Last Updated on December 1, 2025 by Bilal Hasdemir
The outlook for children with neuroblastoma is influenced by several key factors.
We will dive into the details of neuroblastoma. This includes its stages, treatment choices, and how these impact a child’s life expectancy. Knowing these things helps families deal with the tough parts of this diagnosis life expectancy neuroblastoma child.
Key Takeaways
- Neuroblastoma survival rates vary significantly based on age and stage at diagnosis.
- Treatment response plays a critical role in determining life expectancy.
- Recent advancements in treatment have improved survival rates for some patients.
- Understanding the factors that influence life expectancy can help families cope with the diagnosis.
- Early detection and proper treatment are key to better outcomes.
Understanding Neuroblastoma in Children

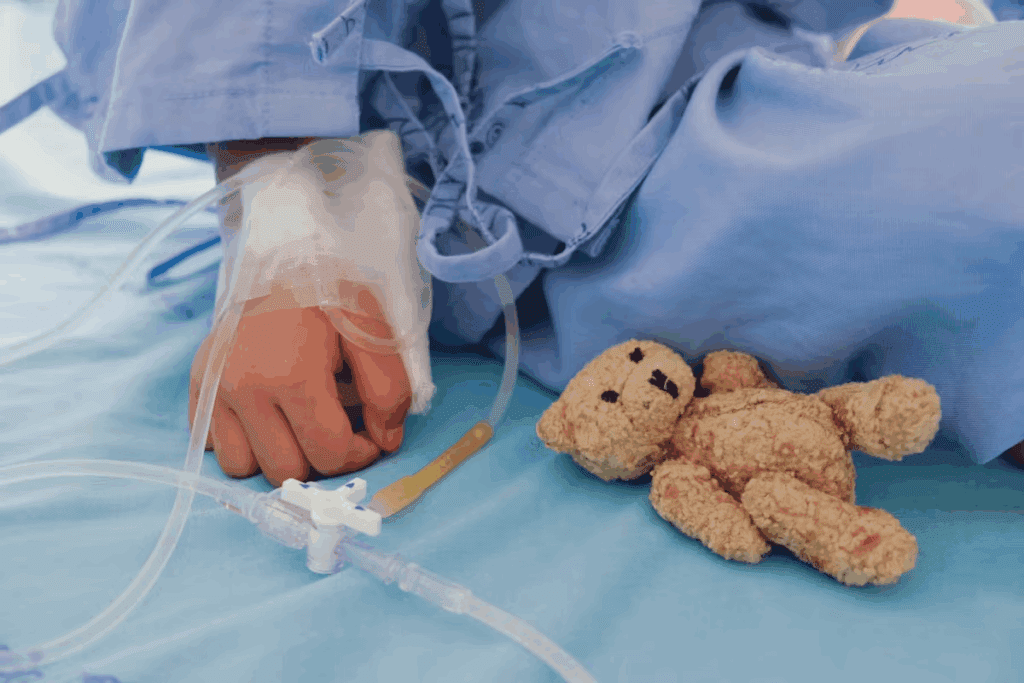
Neuroblastoma is a rare cancer that affects young kids, mostly under five. It starts from immature nerve cells. It often begins in the adrenal glands, neck, chest, or spinal cord. Knowing about neuroblastoma helps families and caregivers deal with diagnosis and treatment.
Definition and Origin of Neuroblastoma
Neuroblastoma comes from neuroblasts, young nerve cells. These cells are part of the nervous system that controls body functions like heart rate and digestion. The exact cause is unknown, but it’s thought to be due to genetic mutations causing these cells to grow out of control.
Incidence and Demographics
Neuroblastoma is the most common cancer in infants and the third most common in kids. It’s most common in children under one. About 700 new cases are diagnosed in the U.S. each year. It’s slightly more common in boys than girls.
Common Symptoms and Presentation
Symptoms vary based on where the tumor is and if it has spread. Common signs include a lump in the neck, chest, or belly, proptosis (bulging eyes), and changes in bowel or bladder habits. It can also cause paralysis or weakness if it presses on nerves or the spinal cord. Spotting these symptoms early is key for timely treatment.
It’s vital for parents and caregivers to know these signs. Recognizing them early can greatly improve treatment outcomes and the prognosis for kids with neuroblastoma.
Diagnosis and Staging of Neuroblastoma

Diagnosing neuroblastoma requires imaging studies, biopsy, and molecular tests. These steps help find out how far the disease has spread. Knowing this is key to understanding the prognosis and planning treatment.
Diagnostic Procedures and Tests
Several tests are used to find neuroblastoma, including:
- Imaging Studies: Ultrasound, CT scans, MRI, and MIBG scans show the tumor’s size and spread.
- Biopsy: A biopsy removes a tumor sample for lab tests to confirm the diagnosis.
- Molecular Testing: Tests like MYCN amplification analysis reveal the tumor’s genetic makeup.
The International Neuroblastoma Staging System (INSS)
The INSS is a staging system for neuroblastoma. It classifies the disease based on its extent and how easily the tumor can be removed. The stages go from 1 (localized) to 4 (distant metastasis), with a special stage 4S for infants.
The International Neuroblastoma Risk Group (INRG) Classification
The INRG Classification helps predict neuroblastoma risk. It looks at age, stage, tumor type, and genetic factors like MYCN status. This helps doctors choose the right treatment intensity.
Understanding neuroblastoma diagnosis and staging is vital for effective treatment. By using diagnostic tests and staging systems, we can predict outcomes better. This helps improve survival rates for children with neuroblastoma.
Risk Factors Affecting Life Expectancy Neuroblastoma Child
The outlook for children with neuroblastoma is influenced by several key factors. Knowing these factors helps doctors plan the best treatment and guess how long a child might live.
Age at Diagnosis
How old a child is when they get diagnosed matters a lot. Infants under 18 months usually have a better chance of beating the disease than older kids. This is because their disease is often less severe.
Younger kids are more likely to get better on their own or with less harsh treatments. Older kids, on the other hand, often need stronger treatments because their disease is more aggressive.
Tumor Biology and Genetic Markers
The type of tumor and certain genetic markers are also key. Tumor histology, or how the tumor cells look under a microscope, tells doctors a lot about the disease’s aggressiveness.
Genetic features like DNA ploidy and specific mutations also affect the prognosis. For example, tumors with near-triploid or triploid DNA content usually have a better outlook.
MYCN Amplification and Its Impact
MYCN amplification is a genetic marker linked to high-risk neuroblastoma. It means the disease is likely to be more aggressive and have a worse prognosis.
Kids with MYCN-amplified tumors need more aggressive treatments, like high-dose chemotherapy and immunotherapy. Scientists are working hard to understand how MYCN amplification affects treatment results and find new ways to fight the disease.
By knowing about age, tumor biology, and genetic markers like MYCN amplification, doctors can predict life expectancy better. They can then create personalized treatment plans for kids with neuroblastoma.
Neuroblastoma Survival Rates: An Overview
The outlook for children with neuroblastoma is influenced by several key factors.e and how far the cancer has spread. Knowing these factors is key for patients and their families.
Understanding Survival Statistics
Survival stats for neuroblastoma show the 5-year survival rates. These rates tell us what percent of patients live for 5 years after being diagnosed. They come from big groups of patients and give a general idea of what to expect.
It’s important to remember that these rates don’t predict what will happen to one person. But they help us understand the chances of survival based on past data. New treatments have made survival rates better, so it’s good to look at the latest numbers when thinking about the future.
5-Year Survival Rates
The outlook for children with neuroblastoma is influenced by several key factors.
| Age at Diagnosis | Stage | 5-Year Survival Rate |
| Infants ( | Low-risk | 95-100% |
| Children (>18 months) | High-risk | 40-50% |
| Children (>18 months) | Low-risk | 80-90% |
Long-Term Survival Considerations
While 5-year survival rates are helpful, long-term survival is also very important. Long-term survival means living 10, 20, or more years after being diagnosed. For neuroblastoma, how well the first treatment works, if any cancer is left behind, and treatment side effects all play a role.
We’re seeing more kids living longer after being diagnosed with neuroblastoma, thanks to younger ages and lower-risk disease. Research and new treatments are helping us understand neuroblastoma better and improve patient outcomes.
Neuroblastoma Survival by Stage
Survival rates for neuroblastoma change a lot based on the stage at diagnosis. The stage of the disease is key in figuring out the prognosis and treatment plan. We’ll look at survival rates by stage, giving insights into each stage’s prognosis.
Stage 1 and 2 Survival Rates
Patients with stage 1 or 2 neuroblastoma have high survival rates. The 5-year survival rate for stage 1 is over 95%, and for stage 2, it’s around 90-95%. These stages are low-risk, with the disease often being localized. This makes removing the tumor through surgery very effective.
Stage 3 Survival Rates
Stage 3 neuroblastoma is considered intermediate to high-risk. The 5-year survival rate for stage 3 is between 70-80%. Treatment for stage 3 includes chemotherapy, surgery, and radiation therapy.
Stage 4 Survival Rates
Stage 4 neuroblastoma is the toughest to treat. The 5-year survival rate for older children with stage 4 is 40-50%. This stage means the disease has spread to distant parts of the body. Treatment is intense, including high-dose chemotherapy and stem cell transplantation.
Stage 4S Survival Rates
Stage 4S neuroblastoma is a special case, mainly in infants under 1 year old. Despite having metastatic disease, stage 4S has a good prognosis. Survival rates are over 80-90%. Many infants with stage 4S neuroblastoma see their tumors shrink on their own.
Knowing survival rates by stage helps patients and families make better care choices. While stage is important, age, tumor biology, and treatment response also affect the prognosis.
Age-Related Prognosis in Pediatric Neuroblastoma
The outlook for children with neuroblastoma is influenced by several key factors.e. Knowing how age impacts the disease is key for making treatment plans and giving families the right info.
Infants Under 18 Months
Infants under 18 months usually have a better chance of beating neuroblastoma. Their tumors often change into less harmful types on their own. So, doctors try to use gentler treatments to avoid long-term side effects.
Favorable Outcomes in Infants:
- Higher rate of spontaneous regression
- More responsive to less intensive treatments
- Better overall survival rates compared to older children
Children Over 18 Months
Kids over 18 months face a tougher fight against neuroblastoma. Their tumors are more aggressive and harder to treat. Doctors use stronger treatments like chemo, surgery, and radiation to fight the disease.
Challenges in Older Children:
- More aggressive tumor behavior
- Higher risk of treatment resistance
- Need for more intensive treatment protocols
Adolescents and Young Adults
Neuroblastoma in teens and young adults is rare and has its own challenges. It can be very aggressive and hard to treat. Doctors aim to find treatments that work well but also avoid long-term side effects.
| Age Group | Prognosis Characteristics | Typical Treatment Approaches |
| Infants (<18 months) | Favorable tumor biology, higher spontaneous regression | Less intensive therapies, observation |
| Children (>18 months) | More aggressive tumors, unfavorable markers | Intensive chemotherapy, surgery, radiation |
| Adolescents/Young Adults | Rare, potentially aggressive, distinct clinical features | Multimodal treatment, clinical trials |
As shown in the table, age is a big factor in neuroblastoma treatment. Knowing these differences helps doctors tailor treatments and gives families a clear idea of what to expect.
Treatment Approaches and Their Impact on Survival
Treatment for neuroblastoma often includes surgery, chemotherapy, radiation, and stem cell transplants. The choice of treatment depends on the disease stage, patient age, and tumor characteristics.
Surgery
Surgery is key in treating neuroblastoma, mainly for localized cases. The goal is to remove the tumor fully. Studies show that removing the tumor completely can greatly improve survival chances in low-risk cases (1).
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. It’s often used with other treatments. Chemotherapy can shrink tumors, making them easier to remove surgically. The choice of drugs depends on the tumor’s risk level.
Radiation Therapy
Radiation therapy kills cancer cells with high-energy rays. It’s useful after surgery or for advanced cases. Radiation therapy helps control the disease and improve survival in high-risk cases (2).
Stem Cell Transplantation
Stem cell transplantation replaces damaged bone marrow. This treatment allows for more intense therapy, which is key for curing high-risk neuroblastoma. Studies show it can boost survival rates in these patients (3).
A study in the Journal of Clinical Oncology found a higher 5-year survival rate for high-risk neuroblastoma patients who got stem cell transplants. This compared to those who got conventional chemotherapy (4).
| Treatment Modality | Role in Neuroblastoma Treatment | Impact on Survival |
| Surgery | Removal of primary tumor | Improves survival in low-risk disease |
| Chemotherapy | Systemic treatment to reduce tumor size | Enhances survival when combined with other treatments |
| Radiation Therapy | Treatment of residual disease or palliation | Improves local control and survival in high-risk disease |
| Stem Cell Transplantation | Replacement of bone marrow after intensive therapy | Improves survival outcomes in high-risk neuroblastoma |
“The integration of multiple treatment modalities has revolutionized the care of neuroblastoma patients, providing better outcomes and hope for long-term survival.”
In conclusion, treating neuroblastoma involves a team effort using various treatments. Understanding each treatment’s role helps healthcare providers tailor care. This approach improves survival chances for children with neuroblastoma.
Immunotherapy and Targeted Treatments for Neuroblastoma
Immunotherapy has changed how we treat neuroblastoma, bringing hope to patients and families. It uses the body’s immune system to fight cancer. This is a more focused approach than old treatments.
Anti-GD2 Immunotherapy is a key area in neuroblastoma treatment. It targets the GD2 antigen on neuroblastoma cells. This helps the immune system find and kill cancer cells better.
Anti-GD2 Immunotherapy
Anti-GD2 immunotherapy has shown great promise in trials, mainly for high-risk neuroblastoma patients. Dinutuximab is an anti-GD2 antibody approved for high-risk neuroblastoma. It’s often used with other treatments to boost its effect.
ALK Inhibitors and Other Targeted Therapies
Other targeted therapies are also being studied for neuroblastoma. ALK inhibitors target the ALK gene, which can be mutated in some cases. These drugs have shown promise in treating ALK-positive neuroblastoma.
Impact on Survival Outcomes
Immunotherapy and targeted treatments are improving survival rates for neuroblastoma patients. These therapies offer more personalized and effective treatments. Ongoing research will help us use these treatments better.
Looking ahead, immunotherapy neuroblastoma and targeted treatments neuroblastoma will be key in fighting this disease. By improving our use of these therapies, we aim to better the lives of those affected by neuroblastoma.
High-Risk Neuroblastoma: Life Expectancy and Treatment Challenges
High-risk neuroblastoma is a tough disease that needs strong treatments. It’s aggressive and has a poor outlook, needing many treatments.
Defining High-Risk Disease
High-risk neuroblastoma includes stage 4 patients, those over 18 months old, and those with MYCN amplification. Knowing these risk factors helps doctors plan treatments.
Doctors group neuroblastoma by risk based on age, stage, and biology. High-risk cases often have advanced stages and bad biology.
Current Survival Statistics
Survival rates for high-risk neuroblastoma are getting better thanks to new treatments. But, there’s a big chance of relapse.
| Risk Group | 5-Year Survival Rate |
| High-Risk | 50-60% |
| Stage 4 | 40-50% |
These numbers show the tough fight against high-risk neuroblastoma. We need more research and better treatments.
Treatment Intensification Strategies
Treatment for high-risk neuroblastoma includes lots of chemotherapy, surgery, radiation, and immunotherapy. New targeted and immunotherapy options are showing promise.
Anti-GD2 immunotherapy has helped high-risk patients live longer. Other treatments like ALK inhibitors are also being used, based on the tumor’s genetics.
As we learn more about high-risk neuroblastoma, we’re getting closer to better treatments. This brings hope for better lives for these patients.
Neuroblastoma Remission Rates and Recurrence Risk
Knowing the chances of remission and recurrence is key for families dealing with neuroblastoma. Remission is a big win in treatment, but the chance of it coming back is a worry, mainly for those at high risk.
Complete and Partial Remission
Remission in neuroblastoma means no or fewer tumor cells after treatment. Complete remission means no tumor cells at all. Partial remission means a big drop, but not all, tumor cells are gone. The chance of getting to complete remission depends on the risk group at diagnosis.
“The main goal of treatment is to get to complete remission,” “But, the risk of it coming back is high, even in high-risk cases. This shows why we must keep a close eye on patients.”
Recurrence Rates by Risk Group
Recurrence rates differ a lot between risk groups. Low-risk patients usually have a lower chance of it coming back than high-risk ones. Studies show that low-risk neuroblastoma has a recurrence rate under 5%. High-risk patients face a 20% to 50% chance of it coming back.
| Risk Group | Recurrence Rate |
| Low-Risk | <5% |
| Intermediate-Risk | 5-15% |
| High-Risk | 20-50% |
Monitoring During and After Treatment
Keeping a close eye on patients during and after treatment is key to catch any signs of recurrence early. This includes regular scans and checks of tumor markers. The monitoring plan depends on the patient’s risk level and treatment.
Understanding remission and recurrence is essential in fighting neuroblastoma. By staying informed and teaming up with healthcare providers, families can face the challenges of neuroblastoma better.
Long-Term Effects and Quality of Life for Survivors
Surviving neuroblastoma brings its own set of challenges. These include physical, cognitive, and psychological late effects. As survival rates rise, tackling these issues becomes more critical.
Physical Late Effects
Neuroblastoma survivors face various physical late effects from their treatment. These can include:
- Hearing loss from certain chemotherapy agents
- Cardiac issues from anthracycline exposure
- Endocrine problems, like thyroid dysfunction or growth hormone deficiency
- Secondary cancers, though rare, are a risk
Regular follow-up care is key to spotting and managing these effects early.
Cognitive and Psychological Impacts
Neuroblastoma and its treatment can also affect survivors’ minds and emotions. These impacts may include:
- Cognitive problems, like memory or concentration issues
- Emotional challenges, such as anxiety or depression
- Social and behavioral issues, often seen in children who were treated young
Early support and intervention can lessen these effects and enhance survivors’ quality of life.
Monitoring and Follow-up Care
Comprehensive follow-up care is vital for neuroblastoma survivors. This includes:
- Regular check-ups with healthcare providers to monitor for late effects
- Screening tests, like hearing tests or cardiac evaluations, as needed
- Supportive care services, including psychological counseling or educational support
Through thorough and ongoing care, we can help survivors overcome their challenges and improve their long-term outcomes.
Supporting Families Through the Neuroblastoma Journey
Families with children facing neuroblastoma need a lot of support. They must deal with the shock and overwhelm of a diagnosis. This journey is complex and involves many challenges.
Coping with Diagnosis and Treatment
Dealing with a neuroblastoma diagnosis is tough. It requires emotional, psychological, and informational help. Families find support in:
- Emotional Support: Counseling and therapy to handle the emotional shock.
- Informational Resources: Reliable info on neuroblastoma, treatment, and what to expect.
- Community Support: Meeting other families who’ve been through similar experiences.
Resources and Support Networks
There are many resources for families, including:
- Support Groups: Places where families can share and get support.
- Educational Materials: Books, websites, and brochures with detailed neuroblastoma info.
- Professional Counseling: Trained therapists for stress and emotional challenges.
Discussing Prognosis with Children
Talking about prognosis with kids is very sensitive. It’s important to be honest but also consider their age and understanding:
- Age-Appropriate Information: Share info that fits the child’s level of understanding.
- Reassurance: Let the child know they are loved and help is being done.
- Ongoing Support: Be ready to answer questions and offer comfort.
With the right support, families can face the neuroblastoma journey better. They can be more resilient and hopeful.
Future Directions in Neuroblastoma Treatment and Outcomes
Neuroblastoma research is on the verge of a breakthrough. Ongoing clinical trials and precision medicine are bringing new hope. We’re moving towards treatments that are more targeted and effective.
Promising Clinical Trials
Several clinical trials are showing great promise in treating neuroblastoma. These trials are looking at new ways to fight the disease. They include:
- Immunotherapy Combinations: Testing how combining different immunotherapies can boost anti-tumor effects.
- Targeted Therapies: Studying the safety and effectiveness of treatments that target specific molecular pathways in neuroblastoma.
- Precision Medicine Approaches: Tailoring treatments based on each patient’s tumor genetics.
Precision Medicine Approaches
Precision medicine is changing how we treat neuroblastoma. It allows for more personalized and effective care. By studying a patient’s tumor genetics, doctors can find the best treatments.
This approach not only improves treatment results but also lowers the risk of side effects.
Some key precision medicine methods include:
- Genetic Profiling: Detailed genetic analysis to find mutations that can be targeted.
- Targeted Therapy: Using drugs that target specific genetic changes in the tumor.
- Biomarker-Driven Treatment: Using biomarkers to predict how well a patient will respond to treatment.
Improving Long-term Survival Rates
Improving survival rates for neuroblastoma patients is a major goal. Research and clinical trials are working on better treatments. These aim to increase survival while reducing side effects and improving quality of life.
Some strategies for better survival include:
- Risk Stratification: Identifying high-risk patients for more intense treatment.
- Treatment Intensification: Using high-dose chemotherapy and stem cell transplantation for high-risk patients.
- Survivorship Care: Providing ongoing care to manage late effects and improve long-term outcomes.
Conclusion
The outlook for children with neuroblastoma is influenced by several key factors.
FAQ
What is neuroblastoma, and how does it affect children?
Neuroblastoma is a cancer that starts in the adrenal glands or nerve tissue. It mainly affects kids. Symptoms can include a swollen belly, bone pain, and trouble breathing, depending on the tumor’s size and where it is.
How is neuroblastoma diagnosed and staged?
Doctors use CT scans, MRI, and MIBG scans to find the cancer. They also do biopsies. The International Neuroblastoma Staging System (INSS) or the International Neuroblastoma Risk Group (INRG) Classification helps figure out how serious it is.
What factors influence the life expectancy of a child with neuroblastoma?
Several things matter, like how old the child is, the tumor’s type, and genetic markers like MYCN amplification. The disease’s stage also plays a big role. Young kids and those with low-risk disease usually do better.
What are the current survival statistics for neuroblastoma?
The 5-year survival rate for neuroblastoma changes based on the stage and risk group. While survival rates have gone up, high-risk neuroblastoma is harder to treat and has lower survival rates.
How does the stage of neuroblastoma impact survival rates?
As the stage gets higher, survival rates go down. Kids with Stage 1 and 2 have better chances. But, Stage 4, and high-risk neuroblastoma, have lower survival rates. Stage 4S sometimes gets better on its own.
What is the impact of age on neuroblastoma prognosis?
Younger kids, under 18 months, usually have a better chance of beating the disease. Older kids and young adults face different challenges and outcomes because of the tumor’s biology and how well it responds to treatment.
What treatment approaches are used for neuroblastoma, and how do they impact survival?
Doctors use surgery, chemotherapy, radiation, and stem cell transplants to treat neuroblastoma. Immunotherapy and targeted treatments are also used, mainly for high-risk cases, to help improve survival chances.
What are the long-term effects experienced by neuroblastoma survivors?
Survivors might face physical issues like hearing loss or growth problems. They could also have cognitive or psychological effects. Getting ongoing care is key to managing these issues and improving their quality of life.
How can families cope with a neuroblastoma diagnosis and treatment?
Families can find support through networks, counseling, and resources. It’s important to talk openly with doctors and to discuss the prognosis with the child.
What are the future directions in neuroblastoma treatment and outcomes?
New clinical trials and precision medicine are promising. They aim to improve long-term survival rates. Advances in immunotherapy and targeted treatments could lead to better outcomes.
What does remission mean in neuroblastoma, and what are the recurrence rates?
Remission means no detectable disease. Complete remission means no signs of disease, while partial remission means a big reduction. Recurrence rates vary by risk group, with higher risk groups facing higher rates.
How does MYCN amplification affect neuroblastoma prognosis?
MYCN amplification means the disease is more aggressive and has a worse prognosis. It’s a key factor in determining the risk level and treatment intensity.
What is the role of immunotherapy in neuroblastoma treatment?
Immunotherapy, like anti-GD2 therapy, is now a standard part of treatment for high-risk neuroblastoma. It targets neuroblastoma cells and has improved survival rates.
References
- National Cancer Institute. (2025). Neuroblastoma treatment (PDQ®). https://www.ncbi.nlm.nih.gov/books/NBK65747/