Last Updated on December 1, 2025 by Bilal Hasdemir
Neuroblastoma is a rare form of cancer that primarily affects children, with approximately 1 in every 7,000 diagnosed, mostly in those under the age of 5. It starts in nerve tissue and often begins in the adrenal glands. When it spreads, treatment gets harder and outcomes can be worse.
Neuroblastoma metastasis is a big worry in pediatric oncology. Knowing where it spreads is key to planning treatment.
Key Takeaways
- Neuroblastoma is a rare cancer mainly found in young children.
- It starts in nerve tissue and can begin in any part of the sympathetic nervous system.
- Metastasis makes treatment harder and can affect how well a patient does.
- Knowing where it spreads is important for good treatment plans.
- Neuroblastoma spreading is a big issue in pediatric oncology.
Understanding Neuroblastoma: A Complete Overview
Neuroblastoma is a cancer that comes from immature nerve cells. It’s a big challenge in treating kids with cancer. We’ll look at what it is, where it comes from, how common it is, and where it usually starts.
Definition and Origin of Neuroblastoma
Neuroblastoma is a cancer that starts from immature nerve cells, called neuroblasts. These cells are found in many parts of the body, often in the adrenal glands. These cells are early versions of nerve cells and are present in the fetus. In neuroblastoma, these cells don’t grow up and instead form tumors.
Incidence and Demographics
Neuroblastoma is a rare cancer, making up about 6% of all childhood cancers. It mostly hits kids under 5, with most cases in kids under 1. It’s a bit more common in boys than girls. Here’s some data to help us understand who gets it:
| Age Group | Incidence Rate |
| 0-1 year | Higher incidence |
| 1-5 years | Most common |
| >5 years | Less common |
Primary Sites of Neuroblastoma
Neuroblastoma can start in any part of the sympathetic nervous system. This includes the adrenal glands, neck, chest, and pelvis. The most common place is the adrenal gland, which sits on top of the kidney. It can also start in the neck, chest, and pelvis, along the sympathetic nerve chains.
Knowing where neuroblastoma starts helps us understand how complex it is. It shows why we need to treat it in a detailed way.
The Metastatic Process in Neuroblastoma
The metastatic process in neuroblastoma is complex. It involves interactions between cancer cells and the body’s systems. This process is key to cancer progression and affects treatment and prognosis.
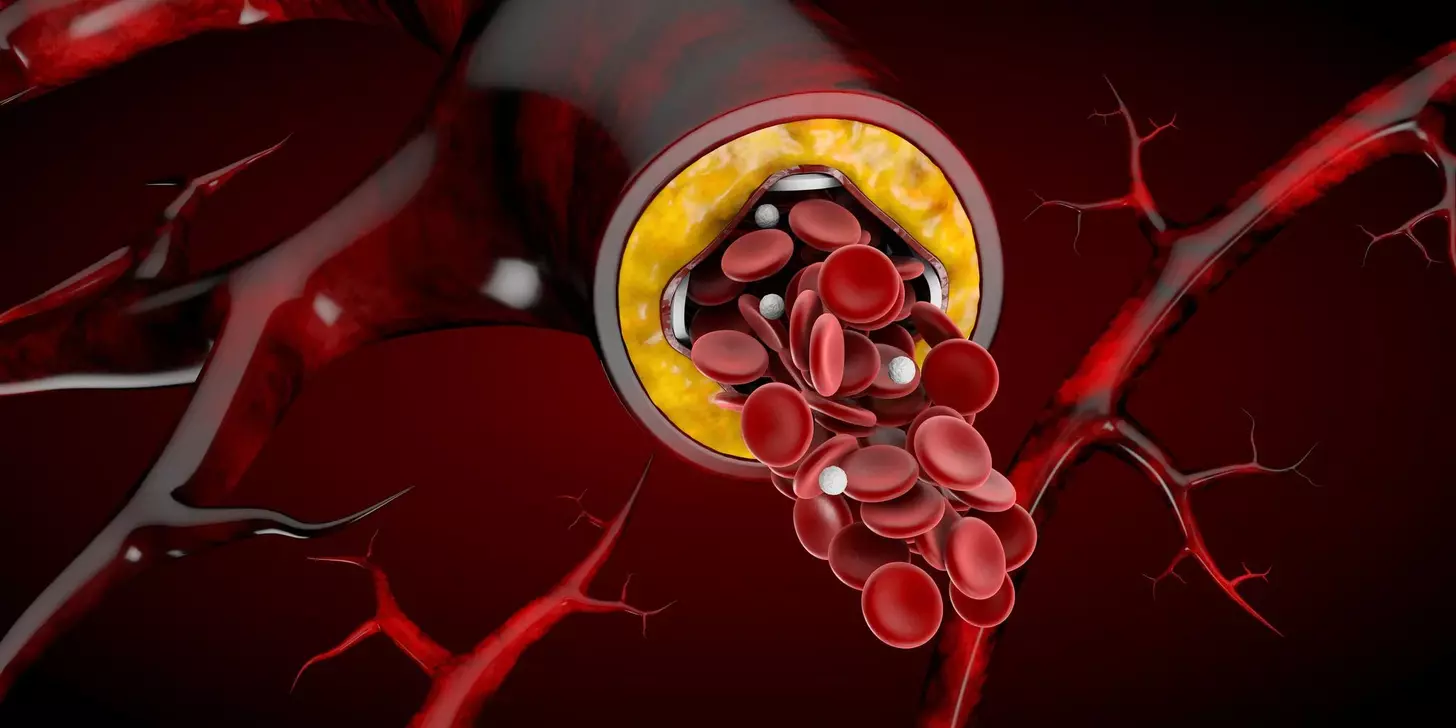
How Cancer Cells Spread
Cancer cells can break away from the primary tumor. They spread to other parts of the body through the bloodstream or lymphatic system. This involves steps like invasion, circulation, and colonization at distant sites. Understanding these mechanisms is key for developing targeted therapies.
The spread of cancer cells is not random. It involves complex biological processes. These processes help cancer cells evade the immune system and establish new tumor sites.
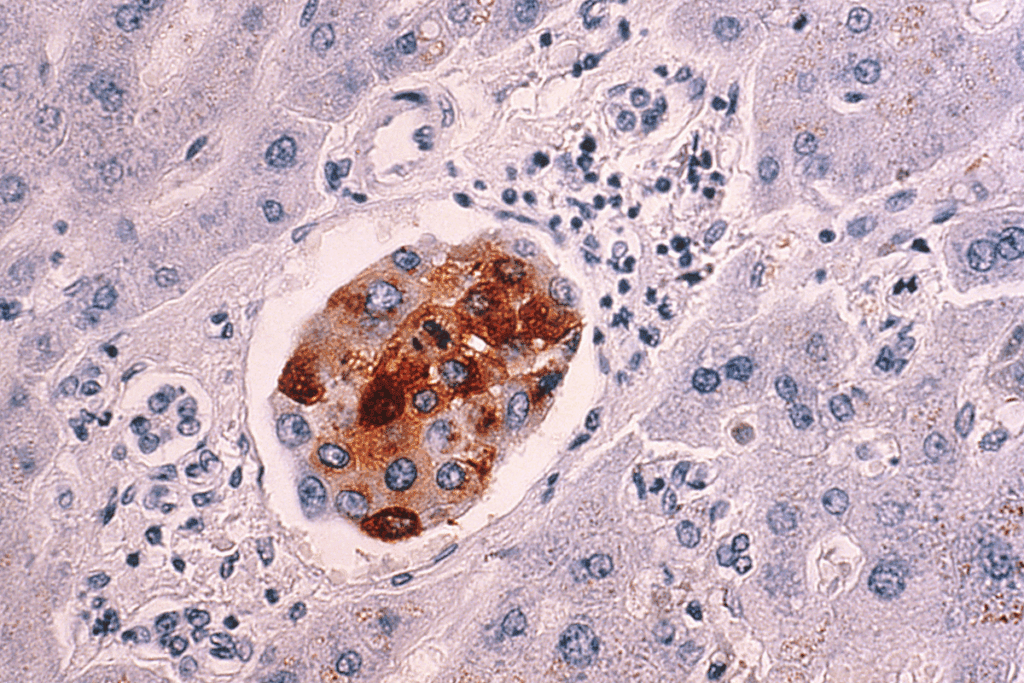
Unique Characteristics of Neuroblastoma Metastasis
Neuroblastoma metastasis has unique features. It often spreads to specific sites like the bone marrow, bones, lymph nodes, and liver. The pattern of metastasis can influence the clinical presentation and prognosis.
Genetic and molecular characteristics of neuroblastoma, such as MYCN amplification, also play a role. Understanding these factors is vital for risk stratification and treatment planning.
Common Sites of Metastatic Neuroblastoma
Metastatic neuroblastoma often affects many areas, each with its own challenges. Knowing these common sites is key to managing and treating the disease effectively.
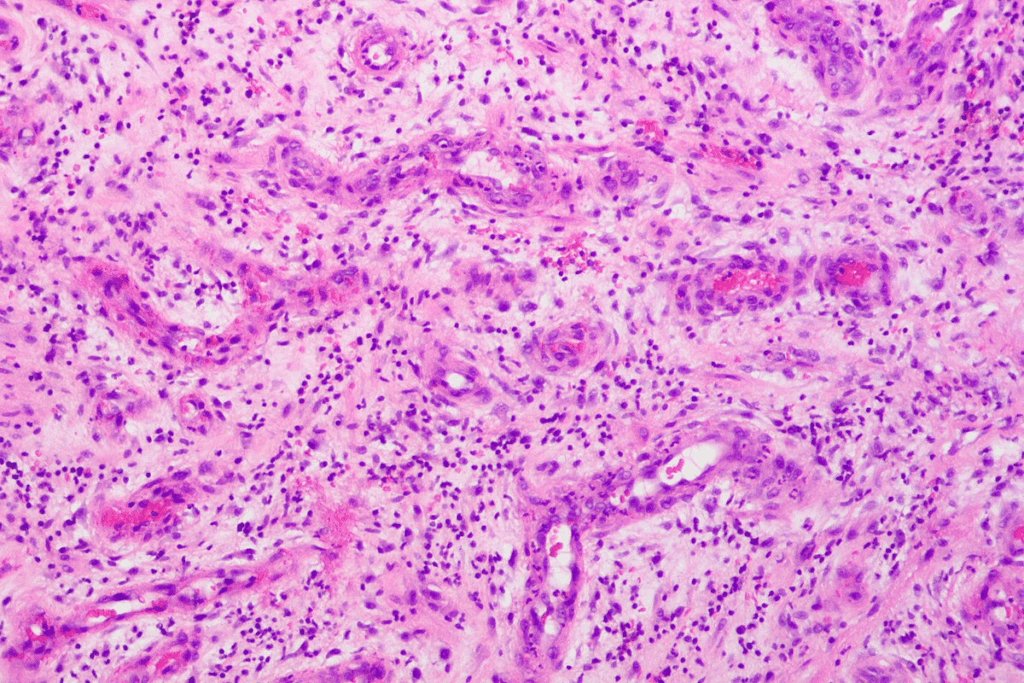
Bone Marrow Involvement
Bone marrow involvement is a common problem with neuroblastoma. It happens when cancer cells get into the bone marrow. This can lower blood cell production, causing anemia, infections, and bleeding issues.
Symptoms indicative of bone marrow involvement include fatigue, pallor, and an increased frequency of infections. Doctors use bone marrow aspiration and biopsy to diagnose it.
Bone Metastases
Bone metastases are another common issue. Cancer cells can damage bones, causing pain, fractures, and high calcium levels.
Having bone metastases means the disease is likely in a more advanced stage. It needs aggressive treatment.
Lymph Node Spread
Lymph node involvement is common in metastatic neuroblastoma. Cancer cells can go to nearby or distant lymph nodes, making them swollen and painful.
Doctors check for lymph node spread through imaging and biopsies. This helps figure out how far the disease has spread.
Liver Metastases

Liver metastases are more common in young children and infants. They can cause the liver to grow big and not work right.
Liver involvement is checked with ultrasound, CT, or MRI scans.
| Metastatic Site | Common Symptoms | Diagnostic Methods |
| Bone Marrow | Fatigue, infections, bleeding | Bone marrow aspiration and biopsy |
| Bones | Pain, fractures, hypercalcemia | Imaging studies (X-ray, CT, MRI) |
| Lymph Nodes | Enlarged lymph nodes, pain | Imaging studies, lymph node biopsy |
| Liver | Hepatomegaly, liver dysfunction | Ultrasound, CT, MRI scans |
Less Common Metastatic Sites
Neuroblastoma can spread to several important areas, not just bones, bone marrow, and lymph nodes. These other locations are less common but play a big role in how the disease progresses.
Central Nervous System Metastases
CNS metastases in neuroblastoma are rare but very serious. CNS involvement can cause a lot of problems and needs quick diagnosis and treatment. We will look into the challenges of diagnosing and treating CNS metastases.
Even though CNS metastases are rare, they show the disease is getting worse. Early detection is key to managing them well.
Lung Involvement
Lung metastases from neuroblastoma are rare but can happen, mainly in advanced stages. Lung involvement might cause breathing problems, and doctors use imaging to find it.
We will talk about how to recognize and treat lung metastases in neuroblastoma. It’s important to use a combination of treatments.
Other Rare Sites
Neuroblastoma can also spread to the liver, pancreas, and skin, though it’s rare. These rare metastases bring their own set of challenges for diagnosis and treatment.
We will discuss the impact of these rare sites and the specific treatments needed for them.
Diagnosing Metastatic Neuroblastoma
To diagnose metastatic neuroblastoma, doctors use a detailed method. They look at the first symptoms, use advanced imaging, and run lab tests. We’ll dive into these steps to see how they help in finding the right treatment.
Initial Symptoms of Metastatic Disease
Initial symptoms of metastatic neuroblastoma can vary significantly among individuals. Common signs are bone pain, fatigue, and weight loss. Some might see proptosis (bulging eyes) or periorbital ecchymosis (bruising around the eyes) if the tumor spreads to the orbits.
“Symptoms can include a lump in the neck, chest, or abdomen, and in some cases, patients may experience neurological symptoms if the tumor compresses or invades nearby structures.”
Imaging Techniques
Imaging studies are key in diagnosing metastatic neuroblastoma. The most used methods are:
- CT scans: Give detailed images of the body, showing the main tumor and how far it has spread.
- MRI: Provides clear images of soft tissues, helping to see if the tumor has reached the spinal cord or other important areas.
- PET scans: Use a radioactive tracer to show where tumors are by highlighting areas of high activity.
Laboratory Tests and Biomarkers
Lab tests are vital for confirming the diagnosis and seeing how far the disease has spread. Important tests include:
- Urine catecholamines: High levels of certain catecholamines in the urine can point to neuroblastoma.
- Bone marrow biopsy: Examines bone marrow samples for cancer cells, which is key for staging and diagnosing.
- Blood tests: May check lactate dehydrogenase (LDH) and other biomarkers to see how big the tumor is.
By using these diagnostic methods together, doctors can accurately diagnose metastatic neuroblastoma. They can then create a treatment plan that fits the patient’s specific needs.
Staging Systems for Neuroblastoma
Staging systems for neuroblastoma help doctors understand how far the disease has spread. They also look at the risk factors of the tumor. Knowing this helps doctors predict how well a patient will do and what treatment to use.
International Neuroblastoma Staging System (INSS)
The International Neuroblastoma Staging System (INSS) is a key tool for classifying neuroblastoma. It looks at how far the disease has spread and if it can be removed by surgery. The INSS divides neuroblastoma into stages, from small, local tumors to tumors that have spread far.
| INSS Stage | Description |
| Stage 1 | Localized tumor with complete gross excision |
| Stage 2 | Localized tumor with incomplete gross excision |
| Stage 3 | Unresectable unilateral tumor or contralateral tumor |
| Stage 4 | Distant metastatic disease |
| Stage 4S | Localized primary tumor with dissemination limited to skin, liver, or bone marrow in infants |
International Neuroblastoma Risk Group (INRG) Classification
The International Neuroblastoma Risk Group (INRG) Classification is another important tool. It looks at clinical and biological risk factors to group patients by risk. The INRG system uses imaging and biological markers to predict outcomes.
The INRG classification is great for finding high-risk patients. It helps doctors plan more intense treatments for them. It also helps in making treatment plans that fit each patient’s needs.
Both the INSS and INRG systems are vital in managing neuroblastoma. They help doctors tailor treatments to each patient’s situation.
Genetic and Molecular Factors Influencing Metastasis
Understanding the genetic factors that influence neuroblastoma metastasis is key to finding effective treatments. The genetic makeup of neuroblastoma greatly affects its ability to spread.
MYCN Amplification
MYCN amplification is a known genetic marker for aggressive neuroblastoma. Tumors with MYCN amplification are often diagnosed at a later stage and have a worse prognosis. This marker is vital in deciding treatment plans.
ALK Mutations
ALK mutations also play a role in neuroblastoma behavior. These mutations activate pathways that help tumors grow and spread. Thanks to ALK mutations, targeted therapies have been developed, giving hope to high-risk patients.
Other Genetic Markers
Other markers like 11q deletion and 17q gain are also important in neuroblastoma. These genetic changes can affect how likely a tumor is to spread and guide treatment choices.
Using genetic and molecular information in treating neuroblastoma is a big step forward. We’re moving towards treatments that are tailored to each patient’s tumor, based on genetic profiles.
Treatment Approaches for Metastatic Neuroblastoma
For metastatic neuroblastoma, a mix of treatments works best. This method uses different ways to fight the disease all at once.
Multimodal Treatment Strategy
Using many treatments together is key for metastatic neuroblastoma. This mix includes surgery, chemotherapy, and radiation therapy. It helps tackle the disease’s complex nature.
We make each treatment plan special for each patient. We consider how far the disease has spread, the patient’s genes, and their health.
Surgery for Metastatic Disease
Surgery is very important in treating metastatic neuroblastoma. It helps remove the main tumor and any other disease spots. The goal is to remove as much of the tumor as possible.
Sometimes, surgery comes after chemotherapy. This makes the tumor smaller and easier to remove.
Radiation Therapy
Radiation therapy is a big part of treating metastatic neuroblastoma. It focuses on specific disease areas, like the main tumor or spots in bones or organs.
We use new radiation methods, like IMRT, to hit the disease hard. This way, we protect the healthy parts around it.
Chemotherapy Protocols
Chemotherapy is a mainstay in treating metastatic neuroblastoma. We use a mix of drugs to attack cancer cells well.
The drugs and how strong the treatment is depend on the patient’s risk, age, and health.
Advanced Therapies for High-Risk Metastatic Neuroblastoma
Advanced therapies are bringing new hope to those with high-risk metastatic neuroblastoma. We’re seeing a big change in how we treat this disease. New methods aim to increase survival rates and improve life quality.
Anti-GD2 Immunotherapy
Anti-GD2 immunotherapy is key in fighting high-risk neuroblastoma. It targets the GD2 antigen found on neuroblastoma cells. This therapy uses the immune system to kill cancer cells, lowering the chance of it coming back.
Clinical trials have shown promising results. Patients who got anti-GD2 immunotherapy did better and lived longer.
Retinoic Acid Therapy
Retinoic acid therapy is another advanced treatment for high-risk neuroblastoma. It makes neuroblastoma cells less aggressive and easier to treat. Studies have shown it improves results when used with other treatments like chemotherapy and immunotherapy.
Emerging Targeted Therapies
Targeted therapies are getting better fast, with new agents being tested for high-risk metastatic neuroblastoma. These therapies aim at specific cancer growth drivers. Early trials are showing good signs, opening doors for more research and possible use in standard treatments.
We’re hopeful about the future of treating high-risk metastatic neuroblastoma. The ongoing development of advanced therapies is vital. It will help improve patient outcomes and fight this tough disease better.
Clinical Trials and Research Advancements
Research is making big strides in understanding neuroblastoma. New clinical trials are exploring fresh ways to treat it. This change is thanks to ongoing research and trials.
Current Clinical Trials
Many clinical trialsare looking into new treatments for neuroblastoma. These include immunotherapy and targeted therapy. shows many studies are recruiting or underway. They’re focusing on:
- Immunotherapy: Using the immune system to fight neuroblastoma cells.
- Targeted Therapy: Creating treatments that target specific genetic mutations in neuroblastoma.
- Combination Therapies: Testing how combining different treatments can improve results.
Promising Research Directions
The future of treating neuroblastoma is bright. Several promising areas are being explored. These include:
- Personalized Medicine: Creating treatments based on each patient’s unique genetic profile.
- Novel Immunotherapeutic Approaches: Finding new ways to boost the immune system against neuroblastoma.
- Targeting Cancer Stem Cells: Working on strategies to target the main cause of neuroblastoma’s return and spread.
These advancements highlight the need for more research and funding in neuroblastoma treatment. As we progress, we can expect neuroblastoma care to keep evolving. This brings new hope to patients and their families.
Long-term Monitoring and Follow-up Care
Long-term care is key for neuroblastoma survivors. It helps doctors watch for signs of the disease coming back and handle treatment side effects. As we get better at treating neuroblastoma, more people are living longer. So, caring for them long-term is more critical than ever.
Surveillance for Recurrence
Regular checks are essential to catch recurrence early. We suggest a plan of regular visits, scans, and blood tests. This plan is based on the patient’s risk and treatment history. It might include:
- Periodic imaging studies such as MRI or CT scans
- Blood tests to monitor tumor markers
- Bone marrow examinations if necessary
Being watchful helps us spot problems early. This makes it easier to treat them effectively.
Managing Late Effects of Treatment
Neuroblastoma treatment can affect a patient’s health for a long time. We aim to manage these effects to improve their quality of life. Common late effects include:
- Hearing loss due to certain chemotherapy agents
- Growth and developmental issues
- Increased risk of secondary cancers
We use a team of experts to care for these effects. This team includes audiologists, endocrinologists, and oncologists. We also teach patients and their families how to watch their health and know when to seek help.
By focusing on long-term care, we can greatly improve the health and survival of neuroblastoma survivors.
Prognosis and Survival Rates for Metastatic Neuroblastoma
The outlook for metastatic neuroblastoma changes a lot. It depends on several important things. These include the age when the disease is found, how far it has spread, and what the tumor is like.
Factors Affecting Prognosis
Many things can change how likely someone is to survive metastatic neuroblastoma. Age at diagnosis is very important. Kids who are younger usually do better than older ones.
The stage of the disease also matters a lot. If the disease is more advanced, the chances of survival are lower.
What the tumor’s biology is like can also affect the outcome. For example, MYCN amplification and ALK mutations make tumors grow faster. This means they need more intense treatment.
| Prognostic Factor | Favorable | Unfavorable |
| Age at Diagnosis | <18 months | >18 months |
| MYCN Status | Non-amplified | Amplified |
| ALK Mutation Status | Wild-type | Mutated |
Long-term Survival Statistics
Thanks to new treatments, more kids with metastatic neuroblastoma are living longer. Now, about 50-60% of kids with high-risk neuroblastoma survive for 5 years.
We keep watching survival rates to learn more about the disease. This helps us find new ways to help kids fight it.
Conclusion
Understanding neuroblastoma metastasis is key to helping patients with this childhood cancer. We’ve looked at how it spreads, how doctors diagnose it, and the treatments available.
Managing neuroblastoma metastasis needs a team effort. This includes surgery, radiation, and chemotherapy. New treatments like anti-GD2 immunotherapy and retinoic acid therapy also help high-risk patients.
Families dealing with neuroblastoma need support. Organizations focused on childhood cancer research and support offer important help. We suggest that patients and their families check out these resources to help them through their journey.
FAQ
What is neuroblastoma and how does it metastasize?
Neuroblastoma is a childhood cancer that starts in neuroblasts. These cells are usually found in the adrenal glands, neck, chest, or pelvis. It spreads to other parts of the body like bone marrow, bones, lymph nodes, and liver. This happens through the bloodstream or lymphatic system.
What are the common sites of metastatic neuroblastoma?
Common places for metastatic neuroblastoma include bone marrow, bones, lymph nodes, and liver. Symptoms like bone pain, anemia, or swelling in the abdomen can occur at these sites.
How is metastatic neuroblastoma diagnosed?
Doctors use imaging like MRI or CT scans and lab tests to diagnose metastatic neuroblastoma. These tests include biopsy and biomarker analysis. Symptoms like bone pain or weight loss might lead to further tests.
What are the treatment options for metastatic neuroblastoma?
Treatment for metastatic neuroblastoma often involves surgery, radiation, and chemotherapy. For high-risk patients, treatments like anti-GD2 immunotherapy and retinoic acid therapy might be used.
What is the prognosis for metastatic neuroblastoma?
The outlook for metastatic neuroblastoma varies. It depends on the disease stage, age at diagnosis, and genetic factorslike MYCN amplification. Thanks to new treatments, survival rates have improved. But, more research is needed to keep improving outcomes.
What are the genetic and molecular factors that influence metastasis in neuroblastoma?
Genetic and molecular factors, like MYCN amplification and ALK mutations, are key. They help determine the risk of metastasis and how well a patient will respond to treatment.
What is the role of clinical trials in neuroblastoma treatment?
Clinical trials are vital for finding new treatments for neuroblastoma. They help test promising therapies, including targeted treatments and immunotherapy.
How is long-term follow-up care managed for neuroblastoma survivors?
Survivors of neuroblastoma need regular check-ups to watch for recurrence and manage treatment side effects. This includes organ damage or secondary cancers.
What are the current research advancements in neuroblastoma treatment?
New research is focused on targeted therapies, immunotherapy, and precision medicine. These approaches aim to improve outcomes for patients with high-risk neuroblastoma.
Where can I find more information and support for neuroblastoma?
We offer detailed support and resources for neuroblastoma patients. This includes information on treatments, clinical trials, and long-term care. Our team is committed to providing top-notch care with compassion and expertise.
Reference
- Henderson, T. O., Bhatia, S., Pinto, N., London, W. B., McGrady, P., Crotty, C., & Cohn, S. L. (2022). Contemporary survival and prognostic factors in children with neuroblastoma. Journal of Clinical Oncology, 40(6), 608–620. https://pubmed.ncbi.nlm.nih.gov/34932776