
Age, race, and demographic factors also affect CKD progression. Older adults and some racial or ethnic groups are at higher risk. Knowing these demographic risks helps tailor preventive measures.
While some risk factors like genetics and age can’t be changed, others like lifestyle choices and medical conditions can be managed. Focusing on modifiable risk factors can greatly impact CKD progression.
Understanding and addressing CKD progression risk factors is key. Healthcare providers and patients can work together. This way, they can slow disease progression and improve outcomes.
Stage 2 CKD treatment aims to control blood pressure and manage underlying conditions. It also uses specific medications to slow the disease’s progression. A complete treatment plan is needed to tackle both the disease and its causes.
Keeping blood pressure in check is key to slowing CKD. We suggest using certain medications that work well for CKD patients.
ACE Inhibitors and ARBs are often prescribed for CKD. They relax blood vessels, helping the heart pump blood better and reducing kidney pressure.
Research shows ACE inhibitors and ARBs can slow kidney disease in CKD patients.
It’s vital to manage conditions like diabetes and hypertension in Stage 2 CKD. We stress the need for lifestyle changes and medications to control these conditions.
New treatments for CKD are being researched, including novel medications and therapies. These aim to slow disease progression and improve outcomes.
Research focuses on anti-fibrotic agents and inflammation modulators. These could be future treatment options.
Keeping up with the latest in CKD treatment helps us provide the best care for Stage 2 CKD patients.
Living with Stage 2 CKD means making smart food choices. A kidney-friendly diet can greatly improve your health. It helps control the disease and slow its progress.
It’s important to cut down on sodium to keep blood pressure and fluid balance in check. We advise eating less than 2,300 milligrams of sodium daily. Processed and packaged foods are high in sodium, so always check the labels.
The American Heart Association suggests eating no more than 2,300 milligrams of sodium a day. They say cutting down to 1,500 milligrams can help even more with blood pressure.
Protein is essential, but too much can harm the kidneys. Talk to a healthcare provider or dietitian to find out how much protein is right for you. A moderate amount is usually best.
Keeping potassium and phosphorus levels in check is vital as kidney disease worsens. Foods high in these nutrients, like bananas and dairy, should be eaten in moderation. Working closely with your healthcare team is important to find the right balance.
Choosing the right foods can make a big difference. Stick to whole, unprocessed foods like vegetables, fruits, whole grains, lean proteins, and healthy fats.
Making smart food choices can help manage Stage 2 CKD. It can also improve your overall quality of life.
Lifestyle changes are key in slowing down chronic kidney disease. By making healthy choices, people with Stage 2 Kidney Disease can slow down their disease.
Exercise is vital for those with kidney disease. It helps control blood pressure and keeps the heart healthy. Aim for 150 minutes of moderate exercise each week.
Benefits of Exercise for CKD Patients:
Smoking speeds up kidney disease. Quitting can greatly reduce this risk. We suggest getting help from doctors or smoking cessation programs.
The benefits of smoking cessation include:
Keeping a healthy weight is essential for kidney disease management. Extra weight strains the kidneys and worsens conditions like high blood pressure and diabetes. A balanced diet and regular exercise help maintain a healthy weight.
Weight Management Strategies | Benefits |
Balanced diet | Improved overall nutrition |
Regular physical activity | Enhanced weight loss and maintenance |
Monitoring calorie intake | Better control over weight |
Chronic stress harms kidney health by raising blood pressure and leading to unhealthy habits. Techniques like meditation, yoga, or deep breathing can help.
By making these lifestyle changes, people with Stage 2 Kidney Disease can manage their condition better. They might even slow down its progression.
Tracking your kidney health is key to slowing Stage 2 Kidney Disease. Regular checks help spot changes early. This lets you act fast to slow the disease.
How often you need kidney tests depends on your health and other conditions. People with Stage 2 CKD should get tested yearly. But, your doctor might want you to test more often if you have other health issues.
“Regular checks are vital for managing kidney disease,” says a top nephrologist. “Tracking key lab values helps patients and doctors adjust treatment plans together.”
Two important lab values are eGFR and albuminuria. eGFR shows how well your kidneys filter waste. Albuminuria means your kidneys might be damaged.
Digital tools are great for keeping an eye on your kidney health. Mobile apps and online platforms track lab results and more. They help patients and doctors make better choices.
Knowing the signs of CKD getting worse is important. Look out for fatigue, swelling, and changes in how you pee. If you notice these, see your doctor right away.
By staying informed and active in monitoring your kidney health, you can manage Stage 2 CKD well. This improves your overall health.
Having a strong kidney care team is key for those with Stage 2 CKD. It helps them manage their condition well. A team of healthcare professionals works together to care for you.
Primary care doctors are vital in catching and treating kidney disease early. They are usually the first doctors you see. They:
Your primary care doctor will help manage your health. They will also work with other specialists as needed.
A nephrologist is a kidney specialist. You might see one if:
Nephrologists offer expert care. They create a treatment plan to slow disease and manage symptoms.
Other specialists might join your care team. This includes:
A team of specialists ensures your health is fully cared for. This gives you complete care.
Talking well with your healthcare team is key for managing CKD. Here’s how:
By working with your team and talking openly, you can manage your condition better. This improves your life quality.
The future for people with Stage 2 kidney disease looks different for everyone. Knowing what affects it is key to managing it well and living a good life.
How fast Stage 2 CKD gets worse can vary a lot. Things like health, lifestyle, and treatment plans matter a lot. With the right care, many can stay in Stage 2 for years without getting worse.
It’s important to keep an eye on your kidneys and change treatments as needed. Working with your doctor to monitor your health is a must.
Many things can affect how well someone with Stage 2 CKD does in the long run. These include:
Working on these areas early on can really help. By managing health issues and living a healthy lifestyle, you can slow down the disease and improve your life.
Keeping a good quality of life with CKD takes effort. It means following a special diet, staying active, and managing stress.
What you eat is very important. Eating less salt, controlling protein, and watching potassium and phosphorus can help slow the disease and avoid problems.
CKD can affect your mind and feelings too. It’s important to deal with these as part of your care plan. Support from doctors, family, and groups can really help.
Talking about your feelings with your healthcare team is a good idea. They can offer the support and advice you need to handle the emotional side of CKD.
By understanding your future and taking steps to manage Stage 2 CKD, you can keep a good quality of life. This also helps prevent the disease from getting worse.
Managing stage 2 kidney disease is key to slowing it down and keeping healthy. Knowing about the disease, following treatment plans, and changing lifestyle habits can make a big difference. This helps improve health outcomes.
Dealing with CKD requires a team effort. It includes keeping an eye on kidney health, managing blood pressure, and eating right. It’s vital to work with doctors to create a care plan that fits you.
Being proactive in kidney health can lower the risk of serious problems. Early action and treatment are essential for managing stage 2 kidney disease well.
We aim to give people the tools and knowledge to handle their CKD. This way, we can all work towards better health and well-being for those with stage 2 kidney disease.
Stage 2 Kidney Disease, also known as Stage 2 Chronic Kidney Disease (CKD), is a condition where the kidneys are damaged. This damage affects how well they work. It’s when the kidneys lose some function but not too much.
It’s marked by an estimated Glomerular Filtration Rate (eGFR) between 60-89 mL/min. This shows a slight drop in kidney function.
Many people with Stage 2 CKD don’t show any symptoms. But, some might feel tired, have swelling, or notice changes in how they urinate.
Doctors use tests to find Stage 2 CKD. These include eGFR, albuminuria, and imaging tests. They help check how well the kidneys are working and if they’re damaged.
The main reasons for Stage 2 CKD are diabetes, high blood pressure, and other diseases that harm the kidneys.
Managing Stage 2 CKD needs a detailed plan. This includes controlling blood pressure, treating other health issues, following a special diet, and making lifestyle changes. These changes include staying active, quitting smoking, and keeping a healthy weight.
To manage Stage 2 CKD, you should eat less sodium, watch your protein intake, and control potassium and phosphorus levels. It’s also important to choose foods that are good for your kidneys.
How often you check your kidney health depends on your situation. But, it’s good to get regular tests, track important lab values, and use digital health tools. This helps spot any changes or signs of the disease getting worse.
The outlook for Stage 2 CKD varies. It depends on the cause, other health issues, and how well you manage and treat it. With the right care, you can slow the disease and keep a good quality of life.
You should see a nephrologist if you have Stage 2 CKD, or if you have a family history of kidney disease, diabetes, or high blood pressure. A nephrologist can give you specialized care and advice on taking care of your kidneys.
Yes, making lifestyle changes can help slow CKD. These include staying active, quitting smoking, managing your weight, and reducing stress.
Finding and treating Stage 2 CKD early can slow the disease, lower the risk of complications, and improve your life quality.
Preventing Chronic Kidney Disease – https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd/prevention
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us